Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.20 no.39 Canoas Jul./Dez. 2014
Computed tomography imaging features of multicystic granular cell ameloblastoma: a case report
Aspectos tomográficos de ameloblastoma multicístico de células granulares: relato de caso
Gabriella Lopes de Rezende Barbosa I; Matheus Lima Oliveira II; Luís Antônio Nogueira dos Santos III; Solange Maria de Almeida IV
I MSc degree and is a PhD candidate in Oral Radiology at the Department of Oral Diagnosis, Area of Dental Radiology, Piracicaba Dental School, University of Campinas (UNICAMP), Piracicaba, SP, Brazil
II MSc and a PhD in Oral Radiology, and a postdoctoral fellow in Dental Radiology at the Department of Oral Diagnosis, Area of Oral Radiology, Piracicaba Dental School, UNICAMP, Piracicaba, SP, Brazil
III MSc in Dentistry (Stomatology) and a PhD in Oral Radiology from the Department of Oral Diagnosis, Area of Oral Radiology, Piracicaba Dental School, UNICAMP, Piracicaba, SP, Brazil
IV MSc and a PhD in Dental Radiology from the Department of Oral Diagnosis, Area of Oral Radiology, Piracicaba Dental School, UNICAMP, Piracicaba, SP, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
Multicystic ameloblastoma is a clinical variant of ameloblastoma. It is often locally aggressive with significant impact on patient morbidity and mortality. Ameloblastoma is often asymptomatic and is usually detected as an incidental finding during routine dental examinations. It presents slow and persistent growth; in some cases a gradual expansion of the jaw producing facial asymmetry may be noticed . Although the occurrence is rare, ameloblastomas can exhibit malignant behavior and metastasize. Clinical evaluation includes careful review of the patient's medical history and physical examination of the head and neck region. Radiographic imaging techniques are useful for locating the lesion, estimating its dimensions and assessing its effects on adjacent structures. Management of ameloblastoma is a challenge for all involved in the field of head and neck surgery. The aim of this paper was therefore to describe the tomographic features of a multicystic granular cell ameloblastoma in a 40-year-old white male patient.
Keywords: Ameloblastoma, Granular Cell Tumor, X-Ray Computed Tomography, Dental Radiography.
RESUMO
O ameloblastoma multicístico é uma variante clínica do ameloblastoma, muitas vezes localmente agressivo, com significante aumento de morbidade e mortalidade. O ameloblastoma é frequentemente assintomático, sendo identificado incidentalmente durante exames odontológicos de rotina. Trata-se de uma lesão de crescimento lento e persistente, podendo ser notada, em alguns casos, uma expansão gradual da mandíbula, produzindo assimetria facial. Ameloblastomas raramente apresentam um comportamento maligno. A avaliação clínica inclui uma revisão cuidadosa da história clínica do paciente, bem como exame físico da cabeça e pescoço. Modalidades de imagens radiográficas são úteis para localizar a lesão, avaliar suas dimensões e os efeitos sobre as estruturas adjacentes. O manejo da lesão representa um desafio para todos os profissionais envolvidos na área de cirurgia de cabeça e pescoço. Assim, o objetivo deste trabalho foi descrever as características tomográficas de um ameloblastoma multicístico de células granulares em um paciente do sexo masculino, leucoderma, de 40 anos de idade.
Palavras-chave: Ameloblastoma, Tumor de Células Granulares, Tomografia Computadorizada por Raios X, Radiografia Dentária.
INTRODUCTION
Ameloblastoma is a rare odontogenic tumor of the jaws that originates from the epithelium involved in teeth formation: enamel organ, odontogenic rests of Malassez, reduced enamel epithelium and odontogenic cyst lining 1,2. This a locally aggressive tumor that accounts for about 10% of odontogenic tumors 3 and 1% of all oral cancers 4. It is often asymptomatic and so discovered in routine radiographs, but swelling and expansion of the jaws are also common clinical manifestations 5. Radiographically, ameloblastomas are osteolytic, typically found in the tooth-bearing areas of the jaws, and may be either unilocular or multilocular. Radiographic margins are usually well defined and sclerotic, because ameloblastoma grows slowly and persistently 6.
Three types of ameloblastomas can be distinguished, mainly on the basis of clinical behavior and prognosis, as follows: multicystic, unicystic or peripheral 7. The multicystic type (also known as intraosseous or solid ameloblastoma) appears as multilocular or "soap bubble" radiolucencies. Unicystic ameloblastomas appear on radiography as unilocular radiolucent lesions and are often associated with an impacted tooth. Peripheral ameloblastomas occur in the gingiva and there is no bone involvement or radiographic features.
Clinical evaluation includes careful review of the patient's medical history and physical examination of the head and neck. Imaging work includes both panoramic radiography and computed tomography (CT) 8. Panoramic images provide an overview of the dental arches and a close view of a large number of anatomical structures with low doses of radiation. In turn, CT is helpful when planning the surgery because it shows the entire tumor volume and the tumor's relationships to surrounding structures, including soft tissue 9. Management of ameloblastoma poses a challenge for all involved in the field of head and neck surgery. Successful treatment requires not only adequate resection of the tumor but also reconstruction of the residual defect that is both functional and aesthetically acceptable 1,10. The aim of this paper is to describe the tomographic aspects of a multicystic granular cell ameloblastoma.
CASE REPORT
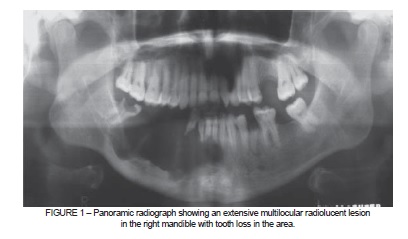
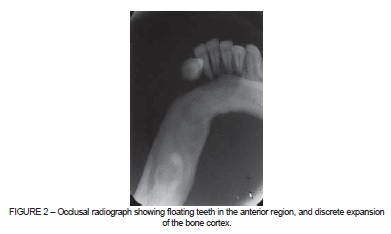
A 40-year-old white male patient was seen at the radiology clinic for evaluation of an asymptomatic swelling on the right side of the lower face. Panoramic radiograph showed radiolucency from the lower right third molar to the left central incisor (Figure 1). Inferiorly, bone resorption extended to the inner cortex of the lower margin of the mandible. A multilocular area with undulating borders and bony septa was identified. The location of the mandibular canal could not be determined. The Lower right premolars, first molar and second molar were missing. The lower central incisors and the right lateral incisor and canine exhibited external root resorption. Occlusal radiography showed minimal expansion of the bone cortex (Figure 2). Incisional biopsy findings suggested a diagnosis of granular cell ameloblastoma.
A helical CT scan (Philips Aura CT Scanner, Amsterdam, The Netherlands) was taken at 120 kV and 100 mA for surgical planning. Iohexol iodine based-contrast (Omnipaque 300; SanofiWinthrop; Markham, Ontario, Canada) was injected intravenously for evaluation of soft tissue involvement. Multiplanar images were reconstructed with 1-mm-thick axial slices, a 0.5mm reconstruction interval and a matrix size of 512 x 512 (Figure 3 and 4). The three-dimensional reconstruction provided better definition of the limits of the lesion and improved understanding of the relationships between the structures involved.
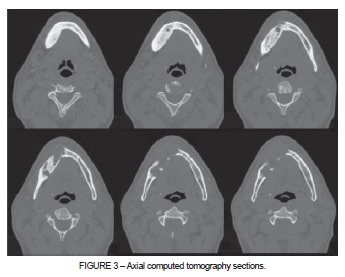
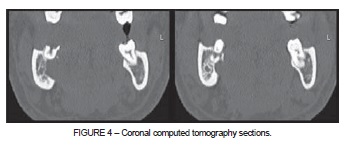
Features seen on CT imaging included a destructive lesion causing hyperostosis of the lower border of the mandible, with mutiloculated hypodense areas, and destruction of the buccal and lingual cortical plate. The buccal cortical plate was expanded and perforated. Soft-tissue involvement was not seen, since the lesion did not absorb contrast media. In coronal sections, we observed that the lesion extended to the distal root of the lower right third molar, adjacent to the lingual cortical plate.
DISCUSSION
Ameloblastoma is an epithelial odontogenic tumor with locally aggressive behavior and a high recurrence rate. It most often occurs in the lower molar region, and the mandible is affected five times more frequently than the maxilla 11. A study reporting on 60 cases of ameloblastoma showed that 69% arose in the angle of the mandible, 23% in the body of the mandible, and 8% in the symphyseal and parasymphyseal regions 12. In the present case, the lesion center was located on the right side of the mandibular body and extended from the midline to the lower right third molar. It has been reported that the mean age of patients with ameloblastoma is 36 with a range of 4-92 years. Our study is in line with these data, since the patient was a 40-year-old. In developing countries, ameloblastoma occurs in younger patients with equal sex distribution 11.
Although ameloblastoma has been described as an uncommon lesion in the scientific literature 1, one study in Sri Lanka analyzed 1677 cases of odontogenic tumors and found an occurrence of 48.7%. Furthermore, the multicystic type was the most common of the three types, with an occurrence of 63.7% 13. In a study investigating 340 Brazilian patients treated for odontogenic tumors between 1954 and 2004, there were 45.3% cases of ameloblastoma and 0.3% cases of ameloblastic carcinoma 14.
The radiographic and tomographic features of our case were fully compatible with multicystic ameloblastoma, which predominantly presents with one of two histological patterns: follicular or plexiform. Other histological variants include acanthomatous, desmoplastic, basal cell and granular cell 5. In this case, histological analysis revealed granular cell ameloblastoma, a variant first reported in 1918 by Krompecher 15. The current literature includes few reported cases of granular cell ameloblastoma, some of which eventually produced metastasis. Granular cell change is a rare histopathological entity 16, and the question of whether the presence of these cells is a degenerative process or is prognostic of an aggressive clinical course is still under discussion 17.
Rarely, ameloblastomas may exhibit malignant behavior including hematogeneous dissemination and can then be classified as metastasizing ameloblastomas or the more aggressive ameloblastic carcinomas. If an unlikely event such as pulmonary metastasis occurs, a chest radiograph should be considered 18. A number of different treatment approaches to ameloblastomas exist. Conservative surgical treatment includes enucleation, curettage, electrocauterization, excision and marsupialisation. Radical surgery depends on the tumor's histological and clinical presentation and includes marginal, segmental or total resection of the involved jaw with wide margins 2,12. Multicystic ameloblastoma has a high recurrence rate following simple enucleation (60- 80%) 19. Surgical resection of ameloblastoma with safe margins is the best primary method for treating multicystic ameloblastomas to avoid recurrence 20.
FINAL CONSIDERATIONS
We have reported a case of multicystic granular cell ameloblastoma of the mandible in a 40-year-old male patient. Conventional radiographs were useful for detecting the lesion and giving an idea of its dimensions. CT provided reliable information about the location, shape, periphery and internal appearance of the Multicystic Ameloblastoma and its effects on surrounding structures. This imaging technique is a very good aid for establishing diagnosis and planning treatment and follow-up.
REFERENCES
1. Sham E, Leong J, Maher R, Schenberg M, Leung M, Mansour AK. Mandibular ameloblastoma: clinical experience and literature review. ANZ J Surg. 2009;79:739-44. [ Links ]
2. Paikkatt VJ, Sreedharan S, Kannan VP. Unicystic ameloblastoma of the maxilla: a case report. J Indian Soc Pedod Prev Dent. 2007;25:106-10.
3. Scholl RJ, Kellett HM, Neumann DP, Lurie AG. Cysts and cystic lesions of the mandible: clinical and radiologic-histopathologic review. Radiographics. 1999;19:1107-24.
4. Bataineh AB. Effect of preservation of the interior and posterior borders on recurrence of ameloblastomas of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:155-63.
5. Neville BW, Damm DD, Allen C, Bouquot JE. Oral & maxillofacial pathology. 2nd ed. Philadelphia: Saunders; 2002. 6. Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology: clinical pathologic correlations. 5th ed. Philadelphia: Saunders/Elsevier; 2008.
7. Philipsen HP, Reichart PA. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral Oncol. 1998;34:317-25.
8. Zemann W, Feichtinger M, Kowatsch E, Kärcher H. Extensive ameloblastoma of the jaws: surgical management and immediate reconstruction using microvascular fl aps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:190-6.
9. Black CC, Addante RR, Mohila CA. Intraosseous ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:585-92.
10. Ooi A, Feng J, Tan HK, Ong YS. Primary treatment of mandibular ameloblastoma with segmental resection and free fibula reconstruction: achieving satisfactory outcomes with low implant-prosthetic rehabilitation uptake. J Plast Reconstr Aesthet Surg. 2014;67:498-505.
11. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86-99.
12. Becelli R, Carboni A, Cerulli G, Perugini M, Iannetti G. Mandibular ameloblastoma: analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofac Surg. 2002;13:395-400.
13. Siriwardena BS, Tennakoon TM, Tilakaratne WM. Relative frequency of odontogenic tumors in Sri Lanka: analysis of 1677 cases. Pathol Res Pract. 2012;208:225-30.
14. Fernandes AM, Duarte EC, Pimenta FJ, Souza LN, Santos VR, Mesquita RA, et al. Odontogenic tumors: a study of 340 cases in a Brazilian population. J Oral Pathol Med. 2005;34:583-7.
15. Krompecher E. The histogenesis and morphology of adamantinomas and other jaw tumors. Beitr Patol Anat. 1918;64:165-97.
16. Yamunadevi A, Madhushankari GS, Selvamani M, Basandi PS, Yoithapprabhunath TR, Ganapathy N. Granularity in granular cell ameloblastoma. J Pharm Bioallied Sci. 2014;6:S16-20.
17. Bansal A, Bhatnagar A, Saxena S. Metastasizing granular cell ameloblastoma. J Oral Maxillofac Pathol. 2012;16:122-4.
18. Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Ameloblastoma. Am J Clin Oncol. 2007;30:645-8.
19. Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg. 2009;38:807-12.
20. Adeyemo WL, Bamgbose BO, Ladeinde AL, Ogunlewe MO. Surgical management of ameloblastomas: conservative or radical approach? A critical review of the literature. Oral Surgery. 2008;1:22-7.
 Correspondence:
Correspondence:
Gabriella Lopes de Rezende Barbosa
Department of Oral Diagnosis, Area of Oral Radiology, Piracicaba Dental School
University of Campinas – UNICAMP
Av. Limeira, 901, CEP 13414-903
Piracicaba, SP, Brazil
E-mail: gabriellalopes@live.com













