Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.3 Porto Alegre Jul./Set. 2012
CLINICAL / CLÍNICO
Neurilemmoma of the oral cavity in pediatric patient
Neurilemoma em cavidade oral acometendo paciente pediátrico
Pedro Paulo de Andrade SANTOS I; Bruna Rafaela Martins dos SANTOS II; Valéria Souza FREITAS III; Roseana de Almeida FREITAS IV; Lélia Batista de SOUZA IV
I Universidade Federal de Campina Grande, Centro de Saúde e Tecnologia Rural, Unidade Acadêmica de Ciências Biológicas. Patos, PB, Brasil
II Universidade do Estado do Rio Grande do Norte. Caicó, RN, Brasil
III Universidade Estadual de Feira de Santana, Departamento de Saúde, Colegiado de Odontologia. Feira de Santana, BA, Brasil
IV Universidade Federal do Rio Grande do Norte, Centro de Ciências da Saúde, Programa de Pós-Graduação em Patologia Oral. Av. Salgado Filho, 1787, 59056-000, Lagoa Nova, Natal, RN, Brasil
ABSTRACT
Neurilemmomas arising from Schwann cells, rarely found in oral cavity, are characterized by solitary occurrence, slow growth and smooth surface with variable clinical aspects, depending on the nerve origin. Most instances are typically asymptomatic. Microscopically, the histopathological characteristic consists of alternating regions of hypercellularity and hypocellularity such as Antoni A and Antoni B, respectively. The prognosis is favorable; complete surgical removal is the treatment of choice, no recurrence should be expected. The present report shows the case of neurilemmoma in bucal mucosa, in a 9-year-old child. Patient was referred to the Stomatology Clinic of School of Dentistry, Universidade Federal do Rio Grande do Norte, with complaint of nodular mass, with approximately one year development. Patient was submitted to excisional biopsy, with histopathological exam showing diagnosis of neurilemmoma. After 1 year follow-up there has been no recurrence of lesion.
Indexing terms: Mouth. Neurilemmoma. Pediatrics.
RESUMO
Os neurilemomas se originam das células de Schwann e raramente são encontrados na cavidade oral, sendo caracterizados por uma ocorrência solitária de crescimento lento e superfície lisa com aspectos clínicos variáveis dependendo do nervo de origem, sendo tipicamente assintomático. Microscopicamente, as características histopatológicas consistem de regiões alternadas de hipercelularidade e hipocelularidade, conhecidas como Antoni A e Antoni B respectivamente. Apresentando um prognóstico favorável, onde o tratamento de escolha é a excisão cirúrgica completa, não sendo esperada recorrência. O presente relato descreve a presença de um neurilemoma em mucosa jugal, acometendo uma criança de 9 anos de idade, que compareceu ao Serviço de Estomatologia da Faculdade de Odontologia da Universidade Federal do Rio Grande do Norte, queixando-se de uma massa nodular, há aproximadamente 1 ano. O paciente foi submetido a biópsia excisional, sendo diagnosticado através do exame histopatológico como neurilemoma e há 1 ano vem sendo acompanhado por nossa equipe sem recorrência da lesão.
Termos de indexação: Boca. Neurilemoma. Pediatria.
INTRODUCTION
Neurilemmoma or Schwanoma is a rare, benign, neurogenic, encapsulated and slow growing tumor. It originates from Schwann cells of the peripheral nerves and may occur at any site where there are nerves with Schwann cells1. These types of cells are responsible for lining the myelinic nerve cells2.
Between 25 to 40% of cases affect the region of the head and neck3. However, it is not commonly found in the oral and maxillofacial region, and is even rarer intraorally, accounting for only 1% of cases4. When the neurilemmoma appears in the oral cavity, this lesion is most frequently found in the tongue5, particularly in individuals in the second through to the fourth decades of life6-7. Its appearance in children 10 years old or younger is very rare8. In this article, a rare case of neurilemmoma located in the jugal mucosa of a child only 9 years old is reported.
CASE REPORT
The patient, a 9-year-old boy presented to the Stomatology Clinic of the Dental Department, Federal University of Rio Grande do Norte, accompanied by his guardian, complaining of the appearance of a mass, initially of small size that gradually became bigger, located in the jugal mucosa, approximately 1 year ago. It was painless and not associated with local trauma.
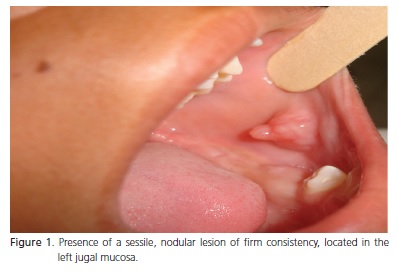
The intraoral clinical exam revealed the presence of a nodular, sessile lesion, located in the left jugal mucosa, presenting a color similar to that of the normal mucosa, measuring 2.5 x 2.0 cm in its largest diameters. It had a predominantly smooth surface with slightly ondulated areas, exhibiting another exophytic growth in the more superior and central portion of the lesion, which fitted in between his teeth. The lesion was firm on palpation, without ulcers or inflammation (Figure 1).
On physical exam it was found that the lymph nodes were not increased in size, and no other lesion was verified. The child's medical history showed nothing noteworthy.
In the authors' investigation, no imaging resources were used, as the lesion was easily visible and palpable.
According to the clinical findings, the clinical hypothesis of fibroma and fibrous hyperplasia were proposed. The patient was submitted to an excisional biopsy and the material was duly sent for histopathological exam.
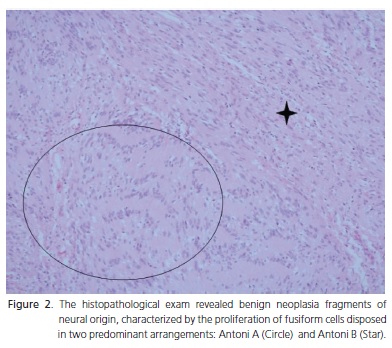
Using routine hematoxylin-eosin (HE) staining, the histopathological exam revealed fragments of benign neoplasia of neural origin, characterized by the proliferation of fusiform cells disposed in two predominant arrangements: one characterized by the cells organized into palisade (Antoni A) around the central acellular, eosinophilic area (Verocay bodies) and the other, in which the proliferating cells were loosely arranged in a disorganized pattern (Antoni B). With these histopathological findings, the diagnosis of neurilemmoma was given (Figure 2).
DISCUSSION
The neurilemomma (Schwanoma) was described for the first time in 1908 by Virchow9, as being a solitary tumor, usually encapsulated, which is derived from Schwann cells, grows, expands and may cause displacement and compression of the nerve or origin10. It is frequently difficult to identify the nerve from which the neurilemomma originates4.
The etiology of this lesion is still unknown, but it may arise from spontaneous growth, external injury, chronic irritation or exposure to radiation11.
The clinical presentation of this case was one of a lesion that increased in size, with development of approximately 1 year. However, in spite of the increase in volume, it remained painless, affecting the jugal mucosa region in a child, therefore, contrary to the data shown in the pertinent literature, which points out the tongue as the most affected intraoral site, and adult age as the most frequent time of occurrence10.
Neurilemmomas generally exhibit a size between 1 and 4cm, but may have larger diameters when located in the mediastinal and retroperitoneal region12. Although the lesion diameter in the case here reported varied from the predicted size, it should be pointed out that 2.5 cm for an intraoral neurilemmoma represents a lesion of considerably large size, particularly since it concerns a child.
There is no predilection for sex, however, some reports indicate a predilection for the male sex3 and the definitive diagnosis requires a histopathological exam, characterized by the presence of densely arranged fusiform cells (Antoni A) with a typical arrangement in palisade (Verocay bodies) and hypocellular arrangements (Antoni B) without defined architecture5,8,10,13-14.
Clinically, the differential diagnosis of neurilemmoma in the oral cavity may be made with salivary gland tumors, leiomyomas, rhabdomyomas, lypomas and inflammatory lesions4, and neuromas and neurofibromas may also be included6.
The prognosis of the neurilemmoma is completely favorable, with conservative surgical treatment being the procedure of choice, and ample incision is not indicated. If complete enucleation is performed, no recurrence is expected. Malignant transformation of the neurilemmoma is still a controversial topic; some authors doubt that this occurs, nevertheless, some isolated cases have been documented7-13.
In the case here reported, after surgical nucleation performed during the excisional biopsy and obtaining the histopathological diagnosis of neurilemmoma, the patient has been followed up by the authors' team for 1 year, without evidence of recurrence of the lesion.
CONCLUSION
Although the neurilemmoma does not present specific clinical characteristics, and is similar to other lesions such as fibroma and fibrous hyperplasia, it is always important to perform the biopsy for the diagnosis of lesions that affect the oral cavity, and send the material to a specialized pathology service for correct diagnosis, thus enabling implementation of the appropriate treatment.
Collaborators
PPA SANTOS photographed the case, was responsible for the literature, and participated in writing the article. BRM SANTOS was responsible for the literature, and participated in writing the article. VS FREITAS and LB SOUZA participated in writing the article. RA FREITAS prepared the histopathological report and participated in writing the article.
REFERENCES
1. Lacerda SA, Brentegani LG, Rosa AL, Vespúcio MVO, Salata LA. Intraosseous schawannoma of mandibular symphysis: case report. Braz Dent J. 2006;17(3):255-8. doi: 10.1590/S0103- 64402006000300015. [ Links ]
2. Chi AC, Carey J, Muller S. Intraosseous schwannoma of the mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(1):54-65. doi: 10.1016/S1079-2104(03)00228-2.
3. Graham RM, Thomson EF, Woodwards RTM. Benign schwanoma of the left cervical phrenic nerve. Br J Oral Maxillofac Surg. 2008;46(2):161-2. doi: 10.1016/j.bjoms.2007.03.002.
4. Enoz M, Suoglu Y, Ilhan R. Lingual schwannoma. J Cancer Res Ther. 2006;2(2):76-8. doi: 10.4103/0973-1482.25856.
5. Martins M, Anunciato de Jesus L, Fernandes K, Bussadori S, Taghloubi S, Martins MA. Intra-oral schwannoma: case report and literature review. Indian J Dent Res. 2009;20(1):121-5. doi: 10.4103/0970-9290.49059.
6. Amir R, Altman KW, Zaheer S. Neurilemmoma of the hard palate. J Oral Maxillofac Surg. 2002;60(9):1069-71. doi: 10.1053/ joms.2002.34423.
7. Yang SW, Lin CY. Schwannoma of the upper lip: case report and literature review. Am J Otolaryngol. 2003; 24(5):351-4. doi: 10.1016/S0196-0709(03)00065-6.
8. Nakasato T, Kamada Y, Ehara S, Miura Y. Multilobular neurilemmoma of the tongue in a child. AJNR Am J Neuroradiol. 2005;26(2):421-3.
9. Wada A, Matsuda H, Matsuoka K, Kawano T, Furukawa S, Tsukuda M. A case of schwannoma on the nasal septum. Auris Nasus Larynx. 2001;28(2):173-5. doi: 10.1016/S0385- 8146(00)00099-7.
10. Santos PPA, Freitas VS, Pereira Pinto L, Freitas RA, Souza LB. Clinicopathologic analysis of 7 cases of oral schwannoma and review of the literature. Ann Diagn Pathol. 2010;14(4):235-9. doi: 10.1016/j.anndiagpath.2010.02.009.
11. Hwang K, Kim SG, Ahn SI. Neurilemmoma of the tongue. J Craniofac Surg. 2005;16(5):859-61.
12. Arda HN, Akdogan O, Arda N, Sarikaya Y. An unusual site for an intraoral schwannoma: a case report. Am J Otolaryngol. 2003;24(5):348-50. doi: 10.1016/S0196-0709(03)00064-4.
13. Kowatsch E, Feichtinger M, Zemann W, Karpf E, Kärcher H. Extraosseous schwannoma of the mental nerve clinically simulating intraosseous. J Oral Pathol Med. 2006;35(8):517-9. doi: 10.1111/j.1600-0714.2006.00429.x.
14. Ying YLM, Zimmer LA, Myers EN. Base of tongue schwannoma: a case report. Laryngoscope. 2006;116(7):1284-7. doi: 10.1097/01.mlg.0000224358.55022.8a.
 Correspondence to:
Correspondence to:
RG TEIXEIRA
e-mail: rgte@terra.com.br
Received on: 12/11/2009
Approved on: 6/9/2010













