Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista Odonto Ciência (Online)
versão On-line ISSN 1980-6523
Rev. odonto ciênc. (Online) vol.25 no.3 Porto Alegre Jul./Set. 2010
CASE REPORT
Oral focal mucinosis: report of two cases
Mucinose oral focal: relato de dois casos
Madhusudhan ASI; Nagarajappa DasII; Manjunatha BSIII; Swati SaawarnI; Charan Babu HSIV
IDepartment of Oral and Maxillofacial Pathology, Pacific Dental College and Hospital, Debari, Udaipur, Rajastan State, India
IIDepartment of Oral and Maxillofacial Surgery, SJM Dental College and Hospital, Chitradurga, Karnataka State, India
IIIDepartment of Oral and Maxillofacial Pathology, KM Shah Dental College and Hospital, Pipariya, Vadodara, Gujarat State, India
IVDepartment of Oral and Maxillofacial Surgery, Pacific Dental College and Hospital, Debari, Udaipur, Rajastan State, India
ABSTRACT
PURPOSE: Oral focal mucinosis (OFM), an oral counterpart of cutaneous focal mucinosis, is a rare disease of unknown etiology. Its pathogenesis may be due to overproduction of hyaluronic acid by fibroblast at the expense of collagen production, resulting in focal myxoid degeneration of connective tissue primarily affecting the mucosa overlying bone. It has no distinctive clinical features, since the diagnosis is solely based on histopathological features. This paper reports two cases and discusses clinicopathological, immunohistochemical features and differential diagnosis of myxomatous lesions of the oral cavity.
CASE DESCRIPTION: The two cases of OFM lesions were present in a 50 year-old patient on the hard palate and in a 26 year-old female patient in the mandible, which seem to be the first report in the Indian population.
CONCLUSION: The histopathological and immunohistochemical analysis of Vimentin and S-100 protein may play a vital role in the correct diagnosis of OFM.
Key words: Oral focal mucinosis; myxomatous lesion; cutaneous focal mucinosis; hyaluronic acid; focal myxoid degeneration
RESUMO
OBJETIVO: Mucinose oral focal (MOF), uma lesão equivalente à mucinose cutânea focal, é uma doença rara de etiologia desconhecida. Sua patogênese pode ser devido a superprodução de ácido hialurônico pelo fibroblasto às expensas de produção de colágeno, resultando em degeneração mixoide focal de tecido conjuntivo primariamente afetando a mucosa sobre o osso. Não tem características clínicas distintas e o diagnóstico é baseado somente em características histopatológicas. Este artigo relata dois casos e discute as características clinico-patológicas e imuno-histoquímicas, bem como o diagnóstico diferencial de lesões mixomatosas da cavidade bucal.
DESCRIÇÃO DOS CASOS: Os dois casos de lesões de MOF estavam presentes no palato duro de um paciente do sexo masculino, de 50 anos de idade, e na mandíbula de uma paciente do sexo feminino, de 26 anos. Estes parecem ser os primeiros casos relatados na população da India.
CONCLUSÃO: A análise histopatológica e imuno-histoquímica de Vimentin e proteína S-100 podem ter um papel importante no correto diagnóstico de MOF.
Palavras-chave: Mucinose oral focal; lesão mixomatosa; mucinose cutânea focal; hyaluronic acidcido hialurônico; degeneração mixoide focal
Introduction
Oral Focal Mucinosis (OFM) is an uncommon clinico-pathologic condition that is considered to be the oral counterpart of cutaneous focal mucinosis (CFM). It is a disease of unknown etiology, possibly resulting from overproduction of hyaluronic acid by fibroblasts (1). Clinically the lesion appears as asymptomatic round elevations, which are histologically characterized by a localized area of myxomatous connective tissue containing mucinous material surrounded by relatively dense collagenous connective tissue (2).
It was first described and named by Tomich in 1974 who reported 8 cases as oral counterpart of CFM. However, similar lesions were also previously described in 1966 by Jhonson and Helwig as solitary asymptomatic dome shaped skin nodules seen usually on face, trunk and extremities (2,3).
It is a rare lesion and so far, only 48 cases have been reported in the English literature. This report adds two such rare cases of OFM which are significant clinically as well as histopathologically. The mucosa directly overlying bone appears to be particularly vulnerable, with gingiva being the most common site followed by hard palate. The lesions are generally the same color as surrounding normal mucosa and skin lesions do not seem to accompany oral lesions. The lesions are difficult to diagnose clinically as there are no clinical distinctive features. The review of available literature shows that it is most commonly diagnosed as fibroma or epulis (3). Thus, the histopathological diagnosis becomes important in these conditions.
Despite being the second most common site, the lesions of the hard palate are rare with only five cases being reported up to date (3). We report two more cases, which seem to be the first report in the Indian population.
Description of the Cases
Case 1
A 50 year-old male patient reported to hospital, with the chief complaint of mass behind his upper front teeth since two months. He first noticed the swelling two months back, when it was small, as that of a peanut and gradually increased to the present size. It was not associated with any secondary symptom other than mild pain during speech and mastication, leading to difficulty in speaking and slurred speech. Patient had tobacco chewing habit from past four years, with a frequency of about two to three times a day.
On intraoral examination, well-defined, pinkish, sessile, roughly ovoid growth measuring about 1 x 0.75 cm in its greatest dimension was noted on right side of anterior part of the hard palate in relation to 11 (Fig. 1). The lesion was extending from distal aspect of 12 medially till the mesial aspect of 21 crossing the midline. Anteriorly, it was in close contact with palatal aspect over the cingulum of 11 and extending about 0.75 cm posteriorly. The lesion was non tender and soft to firm in consistency. Indentations were also present on the surface suggesting trauma from mandibular anterior teeth.

On the basis of clinical findings the provisional diagnosis of 'gingival epulis' was given. An excisional biopsy was performed.
Case 2
A 26 year-old female patient reported to hospital, with a chief complaint of a mass on the lower right back gingiva since three months. The mass was initially small to the size of a peanut and gradually increased to the present size. There were no other associated symptoms other than difficulty in speaking and mastication. The growth was firm; non-tender, sessile, measuring about 1.2 centimeters and located on the gingiva of the mandibular right permanent first molar (Fig. 2). The first clinical impression at examination was that of a fibrous epulis of the gingiva. The lesion was removed surgically and sent for histopathological examination. The cut surface of the excised specimen showed a transparent, jelly like mucinous substance (Fig. 3).

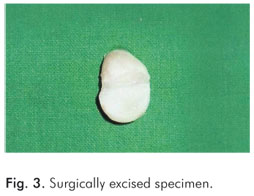
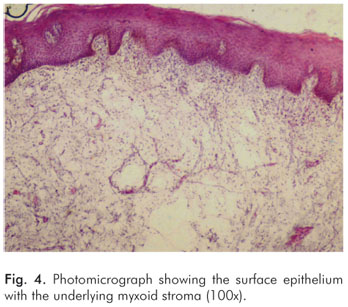
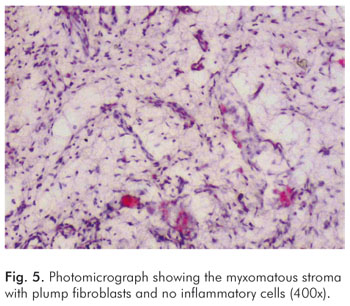
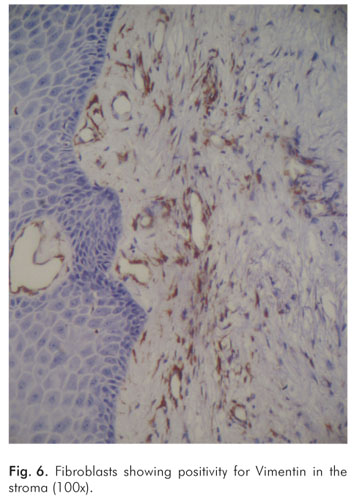
Hematoxylin and eosin stained microscopic slides of both cases revealed a stratified squamous hyper-parakeratinized epithelium and the underlying connective tissue stroma was composed of loose fibro-myxoid stroma with stellate shaped fibroblasts (Fig. 4). Deeper stroma showed spindle shaped fibroblasts interspersed between thin collagen fiber bundles and numerous small blood capillaries (Fig. 5). These histopathological features were suggestive of OFM. Immunohistochemical analysis was also done for Vimentin and S-100 and showed positive reaction for Vimentin (Fig. 6) and negative for S-100 ruling out other myxomatous lesions of neural origin. The surgical wound in both cases healed satisfactorily and no reports of any complication or recurrence since 8 months.
Discussion
OFM is a rare clinico-pathologic condition, first described by Tomich in 1974 and is considered to be the oral counterpart of CFM or cutaneous myxoid cyst (1,2). To the best of our knowledge this report on OFM appears to be first of a kind from the Indian subcontinent in relation to such a large population.
CFM was first named by Johnson and Helwig in 1966 and reported as an asymptomatic, solitary nodule or dome shaped cutaneous lesion of face, trunk or extremities, which were characterized histologically by a mucinous accumulation interspersed with spindle shaped fibroblasts. Earlier, a similar lesion was described as commonly occurring on dorsal aspect of finger and less common on the toes which they termed them as cutaneous myxoid cyst. They considered it as a separate entity because of their different anatomic location and minor histologic variations (4).
Oral lesions of myxomatous nature are relatively rare which include nerve sheath myxoma, soft tissue myxoma, oral focal mucinosis and odontogenic myxomas. Latter one is a bony neoplasm but may occur in soft tissues when they perforate the cortex (5). Etiology of the focal mucinosis is unknown. According to some authors trauma does not appear to play a role in the pathogenesis (4). However, Reed et al. have proposed trauma as an etiologic factor (3,6). In the first case reported here, trauma might have played a role in the etiology, as there was traumatic bite with the mandibular anterior teeth impinging on the lesion. Indentations were also noted on the otherwise smooth surface of the lesion. Johnson et al. attributed the pathogenesis of the cutaneous lesions to an overproduction of hyaluronic acid by fibroblast at expense of collagen production, replacing most of the collagen. As the histochemical characteristics of oral and cutaneous lesions are same, hence the same pathogenesis has been attributed to the oral lesion too (3,4).
OFM is seen primarily in adult patients in an age group of 16-68 years with only one case reported in a 4 year old female patient. The literature shows a female predilection, with 31 cases recorded in females and 18 in males. The mucosa directly overlying bone is particularly affected, with gingiva being the most common site followed by hard palate. Out of 48 cases reported till date, 31 cases have been noted on the gingiva, 5 cases on the hard palate and 3 cases each on alveolar mucosa, buccal mucosa, and tongue and 2 cases on lips. However, for one case the site was not specified (1,3). Thus, our case one is rare and appears to be the first case to be reported on the hard palate in a male patient.
Clinically these lesions present as sessile or pedenculated, painless nodular mass and are of same color as surrounding normal mucosa. Surface is typically smooth and non-ulcerated, although occasional cases exhibit a lobulated appearance. Size varies from few mms to 2 cm in diameter. The patient often has been aware of mass for many months or years before diagnosis is made (1). In the first case there was a pink, sessile, well defined, regular, roughly ovoid smooth mass of about 1 x 0.75 cm in its greatest dimension on right side of anterior part of the hard palate in relation to 11. The second case occurred as a sessile gingival mass, measuring about 1.2 cms with smooth non ulcerated soft to firm mass.
OFM has no distinctive clinical features and most often thought to be clinically as fibroma, gingival epulis, pyogenic granuloma, mucocele or similar lesions. Traumatic fibroma, pyogenic granuloma and minor salivary gland tumor were also considered in the differential diagnosis. A review of all reported cases show that it was never diagnosed clinically as 'oral focal mucinosis' (3). The histological features are always the basis for the diagnosis.
Microscopic examination of both cases showed a well localized but non encapsulated area of loose, myxomatous connective tissue stroma surrounded by dense, normal thin collagen bundles. The sub-epithelial pale eosinophilic myxoid stromas representing an overproduction of hyaluronic acid with stellate shaped fibroblasts were noted. Deeper stroma showed spindle fibroblasts, thin bundles of collagen fibers and numerous small blood capillaries along with diffuse infiltration of mixed inflammatory cells consisting of mainly lymphocytes and plasma cells. All these features were suggestive of OFM.
Immunohistochemical analysis was done to differentiate from myxoid neural lesions, which are positive for S-100. Vimentin is consistently present and correlated with the number of fibroblast-like cells (7). Both cases were sent for immunohistochemical analysis of Vimentin and S-100 protein and results showed positive stain for Vimentin and negative staining for S-100, study ruling out the myxomatous lesion of neural origin.
Microscopically, OFM is seen just beneath the surface epithelium and often causes flattening of rete ridges. The fibroblast within the mucinous area can be ovoid, spindle, fusiform or stellate and may demonstrate delicate fibrillar process. Few capillaries within the lesion, especially compared with the surrounding denser collagen are seen. Similarly, no significant inflammation was observed, although a perivascular lymphocytic infiltration often noted within the surrounding collagenous connective tissue (1,2,3). Radiographic examination of the lesion in both cases did not reveal any abnormality. To conclude, oral focal mucinosis appears to be a mesenchymal derived lesion composed predominantly of fibroblasts (8). It must be stressed that in most focal gingival lesions, a preoperative diagnosis can be almost impossible. The histopathological and immunohistochemical analysis of Vimentin and S-100 protein play a vital role in the correct diagnosis.
References
1. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillo facial pathology. 2nd ed. Philadelphia, Pennsylvania: Elsevier; 2002. [ Links ]
2. Buchner A, Merrell PW, Leider AS, Hansen LS. Oral focal mucinosis. Int J Oral Maxillofac Surg 1990;19:337-40. [ Links ]
3. Lima AAS, Machado MAN, Martins WD, Grégio AMT, Dirschnabel AJ, Mattioli TMF et al. Oral focal mucinosis. Quintessence Int 2008; 39:611-5. [ Links ]
4. Tomich CE. Oral focal mucinosis: A clinic pathologic and histochemical study of eight cases. Oral Surg 1974;38:714-24. [ Links ]
5. Green TL, Leighty SM, Walters R. Immunohistochemical evaluation of oral myxoid lesions. Oral Surg Oral Med Oral Pathol 1992;73:469-71. [ Links ]
6. Reed RJ, Clark WH, Mihm MC. The cutaneous mucinosis. Hum Pathol 1973;4:201-5. [ Links ]
7. Aldred MJ, Talacko AA, Ruljancich K, Story RD, Newland S, Chen ST et al. Oral focal mucinosis: report of 15 cases and review of the literature. Pathology 2003;35:393-6. [ Links ]
8. Wilk M, Schmoeckel C. Cutaneous focal mucinosis: A histopathological and immunohistochemical analysis of 11 cases. J Cutan Pathol 1994;21:446-52. [ Links ]
 Correspondence:
Correspondence:
Manjunatha BS
KM Shah Dental College & Hospital
Pipariya post, Waghodia road
Vadodara-391760, Gujarat State – India
E-mail: drmanju26@hotmail.com
Received: May 10, 2010
Accepted: August 17, 2010
Conflict of Interest Statement: The authors state that there are no financial and personal conflicts of interest that could have inappropriately influenced their work.













