Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.10 no.2 Joinville Abr./Jun. 2013
ORIGINAL RESEARCH ARTICLE
Aesthetic improvements in free gingival graft due to its association with frenectomy
Tertuliano Ricardo LopesI; Cassiana Nathalie MachadoI; Mariana Camargo RogacheskiI; Thalyta VerbicaroI; Allan Fernando GiovaniniI; Tatiana Miranda DeliberadorI
I Department of Dentistry, Positivo University – Curitiba – PR – Brazil.
ABSTRACT
Introduction: The insufficient amount of attached gingiva and the abnormal insertion of the labial frenulum may be related. When this occurs, it is common to associate frenectomy techniques with free gingival graft (FGG).
Objective: To evaluate the clinical and histological staining difference and blood flow when the FGG is or is not associated with frenectomy.
Material and methods: Ten patients were selected in the Dentistry Clinics of the Positivo University and divided into two groups (n = 5): group GF (graft/frenectomy), with association of FGG and frenectomy in the V sextant, and group G (graft), in which only the FGG was performed in the V sextant. Clinical examination, initial standardized photographs and post-surgery following-up for seven, 14 and 21 days were executed. For histological analysis the excesses of the graft tissues of a patient from each group were removed.
Results: Clinically, it was observed in both groups after seven and 14 post-operative days, superficial necrosis of the tissue and color similar to the surrounding soft tissue. At 21 days, there is the total reduction of the necrosed tissue, and it was not seen the color difference between groups. Histologically, the difference between groups is related to the epithelial tissue, which was thicker in group G.
Conclusion: Clinical (color) and histological (vascularization) significant differences were not observed between groups GF and G.
Keywords: Periodontics; labial frenulum; gingiva; histology; clinical stage.
Introduction
In the past, the “ideal” amount of attached gingiva was considered by many experts, an important factor for periodontal health11,17,18,24,27,30. According to Lindhe et al.22, after conducting many researches, it was proven that the periodontal health is not related to the amount of attached gingiva, but the plaque is the main etiological factor of periodontal disease and the insertion loss is not dependent on the extent of attached gingiva. The keratinized gingiva has the function of support between the alveolar mucosa and free gingival margin as well as being resistant to traumatic procedures such as toothbrushing34 and orthodontic forces13. There may be a relationship between the highest insertion of the labial frenulum and insufficient attached gingiva7,25. If such a relationship occurs, it may result in gingival recession, because it makes the process of cleaning difficult, leading to the retention of biofilm and culminating in a chronic inflammatory process36.
In cases of abnormal insertion of the labial frenulum that cause deleterious effects such as gingival recession, the frenectomy is indicated29. This technique involves surgical excision of the labial frenulum. The frenectomy technique may be associated with the surgical procedure of free gingival graft (FGG), with the purpose of alleviating the relapse of labial frenulum, in addition to increase the width of attached gingiva3,9,16 and to deepen the vestibule6.
However there are disadvantages to associate the two techniques. One is the necessity of a surgical field to obtain the graft (donor site)3. Moreover, the use of FGG generates an unfavorable aesthetics. This is because the donor site of the graft, in most cases, is the palate (keratinized gingiva) and at the time of transplantation, the receptor site receives the genetic features of the palate22, leaving the grafted area with a whitish shade. According to Carranza et al.12, at the moment of the removal and transplantation of the graft, its color changes to a grayish white ischemic color, because the blood vessels of the graft are empty, i.e., without adequate vascularization.
The aim of this study was to evaluate clinically and histologically, the difference in color and blood supply of FGG with or without frenectomy.
Material and methods
This study was approved by the Ethical Committee in Research of the Positivo University (Curitiba, Brazil), under protocol number 26/12.
For this present study, ten patients were selected from the Dentistry Clinics of the Positivo University, divided into two groups: group GF (five patients requiring FGG and frenectomy in the V sextant) and group G (five patients requiring only FGG in the V sextant).
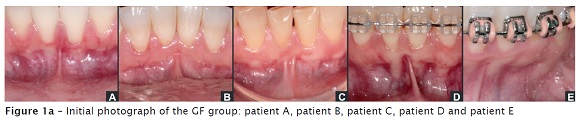
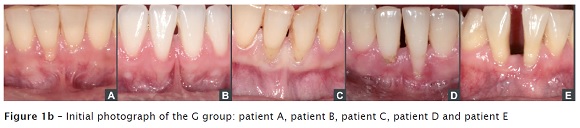
The patients were submitted to clinical examination and initial standardized photographs (figure 1a and figure 1b).
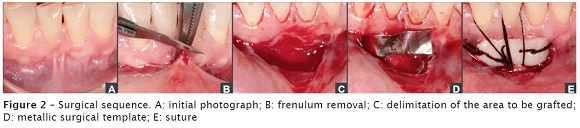
In the group GF, the association of the two techniques were performed comprising frenectomy procedures, preparation of the receptor site, obtainment of the donor site (palate) and FGG technique (figure 2). In group G only the receptor site preparation, the obtainment of the donor site (palate) e and FGG technique were executed.
During the surgical procedure, the patient was submitted to bilateral mental nerve anesthesia and at the donor site an infiltrative anesthesia was performed. The labial frenulum was removed through the frenectomy technique by using the single clamping. With a curve hemostatic clamp and a n. 15c scalpel blade, an incision was executed along the upper surface of the hemostatic clamp surpassing the tip of the clamp a (figure 2-B). Following, a similar incision along the lower surface of the hemostatic clamp consequently result in the labial frenulum removal. Next, a transversal incision in the periosteum (periosteum fenestration), at the height of the alveolar mucosa was executed to avoid a future reinsertion of the frenulum.
Then, the preparation of the receptor site was performed and with the aid of a n. 15c scalpel blade, the deepening of the vestibule was carried out and it was limited to the area to be grafted (figure 2-C). A sterile metallic surgical template (figure 2-D) was used to delimit the area to be graft (map). Previously to the removal of the palate graft, a compressive suture at the posterior area of the palate was executed to compress the greater palatine artery to avoid possible bleeding. Next, the map was placed onto the area between the premolars and an incision perpendicular to the palate was executed, approximately of 1 mm thick, delimiting the graft size. Posteriorly, an incision parallel to the palate was performed to remove the FGG. The graft was adapted to the receptor site through two simple sutures: one at the mesial and the other at the distal side, followed by a compressive “V” suture (figure 2-E).
The area was compressed with moist gauze for 5 minutes to eliminate possible clots between the receptor site and the graft. The sutures were removed after seven days.
In group G, the surgical sequence was the same of the group GF, but without the frenectomy.
To control the post-operative pain and infection, the following drugs were prescribed: anti-inflammatory (Nimesulide – 100 mg, every 12 hours, for 5 days), antibiotics (Amoxicillin – 875 mg, every 12 hours, for 7 days or Clindamycin – 300mg, every 8 hours, for 7 days) and oral antiseptics solution (0.12% chlorhexidine digluconate , every 12 hours, for 7 days)28.
Some post-operative recommendations were instructed to the patients: ice bandages on the receptor site at the first 2 post-surgical hours; not to expose to sun; not execute physical efforts; not vigorously rising; cold liquid and pasty food at the first 48 post-surgical hours.
The patients submitted to the procedures were clinically followed up with periodical appointments at seven, 14 and 21 days. At these periods, standardized photographs were performed aiming to compare the clinical healing between groups. At 21 post-operative days, in two patients (one of the group GF and the other of the group G) it was observed that the FGG was with a thickness wider than that desired. Thus, a second surgical procedure was carried out 84 days after the first surgery, in which a gingivoplasty was executed aiming to reduce the graft thickness.
As a graft piece was removed in the gingivectomy procedure, this tissue was used to evaluate the histological differences in the healing (mainly the vascularization) between both groups. To conduct the histological analysis, the tissue removed was fixed in 10% formaldehyde, washed in water and included in paraffin. Serial cuts of 3 μm of thickness was performed which were stained in hematoxylin and eosin for analysis in light microscopy.
Results
Clinical findings
The results were obtained through clinical and photographic analysis, by observing the color acquired by the graft after the surgery.
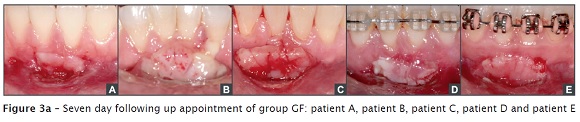
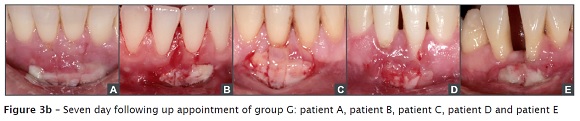
After seven post-operative days, in most patients of both groups, it was seen a superficial necrosis of the tissues. The graft color was similar to that of the surrounding soft tissue (figure 3a and figure 3b).
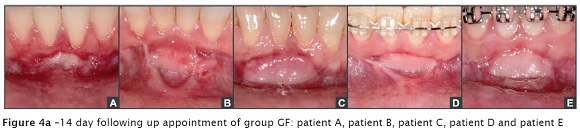
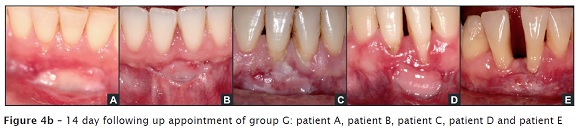
At 14 post-operative day, in some patients of both groups, it was observed yet, small areas of tissue necrosis (figure 4a and figure 4b). The colors of most of the grafts were similar among each other and with the surrounding soft tissue. However, in some patients of both groups, it was seen a more whitish shade than the surrounding tissue (figure 4a – patient A and E and figure 4b – patient A and D).
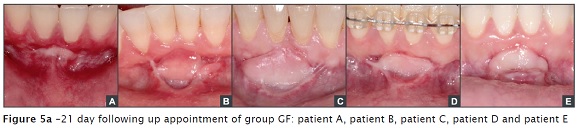
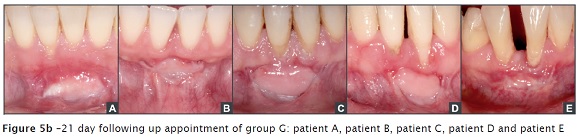
At 21 post-operative days, it was verified the total regression of the necrosis in both groups and it was not observed clinical differences of the color between groups (figure 5a and figure 5b). In group GF, two patients exhibited the graft color very closer to that of the surrounding tissue (figure 5a – patients B and C). In group G, three patients showed the graft color very closer to that of the surrounding tissue (figure 5b – patients B, C and E).
Histological findings
The aim of the histological analysis was to compare the difference in vascularization (amount of the blood vessels) between the groups GF and G.
In the histological cuts of the group G, it was seen a dense and fibrous connective tissue, covered by an epithelium, verifying intense pseudoepitheliomatous hyperplasia and high keratinization. Area of a discrete chronic inflammatory infiltrate in the connective tissue of the focal area was observed (figure 6b). In the histological cuts of the group GF, it was noted a dense and fibrous connective tissue, in addition to a thinner epithelial tissue (figure 6a).
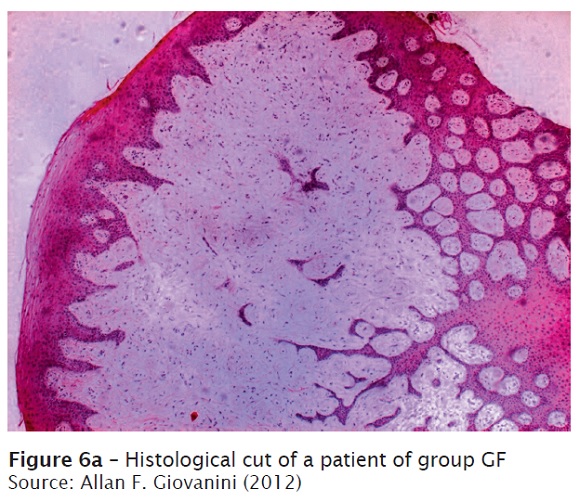
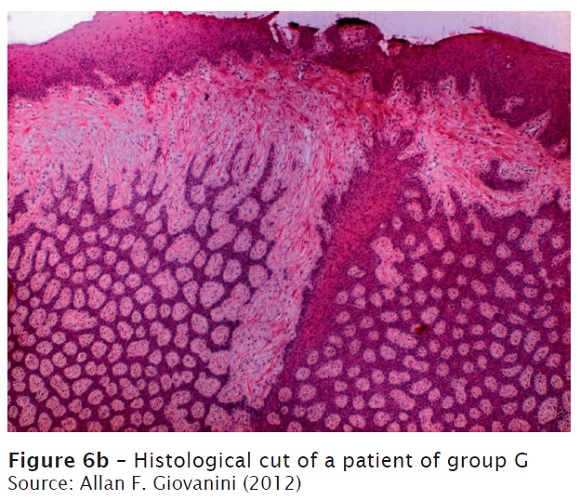
It was not observed a vascular difference between the groups. The main distinction between the groups was the amount of the epithelial tissue, which was greater in group G.
Discussion
The labial frenulum, when abnormally inserted may cause damage to the periodontium4,5,10. Such damaging effects comprising from area hygiene difficulty because of the bad positioning of the toothbrush to gingival recession caused by the traction of the mucosa2,8,14,15,20,21,23,32.
One of the treatments recommended by these cases is the frenectomy (total removal of the labial frenulum)1. However, the healing of this surgical procedure results in an area of little keratinized gingiva. Thus, it is common to associate the frenectomy procedure with the FGG, which maintain the frenulum insertion far from the gingival margin, in addition to lead to an increasing of the attached gingiva19.
FGG surgical procedure consists in the removal of the gingival tissue from the palate (donator site) and its transference for the area with lack of keratinized tissue (receptor site)19. The advantages of this type of procedure are related to the increasing of the area and tissue thickness, graft predictability, technique simplicity and post-operative no painful symptomatology of the receptor site. There are some disadvantages, such as unfavorable aesthetics, second intention healing of the palate, in addition to more painful post-operative period and risks for complications33. Because FGG has the disadvantage of lack of aesthetics at the post-operative period, this present study hypothesized if the possibility of its association with the frenectomy procedure would show a healing improvement, due to a greater vascularization of the area (coming from the frenectomy) and consequently better aesthetics in relation to the color of the graft. However, this hypothesis was not confirmed after the observation of the clinical and histological results. For a longer longevity of the graft, it is necessary that it has proper dimensions, that is, it must be sufficient thin to enable its nutrition (through propagation of the fluids) through the receptor site. A very thinner graft has great chances of necrosis and exposure of the receptor area26,31. However, if the graft is very thicker, its superficial layer may be at risk, once the excess of tissue will hinder an adequate nutrition35. In this present study, a gingivoplasty was necessary in two patients because the gingival grafts were thicker than the desired thickness However, the histological result did not demonstrate an inadequate nutrition, regardless of the thickness of the grafts.
The healing of the FGG comprises three phases: 1) initial phase, from 0 to three days. At this stage, the epithelium of the grafted tissue undergoes a superficial necrosis and receives its avascular plasmatic nutrition from the receptor site22, because just after its removal from the donator site, the blood vessels of the graft are empty12; 2) revascularization phase, from two to 11 days. There is the union (anastomosis) of the pre-existing vessels and the appearance of new vessels, in addition to the beginning of the new re-epithelization; 3) maturation phase, from 11 to 42 days. The “maturation” of both the vessels and epithelium occurs with keratin deposition22.
In this present study, the gingival tissue of both groups was gathered for histological analysis 84 days after the initial surgical procedure. Therefore, it could be observed the tissue healing and the maturation phase. The groups exhibited a similar maturation and amount of blood vessels. Additionally, in the histological aspect, it was verified that the connective tissue repair in both groups was similar. Either fibrosis or disturbances of the vascular new formation was not detected. In group G, it was noted a greater focal epithelial hyperplasia (frenulum area), which was not a primordial factor for the color changing in the representative part of the surgical site. In the tissue remnant, the amount of epithelium is normal. One hypothesis for this focal hyperplasia can be related to the frenulum which was not removed in this group, whose epithelium is superimposed to that of the grafted tissue. Notwithstanding, clinically, this variation is not visible.
Conclusion
Within the limits of this study, it can be concluded that in both groups, there was not clinical (color) and histological (vascularization) significant differences between the association or not of the frenectomy and FGG techniques.
References
1. Addy M, Dummer PM, Hunter ML, Kingdon A, Shaw WC. A study of the association of fraenal attachment, lip coverage and vestibular depth with plaque and gingivitis. J Periodontol. 1987 Nov;58(11):752-7. [ Links ]
2. Almeida AL, Madeira LC, Freitas KC, Greghi SL, Pegoraro LF. Cross-sectional evaluation of the presence of gingival recession in individuals with cleft lip and palate. J Periodontol. 2007 Jan;78(1):29-36. [ Links ]
3. Axinn S, Brasher WJ. Frenectomy plus free graft. J Prosthet Dent. 1983 Jul;50(1):16-9. [ Links ]
4. Baum AT. The midline diastema. J Oral Med. 1966 Jan;21(1):30-9. [ Links ]
5. Bergese F. Ricerche sull inserzione dei frenuli labiali in bambini fra i 9 e 12 ani. Minerva Stomatol. 1966 Oct;15(10):672-6. [ Links ]
6. Bjorn H. Fri transplantation av gingival propria [abstract]. Tidn. 1963;55:84. [ Links ]
7. Bowers GM. A study of the width of attached gingival. J Periodontol. 1963 May;34(1):201-9. [ Links ]
8. Bracho RP, Vicuña NH, Elejalde L, Ceballos OZ, Gudiño MP, Torrealba JCl. Recesión gingival de incisivos inferiores en adolescentes, su asociación con factores de riesgo. Acta Odontol Venez. 2003 Aug;41(3):31-4. [ Links ]
9. Breault LG, Fowler EB, Moore A, Murray DJ. The free gingival graft combined with the frenectomy: a clinical review. Gen Dent. 1999 Sep-Oct;47(5):514-8. [ Links ]
10. Bressman E. The importance of the frenum pull in periodontal disease. In: Ward HL (Ed.). A periodontal point of view. Springfield: Charles C. Thomas; 1973. [ Links ]
11. Carranza FA, Carraro JJJJ. Mucogingival techniques in periodontal surgery. J Periodontol. 1970;41:294-9. [ Links ]
12. Carranza FA, Newman MG, Takei HH, Klokkevold PR. Periodontia clínica. 10. ed. Rio de Janeiro: Elsevier; 2007. p. 1008-12. [ Links ]
13. Coatoam GW, Behrents RG, Bissada NF. The width keratinized gingiva during orthodontic treatment: its significance and impact on periodontal status. J Periodontol. 1981 Jun;52(6):307-13. [ Links ]
14. Duarte CA, Castro MVM, Duarte LPCM. Frênulo labial e papila gengival: soluções cirúrgicas. In: Duarte AC, Castro MVM. Cirurgia estética periodontal. 1. ed. São Paulo: Santos; 2004. p. 97-113. [ Links ]
15. Fowler EB, Breault LG. Early creeping attachment after frenectomy: a case report. Gen Dent. 2000 Sep-Oct;48(5):591-3. [ Links ]
16. Freedman AL, Stein MD, Scheneider DB. A modified maxillary labial frenectomy. Quintessence Int Dent Dig. 1982 Jun;13(6):675-8. [ Links ]
17. Friedman N, Levine HL. Mucogingival surgery: current status. J Periodontol. 1964;35:5-21. [ Links ]
18. Hall WB. The current status of mucogingival problems and their therapy. J Periodontol. 1981;52:569-75. [ Links ]
19. Kina JR, Luvizuto ER, Macedo APA, Kina M. Frenectomia com enxerto gengival livre: caso clínico. Rev Odontol Araçatuba. 2005;26(1):61-4. [ Links ]
20. Kivovics P, Jáhn M, Borbély J, Márton K. Frequency and location of traumatic ulcerations following placement of complete dentures. Int J Prosthodont. 2007 Jul-Aug;20(4):397-401. [ Links ]
21. Lascala NT, Lascala Junior NT. Aspectos cirúrgicos na prevenção – frenectomia – bridectomia e ullectomia. In: Lascala NT. Prevenção na clínica odontológica. 1. ed. São Paulo: Artes Médicas; 1997. p. 210-20.
22. Lindhe J, Karring T, Lang NP. Tratado de periodontia clínica e implantologia oral. 4. ed. Rio de Janeiro: Guanabara Koogan; 2005. p. 560-72. [ Links ]
23. Massad JJJJ, Anderson JF. Hamular frenum modification: a removable denture prosthesis retention and stability enhancement. Int J Periodontics Restorative Dent. 2001 Apr;21(2):183-9. [ Links ]
24. Matter J. Free gingival grafts for the treatment of gingival recession. A review of some techniques. J Clin Periodontol. 1982;9:103-14. [ Links ]
25. Mccomb JL. Orthodontic treatment and isolated gingival recession: a review. Br J Orthod. 1994 May;21(2):151-9. [ Links ]
26. Mormann W, Schaer F, Firestone AC. The relationship between success of free gingival grafts and transplant thickness. J Periodontol. 1981 Feb;52(2):74-80. [ Links ]
27. Nabers CL. Repositioning the attached gingiva. J Periodontol. 1954;25:38-9. [ Links ]
28. Nassar CA, Bitencour AP, Nassar PO. Evaluation of chlorhexidine effects on periodontium healing after gingivoplasty surgery. RSBO. 2012;9(1):56-61. [ Links ]
29. Nogueira GRF, Benatti BB, Bittencourt S, Peruzzo DC, Casati MZ. Frenectomia associada ao enxerto gengival livre. Rev Gaúcha de Odontol. 2005 Apr-Jun;53(2):85-164. [ Links ]
30. Ochsenbein C. Newer concept of mucogingival surgery. J Periodontol. 1960;31:175-85. [ Links ]
31. Pennel BM, Tabor JC, King KO, Towner JD, Fritz BD, Higgason JD. Free masticatory mucosa graft. J Periodontol. 1969 Mar;40(3):162-6. [ Links ]
32. Raveli DB, Chiavini PCR, Pinto AS, Sakima MT, Martins LP, Melo ACM. Diastema interincisal. Fatores etiológicos: relato de casos clínicos. J Bras Ortodon Ortop Facial. 1998 Nov-Dec;3(18):36-42. [ Links ]
33. Segundo TK, Alves R. Emprego do enxerto gengival epitélio-conjuntivo no recobrimento radicular. Rev Gaúcha Odontol. 2005 Jan-Mar;54(1):81-3. [ Links ]
34. Stoner JE, Mazdyasna S. Gingival recession in the lower incisor region of 15 year old subjects. J Periodontol. 1980 Feb;51(2):74-6. [ Links ]
35. Ward VJ. A clinical assessment of the use of the free gingival graft for correcting localized recession associated with frenal pull. J Periodontol. 1974 Feb;45(2):78-83. [ Links ]
36. Yared KFG, Zenobio EG, Pacheco W. A etiologia multifatorial da recessão periodontal. R Dental Press Ortodon Ortop Facial. 2006 Nov-Dec;11(6):45-51. [ Links ]
 Corresponding author:
Corresponding author:
Tatiana Miranda Deliberador
Mestrado Profissional em Odontologia Clínica, Universidade Positivo
Rua Professor Pedro Viriato Parigot de Souza, n. 5.300 – Campo Comprido
CEP 81280-330 – Curitiba – PR – Brasil
E-mail: tdeliberador@gmail.com
Received for publication: November 11, 2012
Accepted for publication: December 1, 2012













