Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista Brasileira de Odontologia
versão On-line ISSN 1984-3747versão impressa ISSN 0034-7272
Rev. Bras. Odontol. vol.73 no.3 Rio de Janeiro Jul./Set. 2016
SHORT COMMUNICATION/PEDIATRIC DENTISTRY
Management of late dental trauma healing complications in primary teeth: a case report of 3 years follow-up
Nashalie Andrade de AlencarI; Tatiana Kelly da Silva FidalgoII; Jacckeline BarrosIII; Maria da Encarnação P. Requejo da CostaI; Lucianne Cople MaiaI
I Department of Pediatric Dentistry and Orthodontics, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
II Departament of Clinics, School of Dentistry, Salgado de Oliveira University, Niterói, Rio de Janeiro, Brazil
III Department of Clinics, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
ABSTRACT
Objective: This case reports the management of late healing complications in primary teeth after dental trauma. Case Report: A 6-year-old girl was referred to the pediatric dentistry clinic with a huge swelling associated with her anterior maxillary left-side region as a main complaint. Her mother reported a traumatic injury in the affected tooth one year before. The clinical exam revealed a noncomplicated fracture and an extensive abscess, both radiographically associated with the left maxillary central incisor. Additionally, pulp obliteration in its homologous tooth was observed. The abscessed tooth was extracted and the homologous tooth was maintained, the child was followed up for three years. No crown or root pathological alterations were observed in either erupted permanent successors. Conclusion: Traumatic injury in the primary teeth may show no initial healing complication however, the follow up and treatment of acute healing complications is essential until the eruption of the permanent tooth.
Keywords: Dental trauma; Children; Pulp obliteration; Clinical management; Abcess.
Introduction
Injuries to primary dentition are among the most common traumas that occur in the maxillofacial region.1 Preschool children experience at least one injury to their primary teeth.1,2 In the early years of life, the most common trauma cause related by children's parents or guardians is a fall from the child's own height.3
Healing complications of trauma are usually described in primary teeth,1,3 and the most common pulpal healing complication is calcification followed by obliteration of the pulp of the injured tooth.1 Pulp degeneration followed by necrosis is not always easy to diagnose early in primary teeth.3 However, its consequences can lead to acute clinical situations.
Furthermore, complications with the unerupted permanent teeth are frequently associated with trauma to their predecessors and usually depend on the developmental stage of permanent buds and their close relationship with the apex of the primary tooth at the moment of trauma occurrence.1 They also depend on the severity and direction of the trauma.1
The treatment for traumatic injuries to primary teeth should always take into account the possibility of damage to permanent successor. The Internacional Association for Dental Traumatology define uncomplicated crown fracture as an enamel fracture or an enamel-dentin fracture that does not involve the pulp. The proposed treatment objectives to maintain the pulp vitality and restore esthetics and function. The prognosis depends on the concomitant injury to the periodontal ligament and on the extent of dentin exposed. It is recommended 3-4 weeks clinical follow-up.4,5
Also, when it is possible to prioritize a minimal intervention in order to maximize the chances of success on the development of the permanent teeth, this is the best approach.1 However, in some cases, minimal intervention is not justified, once its benefits cannot be higher than the risk of damage to the permanent tooth in development or to the child's health. In such cases, tooth extraction is required, and the follow-up is crucial to treatment success. Thus, the aim of this report is to present a dental approach to two different late healing complications after traumatic dental injury in primary teeth.
Case report
A 6-year-old girl was referred to the department of orthodontics and pediatric dentistry of a public university in Rio de Janeiro with a main complaint of a huge swelling in the anterior maxillary left-side region. There was a noncontributory medical history. The child had no systemic commitment and did not use any controlled medication. According to her mother, the patient had fallen from her own height, one year before. Since there were no signals and symptoms observed before, nothing was done at the time of the trauma, no treatment was sought. The child's mother signed a consent form before the treatment.
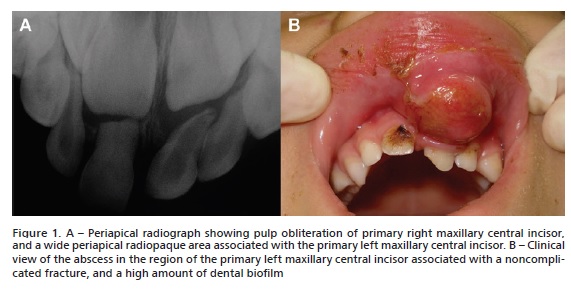
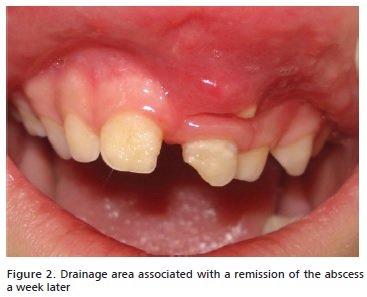
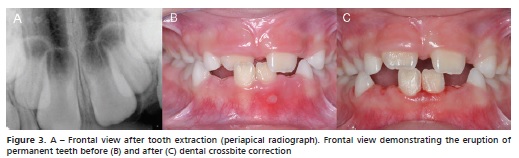
Clinical examination revealed a labial edema associated with an abscess in a palatal displaced left maxillary central incisor with a noncomplicated fracture and with high mobility. In addition, a high dental biofilm accumulation on the homologous tooth was presented. A posterior crossbite was also seen. A radiograph examination revealed a radiolucid area suggestive of a periapical lesion on the primary left incisor. Additionally, pulp obliteration on the primary right incisor was radiographically observed (Figures 1A, 1B). Antibiotics, Amoxicillin 250mg/5mL for 7 days, was prescribed to control the infection, since the child has no allergies or medication restriction. In addition, oral hygiene and diet instructions was recommended. A week later, the abscess had decreased (figure 2) and the left maxillary incisor was extracted with security, since there was a huge initial infection that could be disseminated. The tooth was not restored at the first appointment because a week later it will be extracted. The extraction was done to avoid damages to the permanent successor since the tooth had high mobility and radiolucent area on radiographic exam. The right central incisor was managed with a minimally invasive approach and was maintained in its position (figure 3A) until its physiological exfoliation. After the urgent situation had been resolved, the posterior crossbite was treated.
For an ideal treatment the follow up should be done regularly and cared.5 The child was examined every 3 months, and during the first year follow-up consultation, the eruption of the permanent maxillary central incisors was observed without any pathological alterations. However the right central incisor erupted in a crossbite position (figure 3B), and was promptly orthodontically repositioned (figure 3C).
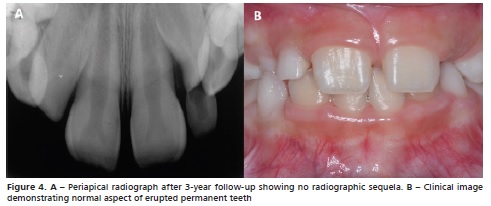
After 3 years of follow-up, it was possible to see the complete eruption of the permanent maxillary central incisors, in a perfect clinical and radiographic way. No healing complications were observed in the permanent teeth (figure 4).
Discussion
Studies have reported that the maxillary central incisors are the most frequently injured teeth in primary dentition. The upper central incisors are generally more prone to dental trauma than the lower central incisors and tend to be the first to receive a direct blow.6,7
Many histopathological reactions may appear due to a trauma in primary dentition; among them we can have a crown discoloration, a pulp canal obliteration, a pathological root resorption or a pulp necrosis.3 Calcified structures and obliterations frequently occur in both primary and permanent teeth that have been directly traumatized, since pulp tissue is able to form calcified structures as a result of traumatic force.8 Also, a pulp necrosis can happen, and the presence of a sinus tract or the noting of an enlarged radiographic periodontal ligament may suggest that a tooth has been traumatized.3,9 In the present case, the same trauma resulted in two different healing complications in traumatized teeth. At the same time, a silent complication in the primary right central incisor in the form of a pulp canal obliteration and an acute abscess in the primary left central incisor were observed. The development of these distinct complications is probably related to some factors such as the kind of trauma and applied forces at the moment of its occurrence, which must be different for each tooth, as well as the own response of each tooth to their own trauma.10
Pulpal necrosis can occur at any time following a traumatic dental injury, and often it occurs asymptomatically,9 and may result in an abscess. As described in the present case, pulpal necrosis was diagnosed only after one year of dental trauma, and during this period the child never complained of pain. Her mother only realized that there was something wrong because of the huge size of the presented lesion. As mentioned in this case report, the lesion size was the trigger for the search for attention.
The damage to the permanent tooth by the injured primary tooth depends on the intensity of force exerted, the direction of force and the degree of hard tissue development of the permanent tooth.9,10 Injuries occurring to primary incisors that are near exfoliation are far less likely to cause significant damage to the permanent tooth since the enamel of the permanent crown is already formed,9 as observed in the current case report. Therefore, the earlier the injury occurs to the primary incisors, the greater the chance that the permanent tooth is affected.9
Traumatized primary incisors frequently cause ectopic eruption of the permanent incisors.9 In some cases, necrosis can displace the eruption of a permanent tooth or the displacing force may redirect the eruption pattern of the permanent tooth,9 which was not observed in the present report, since the presence of an abscess was not able to cause bud deflection or eruption problems. On the other hand, the right permanent central incisor erupted in a crossbite position, probably due to the dental trauma on its predecessor.
Although minimal intervention is the best treatment choice for traumatized temporary teeth,2 it was not fully performed in the present case, since the presence of an abscess indicated a risk of permanent bud damage, and also a risk to the child's health.
Conclusion
An injury to a young child's teeth may show no initial healing complication, however it is crucial to educate parents about the importance of seeking a pediatric dentist in cases of trauma in primary dentition, because late healing complications may occur. In addition, it can be observed that it is possible to have different types of sequelae over time, depending on the severity and direction of the trauma. The dentist must take time to examine and analyze the possibilities of damage to the primary teeth, and also to the permanent tooth.
References
1. Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J Oral Surg. 1972;1(5):235-9. [ Links ]
2. Fidalgo TK, Maia LC. Minimally invasive intervention of acute trauma in the primary dentition: successful five-year follow-up. Gen Dent. 2012;60(3):e158-61.
3. Tannure PN, Fidalgo TK, Barcelos R, Primo LG, Maia LC. Analysis of root canal treated primary incisor after trauma: two-year outcomes. J Clin Pediatr Dent. 2012;36(3):257-62.
4. IADT. Internacional Association for Dental Traumatology. 2014. Available from:www.dentaltraumaguide.org/Primary_enameldentin_fracture_ Treatment.aspx
5. AAPD. American Academy of Pediatric Dentistry. Guideline on Man- Referências :: agement of acute dental trauma. Clinical Guidelines. 2010;32(6):202-12.
6. Oliveira LB, Marcenes W, Ardenghi TM, Sheiham A, Bonecker M. Traumatic dental injuries and associated factors among Brazilian preschool children. Dent Traumatol. 2007;23(2):76-81.
7. Skaare AB, Jacobsen I. Primary tooth injuries in Norwegian children (1-8 years). Dent Traumatol. 2005;21(6):315-9.
8. Katz-Sagi H, Moskovitz M, Moshonov J, Holan G. Pulp canal obliteration in an unerupted permanent incisor following trauma to its primary predecessor: a case report. Dent Traumatol. 2004;20(3):181-3.
9. Haney KL. Trauma to the primary dentition. J Okla Dent Assoc. 2007;99(2):42-4.
10. McTigue DJ. Managing injuries to the primary dentition. Dent Clin North Am. 2009;53(4):627-38.
 Endereço para correspondência:
Endereço para correspondência:
Lucianne Cople Maia
e-mail: rorefa@terra.com.br
Submitted: 05/24/2016
Accepted: 07/10/2016













