Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.1 Joinville Jan./Mar. 2013
CASE REPORT ARTICLE
Oral Kaposi's sarcoma in immunosuppressed patients – report of cases
Allana PivovarI; Cassiano Lima ChaibenI; Francisca Berenice Dias GilII; Antonio Adilson Soares de LimaI
IDepartment of Stomatology, School of Dentistry, Federal University of Paraná – Curitiba – PR – Brazil.
IIDepartment of Dentistry, Oswaldo Cruz Hospital – Curitiba – PR – Brazil.
ABSTRACT
Introduction: Kaposi sarcoma is a vascular neoplasm composed of endothelium-lined vascular spaces and spindle-shaped cells. It often manifests with multiple vascular nodules on the skin and other organs. Kaposi sarcoma is rare in HIV negative patients and it is associated with HHV-8 infection. There are four types: classic, endemic, iatrogenic and HIV-associated. Patients with HIV/AIDS are also at increased risk of developing Kaposi sarcoma.
Objective: The aim of this article is to present two cases of Kaposi sarcoma in the hard palate of HIV/AIDS male patients.
Case report and conclusion: Kaposi sarcoma should be considered in the differential diagnosis of any AIDS patient who presents with bluish, smooth, firm, nonpulsatile macule or nodule in the region of the hard palate. Development of Kaposi sarcoma in the oral cavity also has prognostic implications for untreated HIV patients, who are found to have higher death rates than patients affected only by cutaneous disease.
Keywords: Kaposi sarcoma; acquired immunodeficiency syndrome; oral mucosa.
Introduction
Kaposi's sarcoma is a neoplasm of vascular endothelium that is characterized by proliferation of spindle cells, neoangiogenesis, inflammation and edema 17. Moritz Kaposi, a Hungarian dermatologist in 1872, first described it. Since then, this disease can be classified into four different clinical forms that have identical histologicalfeatures, but affecting specific populations. Lesions appear in different areas of the body and have a different clinical progression 18,30.
In his original article entitled "Idiopathic multiple sarcoma of the skin", Moritz Kaposi described the indolent and rare disease that is known as classic or sporadic Kaposi sarcoma. This clinical form is characterized by single or multiple lesions that are usually located in the lower extremities and affects elderly men 28. The endemic form of Kaposi's sarcoma, present in Africa (mainly in the south of the Sahara Desert), is relatively rare, but more aggressive. It affects young adults and black children 7. The iatrogenic form emerged with the advent of organ transplantation and immunosuppressive therapy, as well as the emergence of chemotherapy. Additionally, there is epidemic form that is associated with acquired immunodeficiency syndrome.
Epidemiological studies suggest that the disease is infectious, mainly associated with human herpes virus type 8 (HHV-8). In vitro studies show that the virus can infect various cell types such as endothelial cells and B-lymphocytes 15. It is believed that HHV-8 is transmitted sexually. Most reports on the epidemic of Kaposi sarcoma has been described in homosexual men and very few cases have been reported among heterosexual men. The receptive anal sex is a significant risk factor 23.
Initially, the most common site of involvement is the skin 11. However, in some cases, there is no cutaneous involvement or it is preceded by visceral, oral or ganglion lesions 21. Skin lesions can be macular, plate-shaped, nodular or papules. Its length may vary from a few millimeters to large confluent plaques or nodules of ten centimeters or more 14,21. The color of the lesions can range from dark pink, red, purple or brown 15.
The average age of patients with Kaposi sarcoma/AIDS is 38 years-old; with 69% of cases occurring between the ages of 30 to 39 years. The ratio of affected men and women varies from 50 to 100:1. Six percent of children with HIV (+) develop the disease, and 8% of seropositive women. About 15% of all diagnosed cases of AIDS have associated Kaposi sarcoma 4.
Kaposi sarcoma is one of the first recognized opportunistic diseases in HIV infection and is still the most common malignancy associated with AIDS 32. The purpose of this paper is to present two cases of Kaposi sarcoma in its epidemic form in HIV positive patients.
Report of cases
Case 1
A white, male patient, 24 years old, was referred by an ophthalmologist to the Oswaldo Cruz Hospital (Curitiba/PR/Brazil) with an indication of treatment for uveitis by cytomegalovirus. The main complaint of the patient was the loss of visual acuity with greater intensity in the left eye. The patient was HIV positive since 2008 and was initially diagnosed with tertiary syphilis. However, subsequently, the clinical and laboratory findings revealed that it was toxoplasmosis.
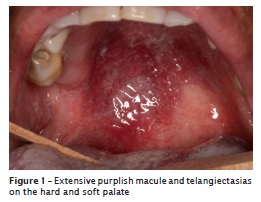
The dental examination revealed absence of some teeth and darkening of the clinical crown in the maxillary central incisors. According to the patient, the pigmentation of the tooth occurred after the endodontic treatment. The teeth #14, #24 and #25 had advanced caries and had an indication for endodontic treatment. Clinical examination also revealed the presence of erythematous candidiasis in the soft palate and purplish lesions suggestive of Kaposi's sarcoma in the hard palate (figure 1). Additionally, several telangiectasias were seen on the surface of the lesion.
Laboratory tests revealed a CD4 count equal to 324/mm3 (18.39%) and an ESR of 15 mm. The renal function tests had the following results: GOT = 15, GPT = 40, creatinin = 1.0 mg/dL and urea = 22.2 mg/dL. The result of the blood count was as follows: erythrocytes = 4.77 M/mL, hemoglobin = 13.4 mg/dL, hematocrit = 41.2%, leukocytes = 5.400 and lymphocytes = 25. The platelet count was equal to 269.000 and the determination of glucose = 70 mg/dL. Inaddition, patients had antibodies to type 1 and 2 herpes virus.
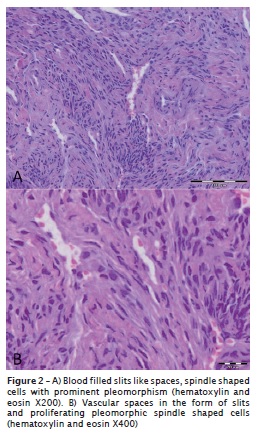
Oral candidiasis was initially treated successfully by Fluconazole (200 mg/day for 14 days). An incisional biopsy was performed in the palatal region close to the teeth #17 and #18. Then, tissue sample was sent for pathological examination at the Clinical Hospital of UFPR. The result showed a kaposiform vascular proliferation that confirmed the clinical hypothesis of Kaposi sarcoma (figure 2A and 2B). Then, the patient was submitted to upper endoscopy for staging of Kaposi's sarcoma and no lesion was found in the upper gastrointestinal tract. The patient was classified as poor risk according to the staging classification system for AIDS-related Kaposi proposed by the AIDS Clinical Trial Group. The patient received a referral for an infectious diseases consultation for the initiation of highly active antiretroviral treatment (HAART).
Case 2
A white male patient, 47 years old, was admitted to the Oswaldo Cruz Hospital (Curitiba / PR/Brazil) with fever, diarrhea, asthenia, anemia, thrombocytopenia, and edema of lower limbs. The patient was diagnosed with HIV infection and had a history of alcoholism and crack use.
Laboratory tests revealed a CD4 count equal to 324 (18.39%) and an ESR of 135 mm. The renal function tests had the following results: GOT = 19, GPT = 7, creatinin = 0.80 mg/dL and urea = 29 mg/dL. The result of the blood count was as follows: erythrocytes = 2.97M/mL, hemoglobin = 9.0 mg/dL, hematocrit = 26.3%, leukocytes = 7.4 and lymphocytes = 25. The platelet count was equal to 64 k/mL and the determination of glucose = 70 mg/dL.
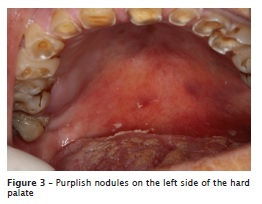
The physical examination revealed the presence of smoker's melanosis, cervical caries and wear of incisal and occlusal surfaces of teeth due to bruxism. Some purple, painless and slightly higher lesions were observed in the posterior region of the hard palate (figure 3). The patient was unaware of the presence of lesions. Thus, he could not specify the period of the appearance of them.
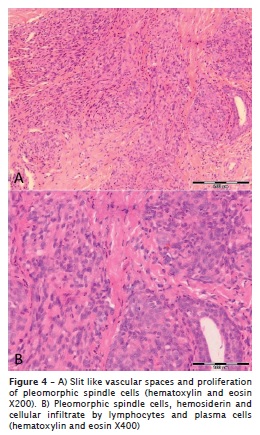
The patient underwent an incisional biopsy. The fragment of the lesion was examined at the Clinical Hospital of UFPR. The histological sections showed an atypical spindle cell proliferation consistent with the clinical hypothesis of Kaposi sarcoma (figure 4A and 4B). The patient was classified as poor risk according to the staging classification system for AIDS-related Kaposi sarcoma because he exhibited the following changes: edema (swelling) due to the tumor, and extensive oral Kaposi sarcoma in other organs (lungs). The patient was referred for treatment of Kaposi sarcoma at another hospital specializing in cancer treatment, but he died of respiratory complications.
Discussion
The World Health Organization (WHO) identified HIV/AIDS as the world's most urgent public health challenge, because AIDS represents the greatest lethal epidemic in recent history. In HIV infected individuals, opportunistic viral infections are the major cause of morbidity and mortality. These agents cause infections which could be asymptomatic or mildly symptomatic in immunocompetent individuals, and it is often self-limiting. However, in immunosuppressed individuals and individuals with malignancy, infection with these agents leads to severe life-threatening diseases 25. The increasedfrequency and severity of diseases caused by these viruses in HIV-infected individuals is due mainly to dysfunction of both the adaptive and innate immune responses to viral pathogens 33.
One of the first HIV-related cases of Kaposi sarcoma was seen at San Francisco General Hospital in 1981. At this time, the Kaposi sarcoma tumor was rarely seen in the United States, and it was a complete surprise in young, previously healthy men. This was the beginning of the HIV/AIDS epidemic. This case was notable for multiple skin lesions and nearly confluent lesions on the inner thighs 22. Kaposi sarcoma is one of the most common cancers caused by an infectious agent 13.
Four groups are at risk to develop Kaposi sarcoma: elderly males of Mediterranean and Eastern European lineage; children and adults from central Africa; persons who are iatrogenically immune compromised; and homosexual men infected with human immunodeficiency virus 1. In both cases reported in this article, the Kaposi sarcoma was seen in patients with HIV-related immunosuppression. It seems that the route of HHV-8 transmission may be both sexual and nonsexual. Furthermore, the pathogenesis of Kaposi sarcoma is uncertain. Recent studies showed an association between all types of Kaposi sarcoma and infection with HHV-8, known as KS-associated herpes virus (KSHV) 12.
Kaposi sarcoma in HIV/AIDS patients, presents as purple macules or nodules. The lesions are painless and the hard palate is the most common location in the mouth 19. The two patients described in this article have developed multiple purple lesions on the hard palate. Surprisingly, no lesions were observed in skin. However, the oral cavity is the first clinical site of disease in 22% of patients with Kaposi sarcoma, and up to 71% of HIV patients may develop oral Kaposi sarcoma concurrent with cutaneous and visceral involvement 25.
The clinical appearance of the oral Kaposi sarcoma may generate doubts about the diagnosis, because there are other lesions that are similar. The differential diagnoses for oral lesion include pyogenic granuloma, histiocytoma, hemangioma, angiosarcoma, bacillary angiomatosis, cutaneous lymphoma, linfangioendotelioma benign acroangiodermatitis, spindle cell hemangioendothelioma, angiolipoma and aneurysmal fibrous histiocytoma 5,36. Thus, oral biopsy and histopathological findings are essential for definitive diagnosis.
The following histopathological findings are observed in Kaposi sarcoma: blood filled slit like spaces, pleomorphic spindle cells with frequent mitoses, extravasated erythrocytes, hemosiderin laden macrophages and cellular infiltrate by lymphocytes and plasma cells 6. In Kaposi sarcoma, cells that normally line small blood vessels proliferate in an abnormal way, extending outward from what would have been the lining of the vessel to penetrate between and partially surround nearby collagen bundles, thus creating "stellate" and "ecstatic" blood vessels that are not closed off but rather are open to surrounding tissue 31. In addition, immunohistochemical staining (CD34 antibody) may be done for further diagnosis. It yields positive results for endothelial lining of slit like spaces and for spindle cells 2,31. The incisional biopsy was performed in two patients and histopathological examination confirmed the diagnosis of Kaposi sarcoma. The labeling immunohistochemistry was unnecessary, since the histopathology was evident.
Cancer staging is the process of using physical exams, imaging tests, and, in some cases, biopsy results to determine where and how much cancer is in the body. For many types of cancer, the stage is the most important factor in selecting treatment options and predicting a patient's outlook for recovery and survival. In 1988 a group of researchers known as the AIDS Clinical Trials Group (ACTG) proposed a staging classification system for AIDS-related Kaposi sarcoma 33. The ACTG system considers three factors: i) The extent of the tumor, ii) The status of the immune system , as measured by the number of certain cells (CD4 cells) present in the blood, and iii) The extent of involvement within the body or systemic illness. In this context, the clinical findings revealed that both patients had poor risk.
There are multiple treatment modalities described in literature including, local surgical excision, cryotherapy, electrosurgery, chemotherapy, laser therapy and radiation therapy, HAART, besides adjuvant treatment with intralesional or systemic injections with cytostatic agents, alpha- and beta-interferon, photodynamic therapy and topical therapy in form of nitrogen mustard or imiquamod 33. For small and single lesions, surgical excision may be recommended 24. Local recurrence is rare after complete excision of the primary lesion. When present, relapse occurs from six months to two years after the procedure 16,24,33. Indications for systemic therapy include (i) Visceral involvement, (ii) Extensive Kaposi sarcoma associated with lymph edema, (iii) Extensive and rapidly progressing Kaposi sarcoma and, (iv) Failure to respond to local therapy 35.
The neoplasms related to KSHV best illustrate the interplay between malignancy, infection and immunity 3. Kaposi sarcoma is approximately 100 times more common during immunosuppression and can be resolved when iatrogenic immunosuppression is stopped and during HAART of HIV-1 infected individuals 3,8. However, the success of HAART in ameliorating Kaposi sarcoma likely is attributable not only to immune restoration, but also to the concomitant reduction in HIV-1 load 29,37. In case 1, the patient was treated with anti-retroviruses. The second patient died before receiving some kind of treatment for the Kaposi sarcoma.
The involvement of the oropharynx occurs in about one third of patients with Kaposi sarcoma and is most frequent lesion in the palate. Furthermore, this disease may also involve the gums, tongue, tonsils, pharynx and trachea 10. Development of Kaposi sarcoma in the oral cavity may cause local tissue damage, pain, bleeding, or interference with oral functions and prosthesis wear, all of which may negatively affect a patient's nutritional status, adherence to medical therapy, and quality of life. Therefore, oral lesions clinically suggestive of Kaposi sarcoma should be biopsied and patients with biopsy-proven Kaposi sarcoma should be tested for HIV 9. Thus, the dentist should be familiar with orofacial manifestations of Kaposi sarcoma, contribute to prevention of this disease by educating patients about risk factors, and question those engaged in risk behaviors about the presence of mucocutaneous lesions.
References
1. Antman K, Chang Y. Kaposi's sarcoma. N Engl J Med. 2000;342:1027-38. [ Links ]
2. Borkovic SP, Schwartz RA. Kaposi's sarcoma. Am Fam Physician. 1982;26(4):133-7. [ Links ]
3. Boshoff C, Weiss R. AIDS-related malignancies. Nat Rev Cancer. 2002;2:373-82. [ Links ]
4. Centers for Disease Control Task Force on Kaposi's sarcoma and opportunistic infections. Epidemiologic aspects of the current outbreak of Kaposi's sarcoma and opportunistic infections. N Engl J Med. 1982;306:248-52. [ Links ]
5. Chor PJ, Santa Cruz DJ. Kaposi's sarcoma: a clinicpathologic review and differential diagnosis. J Cutan Pathol. 1992;19:6-20. [ Links ]
6. Darling M, Thompson I, Meer M. Oral Kaposi's sarcoma in renal transplant patient: case report and literature review. J Can Dent Assoc. 2004;70(9):617-20. [ Links ]
7. Davies JNP, Lothe R. Kaposi's sarcoma in African children. Acta Un Int Cancer. 1962;18:394-9. [ Links ]
8. Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. N Engl J Med. 2003;348:1681-91. [ Links ]
9. Fatahzadeh M. Kaposi sarcoma: review and medical management update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:2-16. [ Links ]
10. Ficarra G, Berson AM, Silverman Jr S, Quivey JM, Lozada-Nur F, Sooy DD et al. Kaposi's sarcoma of the oral cavity: a study of 134 patients with a review of the pathogenesis, epidemiology, clinical aspects and treatment. Oral Surg Oral Med Oral Pathol. 1988;66:543-50. [ Links ]
11. Friedman-Kien AE. Disseminated Kaposi's sarcoma syndrome in young homosexual men. J Am Acad Dermatol. 1981;5:468. [ Links ]
12. Gönen M, Cenker A, Kiyici H, Kalkan M. Penile Kaposi's sarcomas in a circumcised and HIV-seronegative patient. Int J Urol. 2006;13:318-20. [ Links ]
13. Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007; 370(9581):59-67. [ Links ]
14. Guarda LG, Silva EG, Ordóñez NG, Smith Jr JL. Factor VIII in Kaposi's sarcoma. Am J Clin Pathol. 1981;76:197-200. [ Links ]
15. Hammock L, Reisenauer A, Wang W, Cohen C, Birdsong G, Folpe AL. Latency-associated nuclear antigen expression and human herpesvirus-8 polymerase chain reaction in the evaluation of Kaposi sarcoma and other vascular tumors in HIV-positive patients. Mod Pathol. 2005;18:463-8. [ Links ]
16. Hass JR, Hasselager T. Kaposi's sarcoma interpreted as haematoma. Ugeskr Laeger. 2010;172:2388-9. [ Links ]
17. Horenstein MG, Moontasri NJ, Cesarman E. The pathobiology of Kaposi's sarcoma: advances since the onset of the AIDS epidemic. J Cutan Pathol. 2008;35(Suppl 2):40-4. [ Links ]
18. Kang T, Ye FC, Gao SJ, Wang LD. Angiogenesis, Kaposi's sarcoma and Kaposi's sarcoma-associated herpesvirus. Virol Sin. 2008;23:449-58. [ Links ]
19. Lager I, Altini M, Coleman H, Ali H. Oral Kaposi's sarcoma: a clinicopathologic study from South Africa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(6):701-10. [ Links ]
20. Lebbé C. Human herpesvirus 8 as the infectious cause of Kaposi sarcoma: evidence and involvement of cofactors. Dermatol. 1998;134(6):736-8. [ Links ]
21. Lundgren JD. Kaposi's sarcoma and its management in AIDS patients: recommendations from a Scandinavian group. Scand J Infect Dis. 1997;29:3-12. [ Links ]
22. Martin JN. Kaposi sarcoma – associated herpesvirus/ human herpesvirus 8 and Kaposi Sarcoma. Adv Dent Res. 2011;23(1):76-8.
23. Mehta S, Garg A, Gupta LK, Mittal A, Khare AK, Kuldeep CM. Kaposi's sarcoma as a presenting manifestation of HIV. Indian J Sex Transm Dis. 2011;32:108-10. [ Links ]
24. Micali G, Nasca MR, De Pasquale R, Innocenzi D. Primary classic Kaposi's sarcoma of the penis: report of a case and review. J Eur Acad Dermatol Venereol. 2003;17:320-3. [ Links ]
25. Mohanna S, Bravo F, Ferrufino JC, Sanchez J, Gotuzzo E. Classic Kaposi's sarcoma presenting in the oral cavity of two HIV-negative Quechua patients. Med Oral Patol Oral Cir Bucal. 2007;12:E365-8. [ Links ]
26. Musacchio JG, Carvalho Mda G, Morais JC, Silva NH, Scheliga A, Romano S et al. Detection of free circulating Epstein-Barr virus DNA in plasma of patients with Hodgkin's disease. São Paulo Med J. 2006;124:154-7. [ Links ]
27. Ozbudak IH, Guney K, Mutlu D, Gelen T, Ozbilim G. Bilateral tonsillar and esophageal Kaposi sarcoma in an HIV-negative patient. Ear Nose Throat J. 2011;90(7):E23-6. [ Links ]
28. Patrikidou A, Vahtsevanos K, Charalambidou M, Valeri RM, Xirou P, Antoniades K. Non-AIDS Kaposi's sarcoma in the head and neck area. Head Neck. 2009;31:260-8. [ Links ]
29. Pellet C, Chevret S, Blum L, Gauvillé C, Hurault M, Blanchard G et al. Virologic and immunologic parameters that predict clinical response of AIDS-associated Kaposi's sarcoma to highly active antiretroviral therapy. J Invest Dermatol. 2001;117(4):858-63. [ Links ]
30. Quin D, Lu C. The biology of Kaposi's sarcoma-associated herpes virus and the infection of human immunodeficiency virus. Virol Sin. 2008;23:473-85. [ Links ]
31. Schwartz RA, Cohen JB, Watson RA, Gascón P, Ahkami RN, Ruszczak Z et al. Penile Kaposi's sarcoma preceded by chronic penile lymphoedema. Br J Dermatol. 2000;142:153-6. [ Links ]
32. Silverberg MJ, Chao C, Leyden WA, Xu L, Horberg MA, Klein D et al. HIV infection, immunodeficiency, viral replication, and the risk of cancer. Cancer Epidemiol Biomarkers Prev. 2011;20(12):2551-9. [ Links ]
33. Soufiane M, Fadl TM, Nawfel M, Ouafae M, Kawtar Z, Afaf L et al. Kaposi's sarcoma: HIV-negative man with isolated penile localization. Indian J Pathol Microbiol. 2010;53:535-6. [ Links ]
34. Tugizov SM, Webster-Cyriaque JY, Syrianen S, Chattopadyay A, Sroussi H, Zhang L et al. Mechanisms of viral infections associated with HIV: workshop 2B. Adv Dent Res. 2011;23(1):130-6. [ Links ]
35. Vaishnani JB, Bosamiya SS, Momin AM. Kaposi's sarcoma: a presenting sign of HIV. Indian J Dermatol Venereol Leprol. 2010;76(2):215. [ Links ]
36. Wang X, Wang X, Liang D, Lan K, Guo W, Ren G. Classic Kaposi's sarcoma in Han Chinese and useful tools for differential diagnosis. Oral Oncol. 2010;46(9):654-6. [ Links ]
37. Wilkinson J, Cope A, Gill J, Bourboulia D, Hayes P, Imami N et al. Identification of Kaposi's sarcoma-associated herpesvirus (KSHV)-specific cytotoxic T-lymphocyte epitopes and evaluation of reconstitution of KSHV-specific responses in human immunodeficiency virus type 1-Infected patients receiving highly active antiretroviral therapy. J Virol. 2002;76(6):2634-40. [ Links ]
 Corresponding author:
Corresponding author:
Antonio Adilson Soares de Lima
Curso de Odontologia, Departamento de Estomatologia, Universidade Federal do Paraná
Rua Prefeito Lothário Meissner, n. 632 – Jardim Botânico
CEP 80170-210 – Curitiba – PR – Brasil
E-mail: aas.lima@ufpr.br
Received for publication: April 23, 2012
Accepted for publication: July 23, 2012













