Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.2 Piracicaba Abr./Jun. 2012
ORIGINAL ARTICLE
Oral and maxillofacial surgery - Helmet and maxillofacial trauma: a 10-year retrospective study
Maximiana Cristina de Souza MaliskaI; Marcia BorbaII; Luciana AsprinoIII; Márcio de MoraesIV; Roger Willian Fernandes MoreiraIII
IDDS, Master student of Oral and Maxillofacial Surgery, Department of Oral Diagnosis, Oral and Maxillofacial Surgery Division, Piracicaba Dental School, University of Campinas, Brazil
IIDDS, MS, PhD, Collaborative Researcher, Department of Oral Diagnosis, Oral and Maxillofacial Surgery Division, Piracicaba Dental School, University of Campinas, Brazil
IIIDDS, MS, PhD, Associate Professor, Department of Oral Diagnosis, Oral and Maxillofacial Surgery Division, Piracicaba Dental School, University of Campinas, Brazil
IVDDS, MS, PhD, Associated Professor and Coordinator of the Postgraduate Program in Oral and Maxillofacial Surgery, Department of Oral Diagnosis, Oral and Maxillofacial Surgery Division, Piracicaba Dental School, University of Campinas, Brazil
ABSTRACT
AIM: The aim of the present study was to retrospectively evaluate the epidemiologic characteristics of the prevalence, type and treatment modalities of maxillofacial trauma according to use of helmets by motorcyclists in traffic accidents.
METHODS: Data was collected from patients during a 10-year period (1999-2009). Data recorded included demographic, etiology, diagnosis, type of fracture, use of helmet, associated facial and general trauma, soft tissue lesions and treatment methods. Data analysis included a descriptive analysis, Chi-square test and Kruskal-Wallis test.
RESULTS: From 376 motorcycle crash victims, 260 had maxillofacial fractures with a male/female ratio of 4:1 and a mean age of 26.1. Considering the helmet as a security device, 89 patients were not wearing a helmet during the crash against 287 patients that were wearing it. One hundred and sixteen patients had soft tissue lesions, 80 of them wore a helmet at the moment of the crash and 36 did not (p<0.05). The most frequently fractured facial bone was the zygoma (24%) followed by the mandible.
CONCLUSIONS: Motorcycle accidents represented almost one third of all maxillofacial injuries seen at this Oral and Maxillofacial Surgery Division, causing high morbidity. Educational campaigns, defensive driving and use of adequate helmets are necessary to decrease the number of facial injuries in such accidents.
Keywords: maxillofacial injuries, epidemiology, motorcycles.
Introduction
Motorcycle injuries continue to be a major public health problem worldwide, especially in developing countries. These accidents increase dramatically the health costs involved in treatment and rehabilitation of the injured patients, and have interrupted the life of thousands of people, especially in the economically active age range (adolescents and young adults)1.
If motorcyclists are wearing a helmet at the time of the accident, their risk of death is reduced by 42%, while nonhelmeted riders have a 3.1 fold increased risk of head injuries and death2-3 .
Research has also shown the effectiveness of laws requiring the use of helmets by two wheel motor vehicle occupants for the reduction of fatalities and injuries in this user category4-5. With the changes in the Brazilian traffic code issued in 1998, security devices were made mandatory, alcohol abuse was forbidden, and driving without a license or under the age of 18 became serious offenses6.
Although the impact of helmet use on the reduction of head injuries during motorcycle accidents is well known, the effect of their use on facial injuries is not well documented7-8.
The purpose of this study was to review retrospectively the first 10 years after the new traffic law in Brazil. The patterns of the maxillofacial trauma in motorcycle accidents relating the use of helmets were evaluated and discussed.
Material and methods
This 10-year retrospectively study was undertaken by the Graduate Oral and Maxillofacial Surgery Division, University of Campinas - UNICAMP at 7 hospitals located in the cities of Piracicaba, Limeira and Rio Claro, São Paulo state. The research protocol was approved by the Human Research Ethics Committee from the same institution, under the protocol number 131/2008.
Information was obtained from clinical notes and surgical records for each patient using a standardized data collection form that was specifically developed to investigate the epidemiologic features of maxillofacial trauma. The data recorded only patients sustaining maxillofacial injuries after motorcycle accidents. It included patient age, gender, diagnosis, use of helmet, soft tissue lesions, associated facial and general trauma and type of treatment. The exclusion criteria were incomplete information on the trauma in the medical chart.
The injury sites were classified into three thirds of the face: upper (frontal bone), middle (maxilla, zygoma, zygomatic arch naso-orbit-ethmoidal, nasal) and inferior (mandible). Mandible fractures were divided into specific sites: condyle, ramus, angle, body, parasynphysis, synphysis and dentoalveolar. Abrasion and laceration were classified as soft tissue injuries.
Data were entered into Microsoft Excel software. Simple descriptive statistical, chi-square test and Kruskal-Wallis test were applied as appropriate. Statistical significance was inferred at p<0.05.
Results
A total of 2,785 trauma patients were evaluated from April 1, 1999, to December 31, 2009. Of these patients, 772 were traffic accidents victims, 376 were motorcycle crash victims with maxillofacial trauma, and 260 had maxillofacial fractures. Of the 376 patients with maxillofacial trauma, 307 were males and 69 females, with male/female ratio of 4:1.
Patient age at the time of injury was 10 to 65 years (mean 26.1 years). Among the total of 376 patients, 29 (8%) were 10 to 17 years old, 257 (68%) were in the 18-30-yearold age group (being 211 males and 46 females), 83 (22%) were 31 to 50 years old, and 7 (2%) were older than 50 years. The Kruskal-Wallis test did not show a statistically significant association between age groups and use of helmet (p=0.103). Table 1 describes absolute and relative distribution of maxillofacial trauma according to age and gender groups correlating the use of helmet.
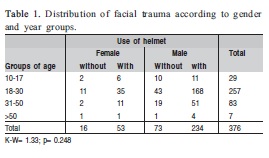
Considering the helmet as a security device, 89 patients were not wearing a helmet at the moment of the crash, against 287 patients that were wearing, of which 234 were males. The chi-square test did not show a statistically significant association between gender and wearing security device.
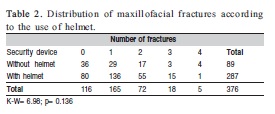
Of the 287 patients that were wearing helmets, 136 suffered maxillofacial fracture and 80 did not have any facial bone fractured (Table 2). Four patients had 4 different fractures even wearing helmet, against 1 patient that was not wearing a security device. The Kruskal-Wallis test did not show a statistically significant association between number of fractures and wearing security device (p=0.136).
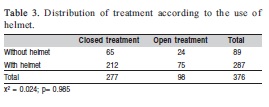
Patients that wearing helmets (212), were treated conservatively, while 75 patients had open treatment. Of the 89 patients that were not wearing a security device, 65 had closed treatment and 24 had open treatment (Table 3). The x² test did not show a statistically significant difference between types of treatment and wearing a security device (p=0.985).
Facial fractures were observed in 260 patients and 116 had soft tissue lesions that include laceration, abrasion andhematoma. Of the patients with these lesions, 80 wore helmets at the moment of the crash and 36 did not. Patients that were wearing a helmet and had fractures account to 207 against 53 that did not. The chi-square test showed a statistically significant difference between type of trauma and wearing security device (p<0.05).
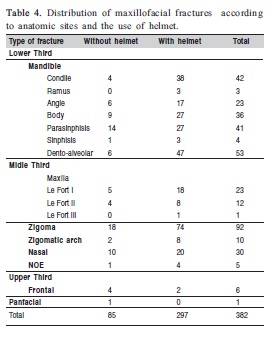
A tota of 382 different types of fractures were found in these 260 patients. The zygoma was the most frequently fractured bone (24%), followed by the mandible: dentoalveolar trauma (14%), condyle and parasynphysis (11%). One one case of panfacial trauma was observed and this patient was not wearing helmet (Table 4).
Overall trauma evaluation revealed 239 patients with concomitant corporeal lesions. Encephalic trauma (260 patients), chest trauma (254) and upper members (164) were not found in patients that were wearing helmet, as seen in Table 5. The chi-square test showed statistically significant association between associated trauma and wearing security device.

Discussion
In developing countries, traffic deaths are projected to be the third most important health problem by 2020, and a large proportion of these deaths involve motorcycles9. Motorcycles are particularly dangerous vehicles. Motorcycle riders are at an increased risk of accident because the small size of the motorcycle makes them more prone than automobile drivers to experience serious injuries10. Assuming that a motorcyclist attains a riding license at the age of 17 and rides 13,500 km per year until retirement lifetime, the risk of death or serious injury approaches 100%11. It is clear that the use of helmets decreases the severity of injury and the probability of deaths, reducing health care costs12-14.
The population evaluated in this retrospective study, 849,269 inhabitants from the cities of Limeira, Piracicaba and Rio Claro, Brazil, is young, has great mobility, lives in urban areas and is economically active. In a 7-year period, the number of inhabitant per motorcycle had a great increase in these three cities, in 2002 there were 14.24 inhabitants per motorcycle and this number in 2009 doubled to 7.52 inhabitants per motorcycle15. The users affirm that motorcycles are affordable, fuel-efficient, have cheaper maintenance than a car and facilitate locomotion in the overcrowding traffic, characteristics of the São Paulo state.
The results of this study demonstrated that motorcycle accidents are common among young male patients. Gopalakrishna et al.13 reported a prevalence of maxillofacial injury in males (89.7%) with a mean age of 28.7 years. According to Oginni et al.16, the male-female ratio was 3.5:1, the peak age incidence for males was 20 to 29 years, whereas female had a peak age incidence of 10 to 19 years in motorcycles accidents. In accordance with the present study, other Brazilians studies investigated the prevalence of young males involved in two wheel vehicle accidents17-18. Ourresults are similar tose of other studies worldwide, representing similar behavior of motorcyclists in different countries, as discussed herein.
Motorcyclists are in disadvantage against car drivers when the collision occurs because this two wheel vehicle do not offer a security device like a seat belt or an air bag, that keeps the body of the patient inside the car. The pillions often are heedless far from the motorcycle and the only device that can prevent a worst injury in the head or face is the helmet. Helmeted riders have been shown to have 70% reduction in injury severity and 40% reduction in mortality compared to unhelmeted riders in collisions19.
Ten years after the introduction of the new traffic code in Brazil, helmeted motorcyclists represents 76.3% of all patients involved in motorcycle accidents against 31.2% of patients before the introduction of the new law, as demonstrated by Liberatti et al. in a study of the Brazilian population20. Ferrando et al.5 analyzed the mortality rate before and after law changes in Spain and found a 25% reduction of fatal accidents among two wheel vehicle occupants, with a reduced incidence of head trauma. Another study that assessed motorcycle and maxillofacial trauma among Nigerian intracity road users16 reached different results, as none of the riders or passengers used a helmet at the time of the road accident, and soft tissue lesions were prevalent among facial injuries.
The number of motorcyclists presenting maxillofacial fractures using helmets in this study was higher than motorcyclists using helmets that sustained facial contusions. As motorcycle crashes are high-energy trauma, it is possible that the impact of the cranium and face during the accident in patients without helmet promote more seriously injury, as immediate death or severe encephalic traumatism.
The incidence of associated body traumatism with maxillofacial fractures can vary widely. This study presented a large number of concomitant traumas in patients that were wearing helmets during the crash. This could be explained by the inexistence of a security device that protects the whole body of motorcyclists. Another factor that can influence this result would be the increase of riders that were using helmets.
Brasileiro and Passeri21 demonstrated a prevalence of 24.1% in upper limbs associated trauma, this data corroborates with this study. Ramli et al.22 affirm that the use of helmet during an accident reduces the incidence of skull injures while the motorcyclist becomes more susceptible to thoracic and orthopedic trauma. Alvi et al.23 disagree with this study, concluding that encephalic trauma is commonly associated with facial trauma ranging from 5.4 to 85%.
Gopalakrishna et al.13 observed that the incidence of mandibular fractures is significantly higher for motorcyclists wearing helmets than for those who do not. The data presented in this study and in the national studies by Maliska et al.24 and Scariot et al.25 agree with this statement. The prominence of the mandible and the dissipation of impact forces along the architectural framework of the middle third can explain this prevalence of fractures. The data collected in this work did not account the deaths, neither the patients that did not have maxillofacial trauma, considering only the patients that survived for oral and maxillofacial specific examination. Further studies must be developed to include these data, probably collected at hospital emergency rooms.
High-energy trauma caused by motorcyclists is responsible for higher percentages of soft tissue lacerations and facial fractures. Motorcycle accidents represented almost one third of all maxillofacial injuries seen in this division of oral and maxillofacial surgery, causing high morbidity. Educational campaigns, defensive driving and the use of adequate helmets are necessary to decrease the number of facial injuries in such accidents.
Facial fractures in motorcyclists occur primarily among men under 30 years of age in the studied population and the majority of patients sustaining maxillofacial fractures wore helmets at the moment of the crash. Overall, the most common fractured sites on the face are the zygomatic complex followed by the mandible. Patients that wore helmets had more conservative treatments, and encephalic trauma is related with the use of helmet. Young adults are more severely injured and are more frequently involved in accidents.
References
1. Salvarani CP, Colli BO, Carlotti Júnior CG. Impact of a program for the prevention of traffic accidents in a Southern Brazilian city: a model for implementation in a developing country. Surg Neurol. 2009; 72: 6-14. [ Links ]
2. Liu BC, Ivers R, Norton R, Boufous S, Blows S, Lo SK. Helmets for preventing injury in motorcycle riders. Cochrane Database Syst Rev. 2008; 23(1): CD004333. [ Links ]
3. Lin MR, Kraus JF. A review of risk factors and patterns of motorcycle injuries. Accid Anal Prev. 2009; 41: 710-22. [ Links ]
4. Derrick AJ, Faucher LD. Motorcycle helmets and rider safety: a legislative crisis. J Public Health Policy. 2009; 30: 226-42. [ Links ]
5. Ferrando J, Plasència A, Orós M, Borrell C, Kraus JF. Impact of a helmet law on two wheel motor vehicle crash mortality in a southern European urban area. Inj Prev. 2000; 6: 184-8. [ Links ]
6. Queiroz MS, Oliveira PC. Traffic accidents: a qualitative approach from Campinas, São Paulo, Brazil. Cad Saude Publica. 2002; 18: 1179-87. [ Links ]
7. Shapiro AJ, Johnson RM, Miller SF, McCarthy MC. Facial fractures in a level I trauma centre: the importance of protective devices and alcohol abuse. Injury. 2001; 32: 353-6. [ Links ]
8. Mallikarjuna SK, Krishnappa P. Prevalence of maxillofacial injuries by motorized two wheeler road traffic accidents in Bangalore city. Dent Traumatol. 2009; 25: 599-604. [ Links ]
9. Crompton JG, Bone C, Oyetunji T, Pollack KM, Bolorunduro O, Villegas C, et al. Motorcycle helmets associated with lower risk of cervical spine injury: debunking the myth. J Am Coll Surg. 2011; 212: 295-300. [ Links ]
10. Bogerd CP, Brühwiler PA. Heat loss variations of full – face motorcycle helmets. Appl Ergon. 2009; 40: 161-4.
11. Hinds JD, Allen G, Morris CG. Trauma and motorcyclists; born to be wild, bound to be injured? Injury. 2007; 38: 1131-8. [ Links ]
12. Houston DJ. The case for universal motorcycle helmet laws. South Med J. 2010; 103: 1-2. [ Links ]
13. Gopalakrishna G, Peek-Asa C, Kraus JF. Epidemiologic features of facial injuries amongst motorcyclists. Ann Emerg Med. 1998; 32: 425-30. [ Links ]
14. Yates JM, Dickenson AJ. Helmet use and maxillofacial injuries sustained following low speed motorcycle accidents. Injury. 2002; 33: 479-83. [ Links ]
15. Fundação Sistema Estadual de Análise de Dados: State Foundation for Data Analysis of the São Paulo State – Brazil [cited 2010 Oct 22] Available from:http://www.seade.gov.br/produtos/imp/.
16. Oginni FO, Ugboko VI, Ogundipe O, Adegbehingbe BO. Motorcyclerelated maxillofacial injuries among Nigerian Iintracity road users. J Oral Maxillofac Surg. 2006; 64: 56-62. [ Links ]
17. Chcarnovic BR, Freire-Maia B, Souza LN, Abreu MHNG. Facial fractures: a 1-year retrospective study in a hospital in Belo Horizonte. Braz Oral Res. 2004; 18: 322-8. [ Links ]
18. Gomez PP, Passeri LA, Barbosa JRA. A 5-Year Retrospective Study of Zygomatico-Orbital Complex and Zygomatic Arch Fractures in Sao Paulo State, Brazil. J Oral Maxillofac Surg. 2006; 64: 63-7. [ Links ]
19. 19.World Health Organization. World report on road traffic injury prevention, 2004. [cited 2010 Apr 15] Available from: http://www.who.int/violence_injury_ prevention/publications/road_traffic/world_report/en/index.html. [ Links ]
20. Liberatti CLB, Andrade SM, Soares DA. The new Brazilian traffic code and some characteristics of victims in southern Brazil. Inj Prev. 2001; 7: 190-3. [ Links ]
21. Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102: 28-34. [ Links ]
22. Ramli R, Abdul Rahman R, Abdul Rahman N, Abdul Karim F, Krsna Rajandram R, Mohamad MS. Pattern of maxillofacial injuries in motorcyclists in Malaysia. J Craniofac Surg. 2008; 19: 316-21. [ Links ]
23. Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003; 113: 102-6. [ Links ]
24. Maliska MCS, Lima Junior SM, Gil JN. Analysis of maxillofacial fracture in the state of Santa Catarina, Brasil. Braz Oral Res. 2009; 23: 268-74. [ Links ]
25. Scariot R, de Oliveira IA, Passeri LA, Rebellato NL, Müller PR. Maxillofacial injuries in a group of Brazilian subjects under 18 years of age. J Appl Oral Sci. 2009; 17: 195-8. [ Links ]
 Correspondence:
Correspondence:
Maximiana Cristina de Souza Maliska
Faculdade de Odontologia, UNICAMP,
Av. Limeira, 901 - Areião - CEP 13414-903
CP 52, Piracicaba - SP - Brazil
E-mail: maximaliska@fop.unicamp.br
Received for publication: February 23, 2012
Accepted: May 03, 2012













