Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.1 Porto Alegre Jan./Mar. 2013
ORIGINAL / ORIGINAL
Evaluation of oral diseases in a population of special needs patients
Avaliação das doenças orais em uma população de pacientes com necessidades especiais
Francisco Artur Forte OLIVEIRAI; Clarissa Pessoa FERNANDESI; Filipe Nobre CHAVESI; Lorena Barreira MAGROIII; Fabrício Bitu SOUSAI; Rafael Lima Verde OSTERNEII
I Universidade Federal do Ceará, Faculdade de Farmácia, Odontologia e Enfermagem Departamento de Clínica Odontológica
II Universidade de Fortaleza, Curso de Medicina. Fortaleza, CE, Brasil
III Centro de Especialidades Odontológicas Regional de São Gonçalo do Amarante, Setor de Pacientes Especiais. São Gonçalo do Amarante, CE, Brasil
ABSTRACT
Objective
To evaluate the oral health status of a population of patients with special needs cared for in the specialization course of the Brazilian Association of Dentistry, Ceará Branch.
Methods
In this cross-sectional, descriptive study the indexes DMFT and CPI were used to evaluate dental caries and periodontal disease, respectively, from August 2009 through March 2010. The need for dental treatment and other soft tissue lesions were also investigated.
Results
88 patients selected by convenience sampling were examined intraorally, and the mean age was 43.8 ± 16. Most of the patients fell within the group of systemic diseases (68.1%), especially cardiovascular diseases (15.9%). The mean DMFT index was 17.54 ± 7.13, and 87.5% of patients presented active dental caries. According to the highest degree of periodontal condition observed in the individual, the dental tartar (index 2) was present in a greater number of patients (50.9%). Regarding the need for dental treatment, 68.1% of patients needed restorative treatment, 43.1% of patients needed surgery (extractions) and 21.5% of patients needed endodontic treatment. There were no soft-tissue abnormalities in most patients (89.7%).
Conclusion
The examined patients showed a high prevalence of oral diseases such as dental caries and gingivitis/periodontitis, and therefore a great need for dental treatment. Given the results, it becomes important to stimulate dental care and preventive practices focused on this segment of the population.
Indexing terms: Dental care for disabled. Dental care for the chronically ill. Epidemiology. Oral health.
RESUMO
Objetivo
Avaliar a condição de saúde bucal de uma população de pacientes com necessidades especiais atendida no curso de especialização da Associação Brasileira de Odontologia, Seção Ceará.
Métodos
Nesse estudo de natureza descritiva e transversal utilizou-se os índices CPO-D e IPC para avaliação das doenças cárie e periodontal, respectivamente, entre os meses de Agosto de 2009 e Março de 2010. Necessidades de tratamento dentário e outras lesões em tecidos moles orais também foram investigadas.
Resultados
Realizaram-se exames bucais em 88 pacientes selecionados por conveniência, sendo a média de idade correspondente a 43,8 ± 16 anos. A maioria se enquadrava no grupo de doenças sistêmicas (68,1%), destacando-se as diseases cardiovasculares (15,9%). O índice CPO-D médio foi 17,54 ± 7,13, com 87,5% dos pacientes apresentando cárie ativa. Segundo o maior grau de condição periodontal observado no indivíduo, o cálculo dental (índice 2) foi o que esteve presente em um maior número de pacientes (50,9%). Quanto às necessidades de tratamento dental, 68,1% deles necessitaram de tratamento restaurador, 43,1% de tratamento cirúrgico (exodontias) e 21,5% de tratamento endodôntico. Não foram encontradas anormalidades em tecido mole na maioria dos pacientes (89,7%).
Conclusão
Os pacientes examinados possuíam alta prevalência de doenças orais, como cárie e gengivite/periodontite e, conseqüentemente, grande necessidade de tratamento odontológico. Diante dos resultados, torna-se importante motivar a atenção odontológica e as práticas preventivas voltadas para essa parcela da população.
Termos de indexação: Assistência odontológica para pessoas com deficiência. Assistência odontológica para doentes crônicos. Epidemiologia. Saúde bucal.
INTRODUCTION
People with Special Needs are characterized as individuals with some loss of or abnormality of a structure and/or psychological, physiological or anatomical function, either permanent or temporary, which creates the inability to perform the essential activities of everyday life, originating from or aggravated by the economic and social environment in which they live. They are people with physical, motor or sensory restrictions mainly caused by congenital or perinatal disorders; transmissible diseases and non-transmissible chronic diseases; psychiatric disturbances; drug abuse; as well as trauma arising from violence or traffic accidents1.
Dentistry for Patients with Special Needs is the area of health that provides personalized dental treatment, which requires care that goes far beyond routine, for these individuals that have some or other medical, mental or psychological affliction2. Based on this reality, the Brazilian Federal Dental Council, during the 2nd National Assembly on Dental Specialties (ANEO), in section XI of Article 31 of resolution CFO-22/2001, produced a standard for the creation of a specialty for patients with special needs by establishing a number of policies. The specialist professional, therefore, should be able to provide, along with a multidisciplinary team in certain cases, a complete and safe dental care to these patients3.
The actual situation with oral health of Special Needs Patients in Brazil is still unknown. The majority of studies carried out so far cover specific groups of patients such as those with neurological4 or oncological changes5, and there is a need to carry out more comprehensive scientific studies that can serve as a basis for actions that provide an improvement in the oral health of these individuals.
Accordingly, the aim of this research study was to evaluate the state of the oral health of patients with special needs attended to in a specialization course in Fortaleza, in the Brazilian state of Ceará.
METHODS
This descriptive, cross-sectional study had a population of 206 patients cared for in the specialization course in Dentistry for Patients with Special Needs, run by the Brazilian Dental Association, Ceará Branch, between August 2009 and March 2010.
The convenience sample comprised 88 patients, selected and examined at the time of their first appointment by two researchers, F.A.F.O. and C.P.F. The examinations were conducted together, after theoretical training to understand all the indices, codes and dental condition or state, to be used on the examination record cards, thereby standardizing the information.
The data were collected via clinical examination record cards which addressed sociodemographic aspects: name, sex, age, city/state of residence, as well as the base disease afflicting them, medical comorbidities and medication used. It also included data for the evaluation of dental health, DMFT index; periodontal data, Community Periodontal Index (CPI); caries treatment needs; and characteristics for lesions found in the oral soft tissues.
The DMFT is an index recommended by the World Health Organization (WHO) to measure and compare experience of dental caries in populations and its value expresses the average of decayed, missing and filled teeth in a group of individuals. The CPI, on the other hand, evaluates the periodontal condition by sextant as to state of health, bleeding and presence of dental tartar or pocket6.
For patients whose systemic state of health made it impossible to carry out a periodontal evaluation at the start, due to the possible damage to health caused by transient bacteremia, this evaluation was performed in subsequent sessions, before being subjected to dental procedures that required the performance of the protocol of prior antibiotic prophylaxis advocated by the American Heart Association (AHA)7.
The patients were grouped into diverse categories, according to medical affliction, adapted classification8, to ascertain the diseases most prevalent in the sample. The indices used in this study for caries, the need for dental treatment and periodontal disease, were those recommended by the World Health Organization (1997), also used in the SB Brasil 2000 project9.
The statistical analysis of the data was done after the production of spreadsheets (Office 2007 - Microsoft, USA) by the software application GraphPad Prism® version 5.00 for Windows® (GraphPad Software, San Diego, California, USA). The following values were calculated: average, standard deviation, median and maximum values of the DMFT variables, need for treatment, CPI and its components, as well as a comparison between the disease groups by taking into account the DMFT index, through the variance analysis (ANOVA) associated with the Tukey multiple comparison test. The level of significance was set at 5%, so a value of p<0.05 was considered as statistically significant.
In compliance with ethical maxims, the study was submitted to and approved by the Ethics in Research Committee at the Dona Libânia National Center of Reference in Dermatology Hygiene (CDERM), filed under reference no. 017/09.
RESULTS
The study consisted of the performance of 88 oral examinations. The frequency between the sexes was identical and the average patient age was 43.8± 16 (ranging from 12 to 84), the age brackets of 40 to 49 (22.7%) and 50 to 59 (22.7%) being the most prevalent.
Approximately 73% (64) of the sample resided in the state capital Fortaleza where the study was carried out and 24.5% (23) came from 19 municipal districts in the hinterland.
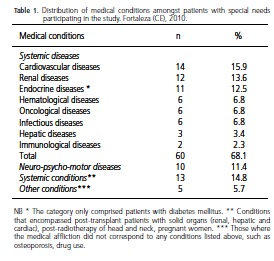
As far as the medical diagnosis is concerned, the majority of patients fell into the group of systemic diseases (68.1%), the main ones being cardiovascular disease (15.9%), renal disease (13.6%) and endocrine disease (12.5%). Approximately 11% of individuals presented with neuro-psycho-motor disorders. The numeric and percentage distribution of the medical conditions encountered are set out in Table 1.
As for medical comorbidities presented by the patients, the most prevalent was high blood pressure, which was present in 22.6% of them. Additionally, 86% of the patients were using at least one medication.
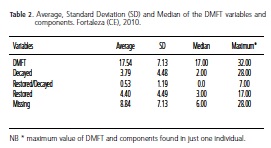
In terms of the dental state, the average DMFT of the patients was 17.54 ± 7.13, w i th 87.5% of them presenting with active caries. The average for decayed, restored/decayed, restored and missing teeth per patient is shown in Table 2.
No statistically significant difference was found, according to the DMFT index, when the most prevalent disease groups (cardiovascular, renal, neuro-psycho-motor and endocrine diseases) were compared.
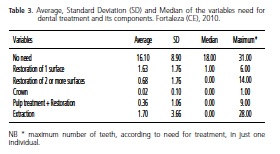
As for the need for dental treatment, in the sample examined, approximately 91% of patients had a need for treatment of which 60 (68.1%) needed restoration treatment in at least one tooth, 38 (43.1%) needed surgical treatment (extraction), 19 (21.5%) needed endodontic treatment and 1 (1.1%) needed a prosthetic crown. The average number of teeth per patient, either with or without the need for treatment for caries and its components, is shown in Table 3.
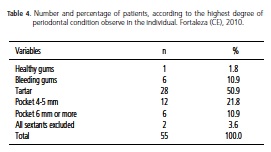
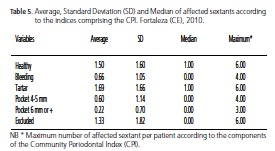
As regards periodontal condition, 55 (62.5%) patients were examined. According to the highest degree of periodontal condition observed in the individual (Table 4), dental tartar (score of 2) was the one present in the largest number of patients (50.9%) and only 1 (1.8%) had healthy gums (score of 0). As far as the distribution of sextant averages is concerned, according to the CPI indices (Table 5), the highest was that of sextants with dental tartar (1.69), followed by healthy (1.5) and excluded (1.33).
In the physical examination of inspection and intra-oral palpation, abnormalities were found in the soft tissue in 9 (10.2%) individuals. One example was of lesions presenting as traumatic ulcers, facilitated by the hyposalivation and dental condition in one patient that had been subjected to radiotherapy treatment for the head and neck.
DISCUSSION
In the present study, 24.5% of patients lived in 19 different municipalities from the Ceará hinterland and came to the state capital to have dental treatment in the Institution (ABO/CE). This piece of data is a reflection, as it is in other countries, according to Davis10, of a failure in the access of these patients to health services, principally dental services, either because of the lack of specialist public services focusing on the oral health of these individuals or through the scarcity of professionals qualified to provide them with care. Some of these patients, such as those with neuro-psycho-motor diseases have difficulty in getting around, which makes it even more complicated for longer journeys, such as those made by around 1/4 of the sample studied, residing in the state hinterland. The creation and decentralization of specialist centers or the insertion of this population into primary health care, are measures that could reduce this problem.
The vast majority of patients evaluated suffered from some or other systemic disease, with the medical comorbidity most seen amongst individuals being high blood pressure (22.6%), and as the majority of them (86%) used at least one form of medication, considerations in respect of the control of anxiety, choice of local anesthetics, understanding of drug interactions and their adverse reactions, including in the oral mucous, are drivers in the clinical conduct of these patients11-12. The lack of epidemiological studies, which include all special patients, and the absence of a unique classification for special needs patients in dentistry, makes it difficult to compare the findings of other studies. One important factor to note is the huge variety of systemic diseases identified in the present study, showing that dental surgeons need to have better understanding of these diseases and greater involvement in multidisciplinary health teams.
The experience of caries presented by the special patients in the sample was high, with the majority of patients presenting with active caries. The prevalence of periodontal alterations was also seen to be high and a large number of the patients had a maximum index of 2 (dental tartar) or 3 (pocket 4-5 mm). Data similar to those in the present study were reported by Soares et al.13, who evaluated the dental and periodontal condition in HIV positive patients, finding an average DMFT of 19.7, the most frequent condition being that of missing teeth, with an average of 11.8. As far as the CPI is concerned, the most prevalent condition was dental tartar (40%) and just one patient was healthy in all sextants.
The high prevalence of oral diseases, primarily those related to a history of dental caries, is a chronic problem that affects a large proportion of the Brazilian population, according to data from SB Brasil 200314, however special needs patients could be subject to an aggravation of their systemic conditions due to defective oral health. One such example is what occurs with transplant patients using immunosuppression therapy, which could present systemic infections originating from infectious outbreaks in the oral cavity, or with oncology patients having chemotherapy treatment who could have their therapy suspended due to the exacerbation of dental infections, resulting in great morbidity amongst them.
Ineffective oral hygiene is as much a driver of the oral health of these patients as is the difficulty of access to dental services or there being few professionals who propose to care for them. Often, these individuals do not have good oral hygiene because they do not have the ability to carry it out, because they will not allow other people to do it for them, or by neglecting it due to stress, tiredness or depression. Moreover, some groups of special patients such as diabetics, influenced by their systemic condition, tend to have more exaggerated oral alterations15-17.
As opposed to the 9% and 1.8% of patients who, did not need some form of dental or periodotal, the majority required basic dental procedures, such as restorations (68.1%), dental extractions (43.1%) and supra-gingival scaling (61.8%). It should be pointed out that, in many cases, these procedures may be carried out within the family health program, mainly on patients with controlled, stable diabetes and hypertension, as there are already programs directed towards these two groups in basic healthcare18.
For those non-controlled patients or patients with more complex diseases or conditions, such as the pretransplant of solid organs (heart, kidney and liver), the planning of dental treatment should be somewhat more meticulous. Teeth for which direct restoration treatment is rendered impossible that have radiolucent lesions seen radiographically at their apices, or which have periodontal furcation lesions, should be removed by surgery, bearing in mind that these individuals, after the transplant, will be in immunosuppression state, i.e. more prone to infection, and their healing ability will be compromised19. The extraction, or not, of unerupted third molars should also be carefully considered, as the partially erupted teeth after transplant could cause situations of grave pericoronitis in these patients.
No abnormalities of the soft tissues were found in the majority of patients (89.7%). It should be remembered, however, that patients with systemic health alterations could present with oral lesions, such as patients with AIDS who could have oral and perioral manifestations indicative of frail overall health and a worse prognosis of the disease20, as well as mucositis and stomatitis that could arise in individuals after radiotherapy treatment of head and neck or grave renal insufficiency21-23. These oral manifestations could also be important in the diagnosis of an individual's systemic disease as oral signs can sometimes be the first to be detected24. This underlines the need for a detailed anamnesis and clinical examination by the dental surgeon, which should be part of the dental routine at all levels of care.
The length of monitoring time between consultations will depend on the special needs group in which the dental treatment was carried out. Oncology patients, for example, should carry out oral adaptation prior to chemotherapy or radiotherapy treatment in the head and neck region, and even when this stage is completed, they should be monitored from a dental perspective, via regular visits during radiotherapy and chemotherapy, as in this way the dentist will be able to intervene promptly in the event of common oral problems arising from medical treatment, such as mucositis25-26. Another situation would be that of patients who complete their dental treatment with the purpose of adaptation for the transplant of solid organs and need periodic monitoring for a short period of time before this procedure is carried out27.
When presenting the results of this study, it is necessary to understand a potential limitation that exists in terms of the difficulty in finding studies in the literature that are similar to this one, that embrace a fairly diverse population of patients with special needs. However, the performance of studies such as this one would appear to be essential to evidence the need for the creation of new specialist centers, mainly in the state hinterland, and the deficiency in the qualification of dental surgeons, as there exist few professionals who are suitable for caring for these patients, having a direct impact on the lack of the inclusion of a large part of special needs patients in basic care.
It is important to arouse interest in dental care and preventive practices aimed at this section of the population. Further studies should be encouraged to acquire a fuller understanding of the needs of these patients and to publicize the specialty of Dentistry for Special Needs Patients amongst health professionals.
CONCLUSION
The studied population comprised predominantly individuals between the ages of 40 and 60, with identical frequency between the sexes and patients with systemic diseases were the most frequent. A high prevalence was observed of oral diseases, such as caries and gingivitis/ periodontitis and, consequently a greater need for dental treatment. Abnormalities in the soft tissues were not found in the majority of patients.
Collaborators
FAF OLIVEIRA and CP FERNANDES contributed to the concept, design, data collection, data interpretation and composition of the article. FB SOUSA and RLV OSTERNE took part in the concept, design, critical review of the intellectual content and the composition of the article. FN CHAVES and LB MAGRO took part in the design, data analysis, statistical analysis, data interpretation and the composition of the article.
REFERENCES
1. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Política Nacional de Saúde da Pessoa Portadora de Deficiência. Brasília: Ministério da Saúde; 2008 [citado 2010 Nov 5]. Disponível em: <http://bvsms.saude.gov.br/bvs/publicacoes/politica_nacional_saude_pessoa_deficiencia.pdf> [ Links ].
2. Lawton L. Providing dental care for special patients: tips for the general dentist. J Am Dent Assoc. 2002;133(12):1666-70. [ Links ]
3. Peres AS, Peres S, Silva RHA. Atendimento a pacientes especiais: Reflexão sobre os aspectos éticos e legais. Rev Fac Odontol Lins. 2005;17(1):49-53. [ Links ]
4. Seirawan H, Schneiderman J, Greene V, Mulligan R. Interdisciplinary approach to oral health for persons with developmental disabilities. Spec Care Dentist. 2008;28(2):43- 52. doi: 10.1111/j.1754-4505.2008.00010.x. [ Links ]
5. Osterne RLV, de Matos Brito RG, Nogueira RLM, Soares ECS, Alves APNN, Moura JFB, et al. Saúde bucal em pacientes portadores de neoplasias malignas: Estudo clínico-epidemiológico e análise de necessidades odontológicas de 421 pacientes. Rev Bras Cancerol. 2008;54(3):221-6. [ Links ]
6. Brasil. Ministério da Saúde. Projeto SB2000: condições de saúde bucal da população brasileira no ano 2000. Manual do examinador. Brasília: Ministério da Saúde; 2001 [citado 2010 Nov 6]. Disponível em: <http://bvsms.saude.gov.br/bvs/publicacoes/condSB_man_exam.pdf> [ Links ].
7. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116(15):1736-54. [ Links ]
8. Little JW, Falace DA, Miller CS, Rhodus NL. Dental management of the medically compromised patient. St. Louis: Mosby Elsevier; 2008. [ Links ]
9. Brasil. Ministério da Saúde. Projeto SB2000: condições de saúde bucal da população brasileira no ano 2000. Manual do coordenador. Brasília: Ministério da Saúde; 2001 [citado 2010 Nov 6]. Disponível em: <http://189.28.128.100/dab/docs/manuais_sbbrasil/man_coord/man_coord.pdf> [ Links ].
10. Davis MJ. Issues in access to oral health care for special care patients. Dent Clin North Am. 2009;53(2):169-81. doi: 10.1016/j.cden.2008.12.003. [ Links ]
11. Yagiela JA, Haymore TL. Management of the hypertensive dental patient. J Calif Dent Assoc. 2007;35(1):51-9. [ Links ]
12. Friedlander AH, Yagiela JA, Paterno VI, Mahler ME. The neuropathology, medical management and dental implications of autism. J Am Dent Assoc. 2006;137(11):1517-27. [ Links ]
13. Soares MSM, Gonçalves LFF, Macena MSA, Bertazzoli RCB, Queiroga AS, Ângelo AR. Condição periodontal e dentária em pacientes HIV positivos. RGO - Rev Gaúcha Odontol. 2009;57(4):419-23. [ Links ]
14. Brasil. Ministério da Saúde. Coordenação Nacional de Saúde Bucal. Condições de saúde bucal da população brasileira. Projeto SB Brasil 2003: resultados principais. Brasília: Ministério da Saúde; 2004 [citado 2010 Nov 6]. Disponível em: <http://cfo.org.br/wp-content/uploads/2009/10/04_0347_M.pdf> [ Links ].
15. Bonito AJ, Cooper LY. Dental care considerations of disadvantaged and special care populations. Baltimore (MD): U.S. Department of Health and Human Services. Health Resources and Services Administration; 2001. [ Links ]
16. Mealey BL, Oates TW, American Academy of Periodontology. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77(8):1289-303. doi: Diabetes mellitus and periodontal diseases. [ Links ]
17. Bayraktar G, Kurtulus I, Duraduryan A, Cintan S, Kazancioglu R, Yildiz A, et al. Dental and periodontal findings in hemodialysis patients. Oral Dis. 2007;13(4):393-7. doi: 10.1111/j.1601- 0825.2006.01297.x. [ Links ]
18. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Diretrizes da Política Nacional de Saúde Bucal. Brasília: Ministério da Saúde, 2004 [citado 2010 Nov 6]. Disponível em: <http://bvsms.saude.gov.br/bvs/publicacoes/politica_nacional_brasil_sorridente.pdf> [ Links ].
19. Feldmeyer L, Hofbauer GF, Böni T, French LE, Hafner J. Mammalian target of rapamycin (mTOR) inhibitors slow skin carcinogenesis, but impair wound healing. Br J Dermatol. 2011;166(2):422-4. doi: 10.1111/j.1365-2133.2011.10591.x. [ Links ]
20. Bravo IM, Correnti M, Escalona L, Perrone M, Brito A, Tovar V, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cir Bucal. 2006;11(1):E33-9. [ Links ]
21. Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein EB. The burdens of cancer therapy. Clinical and economic outcomes of chemotherapy-induced mucositis. Cancer. 2003;98(7):1531-9. doi: 10.1002/cncr.11671. [ Links ]
22. Sonis ST, Oster G, Fuchs H, Bellm L, Bradford WZ, Edelsberg J, et al. Oral mucositis and the clinical and economic outcomes of hematopoietic stem-cell transplantation. J Clin Oncol. 2001;19(8):2201-5. [ Links ]
23. Tomás I, Marinho JS, Limeres J, Santos MJ, Araújo L, Diz P. Changes in salivary composition in patients with renal failure. Arch Oral Biol. 2008;53(6):528-32. doi: 10.1016/j. archoralbio.2008.01.006. [ Links ]
24. Torres-Pereira C, Giovanini AF, Stramandinoli RT, Amenabar JM, Piazzetta CM. Oral paracoccidioidomycosis and pulmonary tuberculosis co-infection: relevance of oral biopsy in establishing the diagnosis and therapeutic approach. Int J of Infect Dis. 2009;13(1):114-6. doi: doi: 10.1016/j.ijid.2008.04.008. [ Links ]
25. Walsh LJ. Clinical assessment and management of the oral environment in the oncology patient. Aust Dent J. 2010;55 (Suppl 1):66-77. [ Links ]
26. Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. Dent Clin North Am. 2008;52(1):61-77. [ Links ]
27. Guggenheimer J, Eghtesad B, Stock DJ. Dental management of the (solid) organ transplant patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(4):383-9. doi: 10.1111/j.1834-7819.2010.01201.x. [ Links ]
 Correspondence to:
Correspondence to:
FAF OLIVEIRA
Rua Alexandre Baraúna, 949, Rodolfo Teófilo, 60430-160, Fortaleza, CE, Brasil
e-mail: arturforte@ymail.com
Received on: 3/4/2011
Final version resubmitted on: 5/11/2011
Approved on: 18/5/2012













