Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.7 no.2 Joinville Jun. 2010
SHORT COMMUNICATION
Allan AbuabaraI; Flares Baratto FilhoII; Rubia F. FuzzaIII
IDDS, Oral & Maxillofacial Radiology, Health Division, City Hall of Joinville, Joinville/SC, Brazil
IIPhD DDS, Professor of Positivo University, Curitiba/PR, and University of Joinville, Joinville/SC, Brazil
IIIMD, Neonatologist and Pediatrician at Dona Helena Hospital, Joinville/SC, Brazil
ABSTRACT
Thyroglossal duct cysts (TDCs) are cervical cysts occurring in approximately 7% of the population, mainly during childhood. The cyst usually presents itself as a painless, asymptomatic midline swelling below the hyoid bone. Differential diagnosis involves branchial cleft cyst, lymphoepithelial cyst, thyroid gland lesions, ranula and lymphadenopathy (of various etiologies). Sonogram (ultrasound) is the most frequent and appropriate imaging modality in suspected TDC. Preoperative fine-needle aspiration is an inexpensive and safe method that can be considered in selected adult patients, having prime importance to the exclusion of carcinoma. This article presents a TDC of the neck in a 5-year-old boy.
Keywords: Thyroglossal cyst; cystic duct; head and neck neoplasms.
Concept, epidemiology and pathogenesis
Thyroglossal duct cysts (TDC) are usually considered to be a benign embryonic malformation where the thyroglossal duct fails to obliterate after descent of the thyroid gland [3]. The thyroid gland is originally located in the floor of the pharynx, between the tuberculum impar (the first pharyngeal arch) and the copula (the second and third pharyngeal arches), during the 4th week of fetal life [11]. During development, the thyroid gland reaches its final position in front of the trachea and leaves the thyroglossal duct, a narrow canal with an epithelial lining along the descending route of the thyroid gland. Normally, the thyroglossal duct completely disappears before the 10th week [11, 13]. However, if the thyroglossal duct is not obliterated, the secretory epithelium of the thyroglossal duct may result in a TDC.
The TDCs are the second most common pediatric neck mass, behind adenopathy in frequency [4]. Thyroglossal duct remnants occur in approximately 7% of the population, although only a minority of these is ever symptomatic [4]. TDCs may be observed at any age, but most are noted during childhood, usually by 5 years of age. TDCs are present at birth in approximately 25% of cases; one third become apparent after the age of 30 [11]. Unlike most thyroid disorders in which females predominate, the gender incidence is equal for TDCs [11].
Clinical picture and management
TDCs can be found anywhere in the midline from the submental region to the suprasternal notch, but are most commonly located halfway between these extremes, near the hyoid bone [11]. Although they are most commonly found immediately adjacent to the hyoid (66%), they can also be located between the tongue and hyoid, between the hyoid and pyramidal lobe, within the tongue, or within the thyroid [6, 12].
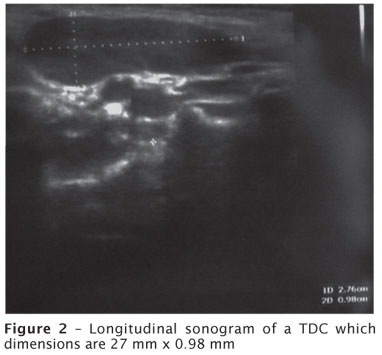
The cyst usually presents itself as a painless, asymptomatic midline swelling and may cause a neck mass or a nodule, which occasionally may become infected and rarely gives rise to carcinoma [11, 13]. In physical examination, TDCs present nodular neck that move upward with the thyroid gland when swallowed. The mass of TDCs usually moves with swallowing or protrusion of the tongue [1]. The figure 1 shows a typical suprahyoid TDC of the neck on a 5-year-old boy. Longitudinal sonogram confirmed the physical findings (figure 2).

Infection and abscess formation are frequent complications due to a communication between the cyst and the mouth with subsequent contamination by oral flora, which is the more common presentation in adults [7, 9]. One fourth of patients present with a draining sinus that result from spontaneous drainage or surgical drainage of an abscess [6]. This drainage can result in a foul taste in the mouth if the spontaneous drainage occurred by way of the foramen cecum. These lesions also fluctuate in size. Other rare presentations can be severe respiratory distress or sudden infant death syndrome due to lesions at the base of the tongue, a lateral cystic neck mass, an anterior tongue fistula, or coexistence with branchial anomalies [6].
Sonogram is the most frequent and appropriate imaging modality in suspected TDC [7]. Preoperative fine-needle aspiration (FNA) is an inexpensive and safe method that can be considered in selected adult patients, having prime importance to the exclusion of carcinoma, especially in adults [9]. The predominant cytopathological findings of TDCs are phagocytes, colloid, cholesterol crystals, and ciliated columnar epithelium. Thyroid tissue is rarely identified cytologically. Thus, FNA is indicated when malignancy is suspected, in the older patient group and those with larger TDCs [7]. FNA is not necessarily in the pediatric population. Elective surgical excision through Sistrunk procedure described in 1920 and modified in 1928 is the treatment of choice. This technique is based on the removal of the central portion of the hyoid bone. This procedure has successfully reduced the number of recurrences compared to local excision of the cyst [1, 7, 10].
Prognosis and complementary explorations
About 1% of the thyroglossal duct cysts are histologically malignant, but the prognosis is generally good [5, 8]. The neoplasia must be suspected in cases of thyroglossal duct cyst with recent changes in the clinical features. Imaging tests (sonogram, computer tomography) do not allow a preoperative diagnosis, and fine-needle aspiration yields a correct result in only 66% of the cases [2]. In addition, the diagnosis must distinguish between thyroglossal duct cyst carcinoma and metastasis from primary thyroid papillary carcinoma located in the pyramidal lobe. Histopathological examination is always necessary. Postoperative complications are usually minor. Differential diagnosis involves branchial cleft cyst, lymphoepithelial cyst, thyroid gland lesions, ranula and lymphadenopathy (of various etiologies) [13]. When a painless mass or nodule is found in the midline from the submental region to the suprasternal notch in a child and it moves with swallowing or protrusion of the tongue, TDC must be suspected and the patient be referred to a specialized physician for further investigations.
References
1. Acierno SP, Waldhausen JH. Congenital cervical cysts, sinuses and fistulae. Otolaryngol Clin North Am. 2007;40:161-76, vii-viii. [ Links ]
2. Bardales RH, Suhrland MJ, Korourian S, Schaefer RF, Hanna EY, Stanley MW. Cytologic findings in thyroglossal duct carcinoma. Am J Clin Pathol. 1996;106:615-9. [ Links ]
3. Cheng CY, Chang YL, Hsiao JK, Wang CP. Metachronous thyroglossal duct cyst and inferior parathyroid cyst: a case report. Kaohsiung J Med Sci. 2008;24:487-91. [ Links ]
4. Enepekides DJ. Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am. 2001;9:131-45. [ Links ]
5. Falvo L, Giacomelli L, Vanni B, Marzollo A, Guerriero G, De Antoni E. Papillary thyroid carcinoma in thyroglossal duct cyst: case reports and literature review. Int Surg. 2006;91:141-6. [ Links ]
6. Foley DS, Fallat ME. Thyroglossal duct and other congenital midline cervical anomalies. Semin Pediatr Surg. 2006;15:70-5. [ Links ]
7. Hirshoren N, Neuman T, Udassin R, Elidan J, Weinberger JM. The imperative of the Sistrunk operation: review of 160 thyroglossal tract remnant operations. Otolaryngol Head Neck Surg. 2009;140:338-42. [ Links ]
8. Martins AS, Melo GM, Tincani AJ, Lage HT, Matos PS. Papillary carcinoma in a thyroglossal duct: case report. Sao Paulo Med J. 1999;117:248-50. [ Links ]
9. Mohan PS, Chokshi RA, Moser RL, Razvi SA. Thyroglossal duct cysts: a consideration in adults. Am Surg. 2005;71:508-11. [ Links ]
10. Navas Molinero C, Sendra Tello J, Plaza Mayor G, Fragola Arnau C, Martínez San Millán J, Martínez Vidal A. Thyroglossal cyst: retrospective study of 58 cases. Results of the Sistrunk operation. Acta Otorrinolaringol Esp. 2000 May;51(4):340-7. [ Links ]
11. Organ GM, Organ Junior CH. Thyroid gland and surgery of the thyroglossal duct: exercise in applied embryology. World J Surg. 2000;24:886-90. [ Links ]
12. Pérez-Martínez A, Bento-Bravo L, Martínez-Bermejo MA, Conde-Cortes J, Miguel-Medina C. An intra-thyroid thyroglossal duct cyst. Eur J Pediatr Surg. 2005;15:428-30. [ Links ]
13. Shahin A, Burroughs FH, Kirby JP, Ali SZ. Thyroglossal duct cyst: a cytopathologic study of 26 cases. Diagn Cytopathol. 2005;33:365-9. [ Links ]
 Address for correspondence:
Address for correspondence:
Allan Abuabara
Rua Fernando Machado, 400 – ap. 201 – América
CEP 89204-400 – Joinville – SC – Brazil
E-mail: allan.abuabara@gmail.com
Received on April 23, 2009
Accepted on July 1, 2009













