Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.9 no.4 Joinville Out./Dez. 2012
Literature Review Article
Papillary regeneration: anatomical aspects and treatment approaches
Jaína Dias de Oliveira I ; Carmen Mueller Storrer II ; Andrea Maria Sousa III ; Tertuliano Ricardo Lopes IV ; Juliana de Sousa Vieira V ; Tatiana Miranda Deliberador VI
II Associate Professor, Positivo University – Curitiba – PR – Brazil
III MsC in Dentistry from the State University of Ponta Grossa – Ponta Grossa – PR – Brazil
IV Associate Professor, Positivo University – Curitiba – PR – Brazil
V Graduate Student of the Master Course in Dentistry from the Positivo University – Curitiba – PR – Brazil
VI Full Professor, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction and objective: This paper aims to report a literature review on the anatomy and morphology of the interproximal papilla and present the options of both surgical and nonsurgical treatment for the recovery of interdental papilla. Literature review: The loss of the interdental papilla because of the interproximal bone loss accounts for aesthetic, phonetic and functional problems of patients with periodontal disease. The interproximal tissue reconstruction has been reported in literature through both surgical procedures with the use of subepithelial connective tissue graft, restorative and orthodontic treatment. Conclusion: The etiology of gingival black space is multifactorial, therefore, it is important to diagnose properly the etiological factor to establish an appropriate treatment planing. However, the treatment approaches are not predictable and further studies are necessary to recommend the clinical practices available to date.
Keywords: dental papilla; gingival; regeneration.
Introduction
Currently a growing concern with beauty and physical appearance comes together with greater demands regarding to aesthetics in Dentistry. The gingival esthetics is one of the most important factors for success in a restorative treatment. The absence of interdental papilla as a result of the periodontal disease development or of the periodontal therapy used is a situation that leads to aesthetic, phonetic and food impaction problems. Papillary regeneration aims to fill the black spaces that occur in interproximal surfaces, one of the most complex cosmetic procedures to be performed among periodontal surgeries. Black triangles (spaces because of the darkened aspect of the oral cavity) occur in more than half of the adults. Therefore, this issue should be discussed with the patient prior to the initiation of dental treatment 32. The black spaces are not aesthetic and contribute for food retention as well as they may affect the periodontium health 22. A correct diagnosis should be performed for either the success or improvement of the treatment of papilla loss, as their etiological factors must be eliminated before considering therapies for reconstruction. In addition to act as a barrier to protect the periodontal structures, the papilla plays a critical role in the aesthetics. Therefore, it is very important to respect the papillary integrity during the dental procedures and minimize its disappearance 42.
The aim of this paper is to report a literature review on the morphological and anatomical aspects of interproximal papilla and present the periodontal, restorative and orthodontic therapeutic considerations about the recovery of interdental papilla.
Literature review
Papillary anatomy and morphology
The interdental space is the physical space present between two adjacent teeth, and its shape and volume are determined by the morphology of the teeth. The interdental papilla represents the gingival tissue that fills this space and is formed by dense connective tissue covered by oral epithelium and may be influenced by the height of the alveolar bone, distance between the teeth and interdental contact point 32.
In the area of the incisors, the interdental papilla is narrow and has a pyramidal shape with its tip just below the point of contact. In the posterior region, it is wider and with a ridgeshaped concave area so-called the col 10. This crest, which determines the position and extent of the contact point of the adjacent teeth, is nonkeratinized or parakeratinized and covered with stratified squamous epithelium 16.
The contact point on the maxillary central incisors is located at the incisal third of the labial aspect, between the central incisors; the contact point on the maxillary lateral incisor is located in the middle of this teeth and between the lateral incisor and canine at the apical third 24. This means that the most visible papilla, located on the upper central incisors, is filled with more space than the others, and its lack causes major aesthetic problems. It is therefore more difficult to be reconstructed.
The classical study conducted by Tarnow et al. 37 correlated the presence or absence of interdental papilla with the distance between the bone crest and the contact point at 288 interproximal sites in 30 patients. The presence of the papilla was observed in almost 100% of the cases in which the distance was less than or equal to 5 mm, in 56% of cases in which the distance was 6 mm, and only 27% of cases in which the distance was 7 mm or more.
According to Fradeani 11, the distance between the roots is another factor that can influence the presence or absence of interdental papilla. The author stated that the a inter-radicular distance smaller than 0.3 mm jeopardizes the presence of the proximal bone and, therefore, it is usually accompanied by the lack of interdental papilla.
The gingival black space has been defined as a distance from the cervical black space to the interproximal contact 18. A smile with gingival black spaces affects the aesthetic of the patient. Kokich 20 observed that the gingival space larger than 3 mm is considered a visible aesthetically problem both for the dentists and the general population.
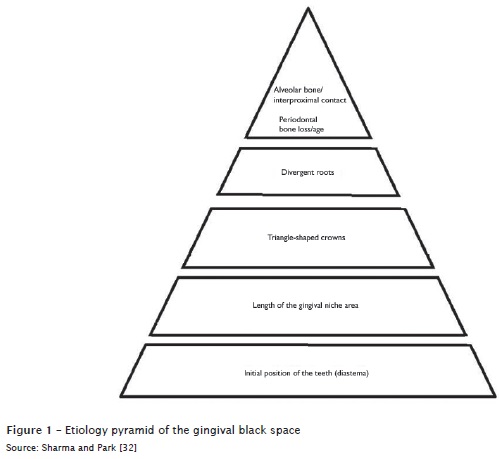
Etiological factors for papilla absence
The etiology of the papilla absence of is multifactorial (figure 1). The causes include changes in papilla during orthodontic alignment, loss of periodontal ligament resulting in recession, loss of alveolar bone height in relation to the interproximal contact, length of the area of the niche, root angle, and positioning of the interproximal contact and triangle-shaped crowns.
The periodontal disease has been associated with loss of interdental papilla due to the loss of alveolar bone 42. Additionally to the periodontal disease, other factors such as the host susceptibility, are involved in gingival black space. The distance of 5 mm from the alveolar crest to the contact point is considered periodontally healthy 42. However pockets with probing depth greater than 3 mm will lead to an increasing of plaque retention, inflammation and recession 42. In the periodontal disease, the alveolar bone loss increases the distance between the contact point and the alveolar crest resulting in a space black.
In the study of Wu et al. 41 it was demonstrated that the distance of 5, 6 and 7 mm resulted in a gingival black space of 2.44% and 73% of the cases, respectively. This indicates that if the alveolar crest distance to the contact point is equal to or less than 5 mm, the papilla will be present in almost 100% of cases. If the distance is greater than 7 mm, there will be papilla in most cases. At 6 mm, the papilla is present in about half of the cases. An increase of 1 mm in the distance between the alveolar bone and the interproximal contact increases the probability of a gingival black space from 78% to 97%. As a rule, the distance between 5 and 6 mm is the most critical and it determines the presence or lack of space in the gingival embrasure 41.
Currently, the study of Chen et al. 8 demonstrated that the presence of papilla is significantly related to the distance from the contact point to the bone crest, that is, the smaller this distance, the smaller the distance between two adjacent teeth; the lower the area of the gingival niche, the more likely is the presence of interdental papilla. The authors reported that the interdental papilla is more present in rectangular-shaped teeth. According to these same authors 8, the loss of bone height may be the crucial factor in the loss of interdental papilla. However, it is unclear whether the position change of the contact point to reduce the distance between the contact point and the bone crest would help the recovering of the interdental papilla 8.
The brushing trauma can also causes gingival black spaces. If the loss of papilla height is caused by trauma during brushing, the aggressively cleaning of the interproximal tissue should be interrupted so that the tissue could be recovered 35.
The presence of gingival black spaces can also be related to age. The studies of Ko-Kimura et al. 18 showed that patients over 20 years-old are more likely to gingival black space than those under 20 years-old. Gingival spaces were found in 67% of the population over 20 years-old; in the population under 20 years-old, the percentage reached 18%. This is because of the thinning of the oral epithelium, decreasing of the keratinization and a reduction in the height of the papilla as the result of age.
Classification of the interdental papilla loss
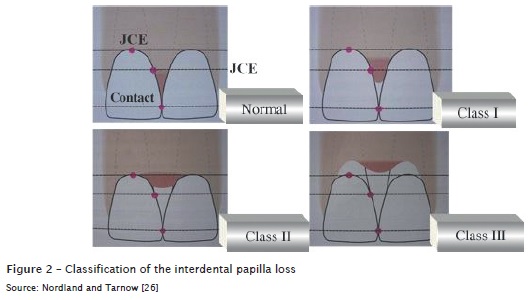
The interdental papilla loss was classified by Nordland and Tarnow 26. This classification is based on three anatomic points: the interdental contact point, the most coronal point of the enamelcementum junction (ECJ) at the interproximal surface and the most apical point of the ECJ at the labial surface. Four classes were identified (figure 2):
• Normal: the interdental papilla fills the niche up to the apical extension of the interdental contact point;
• Class I: the tip of the interdental papilla is placed between the interdental contact point and the most coronal point of the ECJ at the interproximal surface;
• Class II: the tip of the papilla is placed between the most coronal point of the ECJ at the interproximal surface and the most apical point of ECJ at the labial surface;
• Class III: the tip of the interdental papilla is at the ECJ or it is apically to the most apical point of ECJ at the labial surface.
Treatment approaches
Some methods may be used in an attempt to achieve the reconstruction of interdental papilla, including manipulating soft tissue 2, increasing of the hard tissue 5 and the restorative and orthodontic treatment 24.
Techniques of soft tissue manipulation
If the loss of papilla is related to only soft tissue loss, reconstruction techniques are capable of restoring it completely. If the loss of papilla is caused by periodontal disease with interproximal bone resorption, usually a complete reconstruction is not achieved. Surgical and non-surgical considerations are proposed in the periodontal literature to provide a satisfactory reconstruction of the interdental papilla.
Non-surgical considerations
In cases of the interdental papilla damage performed by traumatic brushing, the interdental hygiene should be modified. The re-epithelialization of traumatic injuries can completely restore the papilla 1.
Surgical considerations
Currently there is no predictable surgical procedure to retrieve the interdental papilla 29. Reconstructive surgery can result in contraction of papillary necrosis and of the grafted tissue due to the fragility of the tissue and low blood supply in the region 41.
Among the surgical techniques, it may be used pedicle flaps, free gingival and connective tissue graft 23,31. Some case reports have demonstrated success with subepithelial connective tissue graft and orthodontic therapy 7,25. According to Wu et al. 41, the flap surgery has shown better results than the free gingival graft. Grupe et al. 14 stated that the techniques with pedicle flaps showed better results than free gingival graft techniques, because the blood supply is provided by the base of the pedicle. In 1996, Han and Takei 15 described a technique in which the interdental papilla was moved and placed coronally and a connective tissue graft was placed below the papilla. This technique is based on a model previously described by Tarnow 36. A half-moon shaped incision was made parallely to the labial free gingival margin and the flap dissected was coronally positioned to cover an exposed root. In their modification for reconstruction of the papilla, they recommended the execution of the semilunar incision in the interdental region to allow the restoration of the lost interproximal papilla by placing a connective tissue graft below the deficient area. According to the authors, this procedure must be repeated a second or third time after two or three months of healing. This technique 15 was applied in a patient with an implant onto the area of the maxillary central incisor. The mesial and distal papillas were absent. After the placing of a provisional prosthesis, there was a small improvement in the interdental region. The semilunar and intrasulcular incision was executed to release the connective tissue of the root surface and the papilla was coronally placed. The subepithelial connective tissue graft was removed from the palate and placed in the space created by the displacement. The gain of interdental tissue was observed after the wound healing and also after the period of healing of three and four months.
In 1998, Azzi et al. 2 reported a papilla reconstruction using subepithelial graft associated with a partial thickness flap. The partial flap is raised in the labial and palatal graft to allow the placement of the conjunctive graft removed from the area of the tuberosity. The graft is trimmed to the ideal size and shape and placed under the flap to provide more volume in the papillary region. The labial and palatal flaps are sutured together and subepithelial graft lies beneath them.
In 1999, Azzi et al. 3 described another technique to achieve root coverage and papilla reconstruction of a recession. In this case, the incision is performed near to the mucogingival junction, preserving the integrity of the cervical region, again involving the connective tissue graft removed from the maxillary tuberosity. The connective tissue and the flap displacement allowed the simultaneous treatment of the gingival recession and loss of interproximal papilla. In 2001, to increase the volume of the interdental tissue additional to the f lap described in the aforementioned study, Azzi et al. 4 associated an autogenous bone graft from the region of the maxillary tuberosity with a connective graft tissue from the region of the palate.
In the study published by Pellegrine et al. 28, it was presented a case in which there is a reconstruction of the interdental papilla by modifying the technique of interdental papilla preservation presented by Takei et al. 34 associated with the subepithelial connective graft. In this case, it was shown the possibility of folding the graft to obtain a larger increase in the volume; procedure used in surgery for alveolar ridge thickness augmentation with possible applications in the field of papillary reconstruction 15.
Techniques of hard tissue augmentation
This type of procedure is not commonly used because, although the guided bone regeneration or bone grafts are used to increase the height of the alveolar bone, these procedures are limited in the interdental area 5.
Restorative treatment
Concerning to the restorative treatment, one of the options is to change the position of the point of contact with ceramic veneer or crown. Further, it is possible to add pink porcelain onto the restoration to mask the loss of interdental papilla 42. Moreover, mesial-cervical restorations or laminates will reduce the appearance of gingival by altering the shape of the crown. The composite can be inserted near the gingival sulcus to guide the format of the interdental papilla 32.
Another method of correcting the black space is the interproximal enamel reduction, made with a diamond strip to reshape the mesial surface of the maxillary central incisor. Approximately 0.5 to 0.75 mm of enamel is removed by interproximal reduction 19, which will increase the contact point and move it gingivally. The interproximal enamel reduction in teeth with triangular crowns will change the point of contact for a larger area, reducing the gingival embrasure 32.
Orthodontic treatment
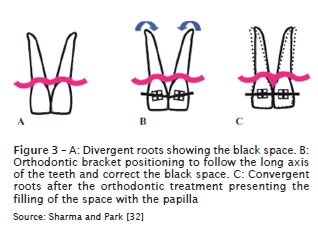
The orthodontic treatment to put the contact point more apically can be executed attempting to reduce the black triangle (figure 3). Further, the alveolar bone height and papilla can be induced by orthodontic extrusion 17.
Divergent roots are associated with the gingival black spaces. With the orthodontic treatment, the maxillary central incisors can follow the axial long axis of the tooth and correct the black space. As the roots become more parallel, the contact point will stretch and move towards the apex of the papilla 41.
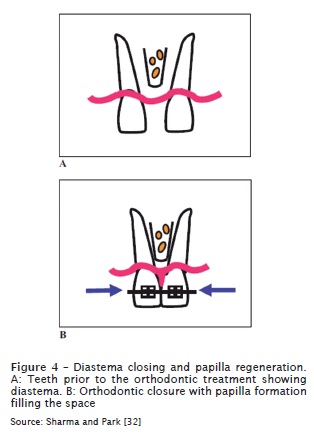
As the crowns of each incisor approach, the stretched transeptal fibers relax and fill the gingival embrasure 19, reducing their probability and severity. When a diastema occurs because of the periodontal disease, its orthodontic closure can be performed after the resolution of inflammation. In such cases, the reconstruction of the interdental papilla is not the main goal of the treatment planing. The volume of soft tissue in the interproximal space will depend on the amount of existing tissue, bone levels and severity of the diastema. The diastema closure through orthodontic treatment will compress the soft tissue and thus fill the gap 32 (figure 4).
Loss of interproximal papilla in the treatment with dental implants
Single implants have a significant chance of losing papilla due to the increase of the distance from the contact point to the alveolar crest. To preserve the papilla in the implant, it is important to keep the distance from the point of contact to the bone level of 5 mm or less. The distance from the adjacent natural tooth to the alveolar crest is more critical than that from the height of the contact point of the implant to the bone 9.
Black spaces are even more pronounced when two adjacent implants are placed. This deficiency in the soft tissue of 1 to 2 mm arises from the biological space around the implant abutment apically to the abutment platform 38. As a result, the biologic space of the implant is located below rather than above the bone crest, as in the case of natural teeth. Ideally, maxillary anterior implants should be at 4 mm apically to the alveolar bone crest. Furthermore, to prevent bone loss and thereby the papilla loss, it is important that the distance between the two implants is of 3 mm 30. This allows that the interproximal bone be held above the implant platform. In the anterior region, it is difficult to obtain this ideal mesial-distal distance. A method for compensating the interproximal bone loss is the increase of the palatal bone in the papilla area 13. However, a distance of ≥ 3 mm will not ensure the presence of interproximal papilla.
There are several considerations that do not allow the papilla regeneration, but they help in preventing the interproximal bone loss and in the aesthetic achievement. One of the options for the treatment of the loss of two teeth that will be replaced by implants in an aesthetic area, it is to install just one implant and to construct a cantilevered prosthesis associated with soft tissue graft and interproximal bone augmentation 39.
Discussion
The presence of interdental papilla is of extremely important in the esthetic gingival factor in this patient's smile. The loss of interdental papilla is caused by the loss of interproximal bone, resulting from the periodontal disease advancement or history of the therapy used (surgical or nonsurgical). However, such factors as trauma brushing, diastema and presence of divergent roots may be related to papilla loss and therefore must also be corrected.
One of the factors that most influence on the presence of the papilla is the distance between the bone crest and the contact point, and the papilla is always present when this distance is of 5 mm or less 37.
The most common treatment approaches used have been the surgical procedures. Among them, the cases successfully described in the literature include connective tissue graft 7,25.
For the surgery success, it is important the presence of a thick gingiva without insertion loss 35. Patients with thinner gingival biotype are more susceptible to recession and therefore interproximal black space.
Patients with thin periodontium usually have long and narrow central incisors, while patients with thicker gingiva have wider and smaller central incisors 27. Furthermore, the periodontal biotype demonstrates a dense bone structure with flat morphology and thick gingiva with short and wide papilla. In contrast, the thin gingival biotype is characterized by a bone appearance with long interdental papilla 6. Typically, the thick gingival biotype has better vascular supply and biological tissue memory that helps the tissue to recover, while the thin biotype usually results in a permanent recession 40.
Another treatment option reported in the literature is the association between the restorative and surgical treatment, through the use of prosthesis for conditioning the gingival tissue. In addition, the orthodontic treatment is successful with the orthodontic extrusion to obtain the increase of the alveolar bone height 17, through the alignment of the roots following the long axis of the teeth 41 and the diastema closure 32. On the other hand, the manipulation techniques of hard tissue are not yet viable.
Although there are surgical and non-surgical techniques for reconstruction of interdental papilla, there are no treatments to achieve predictable success.
Conclusion
The etiology of the gingival black space is multifactorial and it is important to diagnose properly the etiologic factor for establishing an appropriate treatment planing. However, the treatment approaches are not predictable and further studies are needed to recommend the clinical practices available to date.
References
1. Agudio G, Pini Prato GP, Nevins M, Cortellini P, Ono Y. Esthetic modifications in periodontal therapy. Int J Periodontics Restorative Dent. 1989;(9):288-99. [ Links ]
2. Azzi R, Etienne D, Carranza F. Surgical reconstruction of the interdental papilla. Int J Periodontics Restorative Dent. 1998;(18):467-73.
3. Azzi R, Etienne D, Sauvan J, Miller PD. Root coverage and papilla reconstruction in class IV recession: a case report. Int J Periodontics Restorative Dent. 1999;(19):449-55.
4. Azzi R, Takei HH, Etienne D, Carranza F. Root coverage and papilla reconstruction udingautogenous osseous and connective tissue grafts. Int J Periodontics Restorative Dent. 2001;(21):141-7.
5. Blatz MB, Hurzeler MB, Strub JR. Reconstruction of the lost interproximal papilla- presentation of surgical and nonsurgical approaches. Int J Periodontocs Restorative Dent. 1999;(19):395-406.
6. Chang L. The association between embrasure morphology and central papilla recession: a noninvasive assessment method. Chang Gung Med J. 2007;(30):445-52.
7. Checchi L, Montevecchi M, Checchi V, Bonetti A. A modified papilla preservation technique, 22 years later. World J Orthod. 2009;(40):303-11.
8. Chen M, Liao Y, Chan C, Ku Y, Pan W, Tui Y. Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol. 2010;81(2):318-24.
9. Choquet V, Hermans M, Andriaenssens P, Hermans M, Abraham I, Prestipino V et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;(72):1364-71.
10. Cohen B. Pathology of the interdental tissues. Dent Pract. 1959;(9):167-73.
11. Fradeani M. Esthetic analysis: a systematic approach to prosthetic treatment. Quintessence Books; 2004.
12. Prato GP, Rotundo R, Cortellini P, Tinti C, Azzi R. Interdental papilla management: a review and classification of the therapeutic approaches. Int J Periodontics Restorative Dent. 2004 Jun;24(3):246-55.
13. Grunder U, Spielman H, Gaberthuel T. Implant-supported single tooth replacement in aesthetic region: a complex challenge. Pract Periodont Aesthet Dent. 1996;(8):835-42.
14. Grupe HE, Warren RF. Repair of gingival defects by a sliding flap operation. J Periodontol. 1956;(27):92-5.
15. Han TJ, Takei HH. Progress in gingival papilla reconstruction. Periodontol 2000. 1996;(11):65-8.
16. Holmes CH. Morphology of the interdental papillae. J Periodontol. 1965;(36):455-9.
17. Inhgher JS. Forced eruption: alteration of soft tissue cosmetic deformities. Int J Periodontics Restorative Dent. 1989;(9):417-25.
18. Ko-Kimura N, Kimura-Hayashi M, Yamaguchi M, Ikeda T, Meguro D, Kanekawa M et al. Some factors associated with open embrasures following orthodontic treatment. Aust Orthod J. 2003;(19):19-24.
19. Kokich V. Esthet ics: the orthodont icperiodontic restorative connection. Semin Orthod. 1996;(2):21-30.
20. Kokich V. Excellence in finishing: modifications for the perio-restorative patient. Semin Orthod. 2003;(9):184-203.
21. Kokich V, Kiyak A, Shapiro P. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 2005;(1):311-24.
22. Kurth J, Kokich V. Open gingival embrasures after orthodontic treatment in adults: prevalence and etiology. Am J Orthod Dento Facial Orthop. 2001;(120):116-23.
23. Langer B, Calanga L. Subepithelial connective tissue graft. J Prosthetic Dent. 1980;(44):363-7.
24. Miller PD, Allen EP. The development of periodontal plastic surgery. Periodontol 2000. 1996;(11):7-17.
25. Newcovsky C. Interproximal papilla augmentation prodecure: a novel surgical approach and clinical evaluation of 10 consecutive procedures. Int J Periodontics Restorative Dent. 2001;(21):553-9.
26. Nordland WP, Tarnow DP. A classification system for loss of papillary height. J Periodontol. 1998;69(10):1124-6.
27. Olsson M, Lindhe J, Marinello CP. On the relationship between crown form and clinical features of the gingival in adolescents. J Clin Periodontol. 1993;(20):570-7.
28. Pellegrine AA, Okajima LS, Henriques PSG, Ferraz AP, Giannini M. Reconstrução da papila interdental – uma abordagem cirúrgica/ r e s tauradora. Re v As soc Paul Ci r Dent . 2006;60(2):148-54.
29. Ravon N, Handel sman M, Lev ine D. Multidisciplinary care: periodontal care aspects to treatment planning in the anterior esthetic zone. J Calif Dent Assoc. 2008;(36):575-84.
30. Ryser M, Block M, Mercadante D. Correlation of papilla to crestal bone levels around single tooth implants in immediate or delayed crown protocols. J Oral Maxillofac Surg. 2005;(63):1184-95.
31. Saraiva JA, Campos EA, Cavassim R, Pinto SCS, Fontanari LA, Oliveira GJPL et al. Subepithelial connective tissue graft: a case report. RSBO. 2011;8(3):357-62.
32. Sharma AA, Park JH. Esthetic considerations in interdental papilla: remediation and regeneration. J Esthet Restor Dent. 2010;(22):18-30.
33. Silva RC, Carvalho PFM, Joly JC. Planejamento estético em periodontia. eBook 25 CIOSP Jan 2007:300-41.
34. Takei H, Yamada H, Hau T. Maxillary anterior esthetics: preservation of the interdental papilla. Dent Clin of North Am. 1989;(33):263-73.
35. Tanaka OM, Furquim B, Pascotto C, Ribeiro GL, Bosio JB, Maruo I. The dilemma of the open gingival embrasure between maxillary central incisors. J Contemp Dent Pract. 2008;(9):1-9.
36. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol. 1986;13(3):182-5.
37. Tarnow D, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of interproximal dental papilla. J Periodontol. 1992;63(12):995-6.
38. Tarnow D, Cho S, Wallace S. The effect of interimplant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-9.
39. Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74(12):1785-8.
40. Van der Velden U. Regeneration of the interdental soft tissue following denudation procedure. J Clin Periodontol. 1982;9(6):455-9.
41. Wu YJ, Tu YK, Huang SM, Chan CP. The influence of the distance from the contact point to the crest of bone on the presence of interproximal dental papilla. Chang Gung Med J. 2003;26(11):822-8.
42. Zetu L, Wang Z. Management of interdental/ inter- implant papi l la. J Cl in Periodontol . 2005;32(7):831-9.
 Correspondence:
Correspondence:
Tatiana Miranda Deliberador
Mestrado Profissional em Odontologia Clínica, Universidade Positivo.
Rua Professor Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: tdeliberador@gmail.com













