Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.3 Joinville Jul./Set. 2016
LITERATURE REVIEW ARTICLE
Regenerative endodontic treatment of teeth with incomplete root formation: a review
Lincon Hideo NomuraI; Rodrigo Otavio Jatahy Ferreira do AmaralI; Carla Frehner AndradeI; Nathaly Dias MoraisI; Flares Baratto-FilhoI; Denise Piotto LeonardiI
I Department of Dentistry, Positivo University – Curitiba – PR – Brazil
ABSTRACT
Introduction: Endodontic treatment of teeth with open apex requires a non-conventional approach and the goals new therapies are to allow root's complete development differently from what happens with traditional apexification technique. Objective: This study aimed to review the literature on the most recent regenerative endodontic procedures.Literature review: Regenerative endodontics goal is to obtain pulp vitality. Some case reports on donor-obtained dental stem cells show promising results. Other types of laboratory-based dental stem cell therapies are under development. Conclusion: Dentin-pulp complex shows regenerative capacity, but the literature lacks evidence to validate the regenerative therapies in endodontic practice.
Keywords: regeneration; endodontics; dental pulp.
Introduction
The association of bioengineering and medicine results in the appearance of a new study field namely tissue engineering. Tissue engineering goal is to restore some of lost tissue function through natural or synthetic reconstruction in laboratory. New frontiers in Dentistry also have been gained, namely Regenerative Dentistry 12.
Although some current treatment approaches offer high success rate in Endodontics, pulp regeneration may be an alternative to replace necrosed by healthy pulp tissue aiming at tooth revitalization12. Many procedures comprise regenerative endodontics, from direct pulp capping, revascularization, apexogenesis, apexification, to stem-cells and tissue engineering 8.
The traditional cleaning, shaping, and filling of immature teeth with open apex are not indicated. Moreover, due to the thin dentinal walls, these teeth are susceptible to fracture after endodontic treatment 21. Traditionally, apexification through multiple appointments and longer intervals of calcium hydroxide dressing, is used to create an apical barrier prior to canal filling 12. Because this procedure alters the dentin properties and make the teeth susceptible to fracture 3, an approach comprising one or two appointments for placing an apical barrier with mineral trioxide aggregate (MTA) prior to the filling of the coronal portion has been advocated 3. This procedure was reported with high success rates in the literature. However, this procedure does not result in the continuity of the root formation and does not reduce the chance of fracture 12. The ideal result expected for these situations would be a pulp regeneration capable of promoting the normal root development of the tooth 12.
The pulp revascularization is a regenerative treatment and an alternative biological-based method to treat immature teeth, and differently from the apexification and MTA apical barrier, it enables the continuity of the root development 20.
Case reports in the literature show convincingly that immature permanent teeth with pulp necrosis and apical periodontitis and/or abscess may undergo apexogenesis, revascularization or regeneration. However, the literature lacks a guideline on the treatment of these case 5.
This study aimed to review the current literature on pulp regeneration for immature teeth with periapical lesion.
Literature review
Regenerative medicine
The regenerative medicine is the combination of cells, material engineering, and biochemical factors to improve or replace the biological functions attempting to promote the medicine advancement. The basis of regenerative medicine is the use of tissue regenerative therapies 14.
Langer and Vacanti 13 proposed a tissue engineering as a possible technic for regenerating the lost tissues. They affirm that tissue engineering is "an interdisciplinary field that applies the engineering and medical science principles target to the development of biological substitutes to restore, maintain, or improve the tissue function" 13.
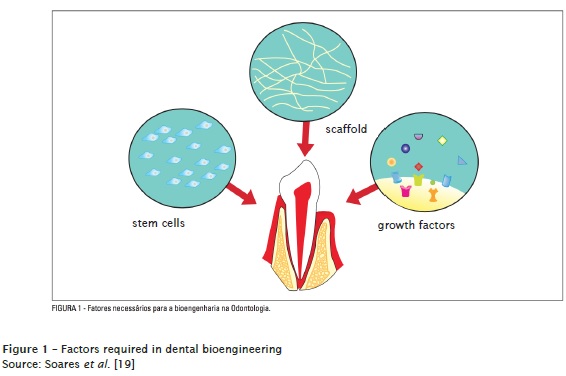
To develop tissue engineering or regenerative medicine, three components are necessary: cells capable of forming tissue (stem cells), physical scaffold that enables the cell differentiation and growth, and molecules (growth factors) that signalizing the cell growth, proliferation, and differentiation 10 (figure 1).
Stem cells
Stem cell biology is an important study field to understand tissue regeneration and the implementation of regenerative medicine 11.
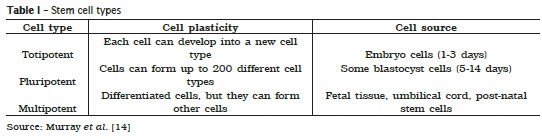
The stem cells are commonly subdivided into totipotent, pluripotent, and multipotent according to their plasticity 14 (table I).
However, the research with embryo stem cell is controversial with legal and ethical problems, a fact that decrease the researchers' attention to develop new therapies with these cells. This explain why many studies are raising attention towards post-natal/adult stem cells donated by the patients themselves or their closer relatives14.
Since the discovery and characterization and multipotent mesenchymal stem cells (MSCs) from bone marrow (BM), MSC population from other tissues have been discovered based on the "golden-standard" criterion established for the bone marrow mesenchymal stem cells (BMMSCs) 9. The fat and blood tissue from the umbilical cord have been a promising alternative for MSCs 9.
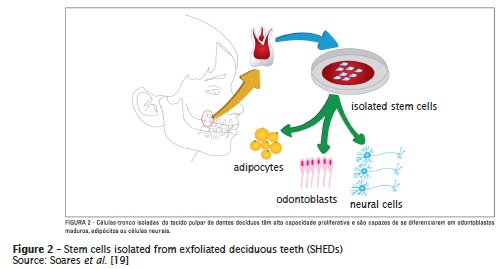
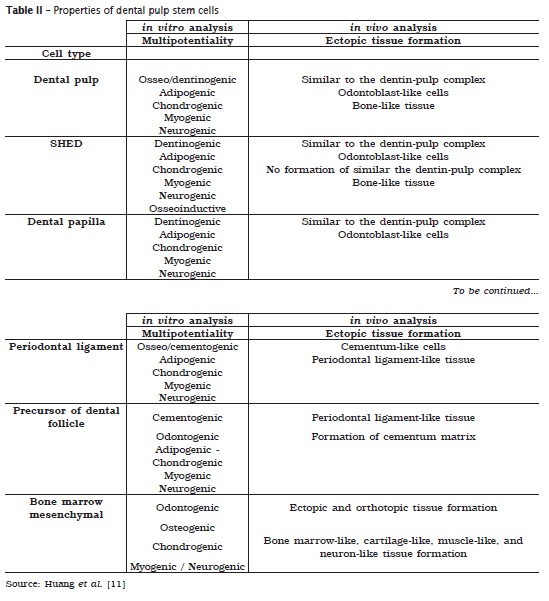
The search for MSCs in specific tissues account for the discovery of many stem cells in many tissues and organs in the last decades 11. MSCs from dental tissue are among them 11 (figure 2, table II). The first type of dental stem cell was gathered from the human pulp tissue namely post-natal dental pulp stem cell (DPSC) 9. Subsequently, more than three dental MSCs were isolated and characterized: Stem cells from exfoliated deciduous teeth (SHEDs), periodontal ligament stem cells (PDLSCs), and stem cells from dental papilla (SCAP). The most recent studies identified a stem cell population from dental tissue, namely dental follicle precursor cells (DFPCs) 11. However, the exact relationship among these different cell population is uncertain 11.
Scaffold
The scaffolds provide the physical, chemical, and biological tridimensional microenvironment for cell differentiation and growth, promoting cell migration and adhesion 4. The scaffolds should be effective to transport the nutrients, oxygen, and residues. They should be gradually degraded and replaced by the regenerated tissue, maintaining the characteristic of the tissue structure 15.
In the field of regenerative endodontics, Plateletrich plasm (PRP) has been suggested potentially as the ideal scaffold. PRP is autologous and relatively easy to prepare in dental clinics 21. In cases of revascularization, the blood clot has been used as scaffold and source of stem cells 22.
Growth factors
Growth factors are proteins secreted as extracellular signs that ruled the morphogenesis/ organogenesis during the epithelium-mesenchymal interactions 4, link to cell receptors, and induce cell proliferation and/or differentiation. Many growth factors are versatile, stimulating cell division into countless cell types, while other are more specific. The name of growth factors commonly has little to do with the main functions, but has to do with the circumstances they appear. For example, fibroblast growth (FGF) was found in the brain extract of a cow and tested in a research that cause the proliferation of fibroblast. Currently, many growth factors were identified with specific functions that may be used to control stem cell activity, either by increasing the cell proliferation rate, inducing the cell differentiation by other tissue type, or stimulating the stem cell to synthetize the mineralized matrix 14.
The dentin contains many proteins capable of producing the tissue stimulus. The dentin demineralization may release growth factors 14.
Other important family of growth factors for tooth developing and regeneration is bone morphogenetic proteins (BMPs). BMP2 stimulates the differentiation of adult pulp stem cells in a cell culture of odontoblastoid morphology. BMP-2, -4, and -7 proteins induce the in vivo formation of reparative dentin. The insulin growth factor (IGF- 1) together with collagen induce the complement of dentinal linkage and formation of tubular dentin. This indicates the regenerative potential of adding growth factors prior to pulp capping or of incorporating these factors to endodontic and restorative materials to stimulate dentin and pulp regeneration 14.
Regenerative Dentistry
Abou Neel et al.1 showed the scenario of the studies on dental tissue engineering. Many dentistry areas, as periodontium, implantodontics, endodontics, and surgery – with researches on salivary glands, skin, oral mucosa, fascial muscles, bone, and temporomandibular joint. The studies demonstrated that in periodontics, the tissue engineering showed great advancements in the last 10-15 years regarding the development of materials for biodegradable scaffolds that behave as templates for the periodontium regeneration 1.
Dental implants are practical and reliable elements for the lost tooth. Notwithstanding, the main side effect of dental implants is the lack of natural contour and structural relationship with alveolar bone, that is, lack of periodontal ligament 11. Huang et al. 11 affirmed that tissue regeneration is a reality in dental practice, because it was possible to reach promising results in forming a new periodontium on an artificial root, with characteristics resembling the original one, but with inferior physical properties. They still showed the beneficial effects of growth factors such as platelet derived growth factor (PDGF) and insulin growth factor (IGF); scaffolds such as platelet-rich plasma (PRP); and cell therapies (bone marrow mesenchymal stem cells) on the repair of periodontal defects 11.
Abou Neel et al.1pointed out that a real potential exists in reaching the dreamed engineering of a complete tooth, biologically. The further studies on regenerative dentistry are targeted to a change from metal-based (implants) to biological-based (cells) dentistry 1.
Regenerative endodontics (pulp regeneration)
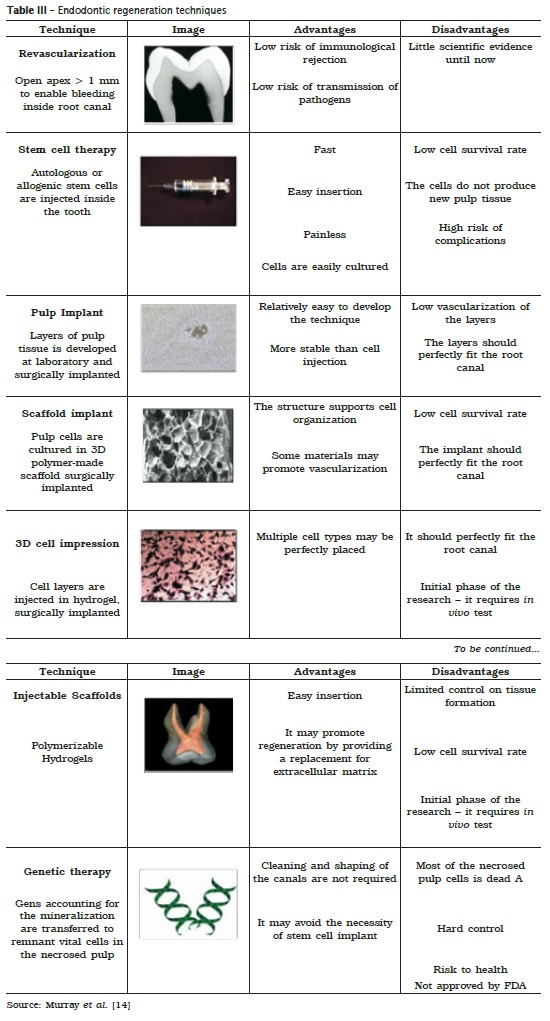
The endodontics is still benefited from this study field of tissue regeneration. Many research areas may be applied on the development of endodontic regenerative techniques 14: a) revascularization through blood clot, b) adult stem cell therapy, c) pulp implant, d) scaffold implant, e) injectable scaffold, f) tridimensional cell impression, and g) genetic therapy 14. These are the most advanced techniques in Endodontics, currently. Notwithstanding, these techniques require further studies to validation because their practical clinical application is still not feasible. table III show the advantages and disadvantages of each aforementioned techniques.
Apexogenesis
Apexogenesis is defined as the physiologic root development not restricted to the apical segment. The continuous dentin deposition occurs along with the root length promoting the increasing of the rigidity and resistance to fracture.
Always when pulp exposure occurs in an immature tooth, one should select a technique that preserves pulp vitality the most. This step enables the continuous physiological dentin deposition, enabling the complete root development 24.
Apexification
When a tooth with incomplete root formation undergoes pulp necrosis, dentin formation and root development stops 7. Consequently, the root canal is large, with thin and fragile walls, with open apex. Thus, endodontic treatment is hindered because root canal preparation is difficult and apical stop is inadequate 7. In those cases, to allow proper apical filling and sealing is indispensable to create the artificial apical barrier to induce the closure of the apical foramen with the mineralized tissue 7.
Trope 23 described the apexification as the formation of a mineralized tissue barrier through calcium hydroxide use. For that purpose, a favorable environment is necessary, similar to the apexogenesis cases 23. This environment should be free of bacteria and provide a mild inflammatory stimulus to initiate the repair 23. Calcium hydroxide is deposited over the apical tissues with instrument or absorbent points. The canal remnants are filled with calcium hydroxide all over the extension, and periodical changes are scheduled at every 6 to 18 months. At every three months, a radiograph is taken to evaluate the formation of mineralized tissue formation. When one suspects of barrier formation, calcium hydroxide is removed through sodium hypochlorite irrigation and another radiograph is taken to evaluate the apical barrier radiopacity. An endodontic file is gently placed up to the apex to verify the apical stop 23.
The apexification with calcium hydroxide is a traditional technique extensively studied over the years with high success rate. However, apexification with calcium hydroxide has some disadvantages, such as treatment time. Treatment time may be as longer as 6 to 18 months, at 3-month interval, to evaluate the formation of hard tissue barrier. This requires the patient's compliance with up to six appointments. Also, the literature evidences that longer use of calcium hydroxide weaken the dentin resistance to fracture 3. Thus, cases of new dental traumas or root fractures are common even prior to the ending of apexification.
Apical barrier through mineral trioxide aggregate (MTA)
MTA is used to create a hard tissue barrier after root canal disinfection. A bulkhead (e.g.: calcium sulfate) is placed beyond the apex to allow a resorbable extra-radicular barrier and that MTA is placed of the apical third, at 3 to 4 mm. A cotton pellet is placed over MTA for at least 6 hours; then, the canal is filled. The immediate filling of the canal is also possible because the tissue fluids of the open apex provide enough conditions for MTA setting. The most cervical portion of the root canal is reinforced by resin composite up to the level of the alveolar ridge 23.
In a study conduct on dogs, Felippe et al. 7 evaluated the MTA influence on apexification and periapical repair in teeth with incomplete root formation and contaminated canals and verified whether calcium hydroxide was necessary prior to MTA. They concluded that MTA favored apexification and periapical repair even without the prior dressing with calcium hydroxide paste. When calcium hydroxide was previously placed, MTA overflowed and barrier formation over the limits of root walls 7.
Studies proved the clinical success of MTA apexification 7,18,23. Notwithstanding, the thin root dentin walls of the incomplete tooth is still a clinical problem. New traumas may occur and these teeth are more prone to non-restorable fractures. The literature reported that at least 30% of these fractures will occur during or after endodontic treatment. Some clinicians still questioned the predictability of the apexification technique and have opted by more invasive treatments, such as tooth extraction followed by implant 23.
The most recent pulp regeneration techniques are based on the following goals: 1) enable the development of the apical portion of the root; 2 maintain the dentin thickness along the root.
Revascularization
Revascularization is the disinfection of the necrosed root system followed by the establishment of bleeding through over instrumentation of the canal and coronal sealing.
The pulp tissue of immature teeth with open apex has a very rich blood supply and contain a structure more prone to regeneration in response to aggressions compared to a completely formed tooth 5.
According to Torabinejad and Turman 21, there is a growing evidence that the pulp revascularization of a human immature tooth with open apex is possible after pulp necrosis and apical pathology. Clinical case and case series reports have demonstrated radiographic signs of continuous formation of dentin walls followed by the apical closure of the roots in teeth with periapical lesions 5,10,16,20,22.
Albuquerque et al. 2 revised the literature on the different protocols of pulp revascularization. The authors reported that the research on this area begins around the 50s and 60s. Since the 2000s, revascularization started to be reported as an alternative to apexification. Attention was drawn to the possibility of the complete development of the root in the cases of necrosed teeth with incomplete root formation. Moreover, recently, the studies focus on the knowledge of which would occur after revascularization: metaplasia or regeneration. Metaplasia is the repair of the root canal space by a tissue similar to the periodontium and bone, while regeneration is the formation of a new pulp tissue that develops with the same characteristics of the damaged tissue 3.
These authors concluded that revascularization is a simple technique with advantages over the apexification because it promotes the dentin wall resistance and apical closure, decreasing the tooth weakness. However, they consider that little is known about the long-term side effects. The authors suggested further longitudinal studies to understand the mechanical properties of dentin wall mineralization 2.
The revascularization follows a well-defined protocol. The disinfection is a fundamental and mandatory step to reach treatment success 6. Differently from conventional endodontics, root canal instrumentation is contraindicated because the root walls are thin and immature. Disinfection is obtained through a proven effective antibiotic therapy against the microorganisms present in endodontic contamination, that is, ciprofloxacin, metronidazole, and minocycline 17. Minocycline has been associated to dentin staining and is frequently replaced by cefaclor 20.
Garcia-Godoy and Murray 8 suggested the following guidelines for tooth regeneration:
1) The tooth should undergo necrosis without indication for apexogenesis, apexification, partial pulpotomy, or endodontic treatment;
2) The tooth should be permanent, immature, and with open apex. The tooth should have thin root walls that benefit from the continuous root development to become stronger and less susceptible to future fracture;
3) The patient should age between 7 and 16 years, have good health. The parents or legal responsible should be aware that the treatment demand multiple appointments;
4) The parents or legal responsible should be aware that pulp regeneration is an experimental treatment and standardized protocols are not available;
5) The patient should be aware about tooth staining due to the use of the antibiotic paste;
6) A anesthetics without vasoconstrictor should be used to induce bleeding inside root canal;
7) MTA or calcium hydroxide layer should be dressed above the blood clot;
8) The endodontic sealers are not biocompatible with regeneration and should not be used;
9) The tooth should be restored with resin-modified glass ionomer, resin composite overlay, or full crown to prevent microleakage, depending on the degree of crown structure loss.
The following regenerative therapies 14 are at experimental level, still further form clinical practice, but the research is increasingly in advance.
Post-natal stem cell therapy
Because of the restrictive politics around mesenchymal stem cells, the researchers have drawn attention to post-natal stem cells donated by the patients themselves or by their closer relatives. This method consists of placing post-natal stem cells inside root canals for regenerative purpose.
The disadvantage is the low survival of the injected stem cells and migration of the stem cells for different body parts, possibly leading to damaging mineralization. Other problem is the isolation of these stems cells for regenerative endodontics 14.
Pulp implant
This technique comprises the transplantation of pulp tissue to a cleaned and shaped root canal. This pulp tissue is originated from purified pulp stem cells free of pathogens or cells obtained from biopsy and cultured in the laboratory 14. Pulp stem cells should be organized into a tridimensional structure capable of maintaining a cell organization and vascularization. This can be reached through the culture of pulp cells on biodegradable membranes or extracellular matrices, such as collagen and fibronectin 14.
The advantage of this technique is the easy laboratorial culture of these cells, much more stable in matrices when compared with cell injection into empty root canals. The disadvantage is the need of specialized procedures to assure the proper adherence to root canal walls l 14.
Scaffold implant
A porous polymer scaffold can be plated with pulp stem cells and implanted into an empty root canal aiming at creating tridimensional pulp tissue with cell organization and vascularization similar to that of native pulp. This scaffold should contain growth factors to help in cell proliferation and differentiation, nutrients to promote cell survival and growth, antibiotics to fight against any microorganism inside the canal. The scaffold should exert mechanical and biological functions essential to the replanted tissue and should be biodegradable to avoid the need of surgical removal. It is still not fully understood which scaffold type would be suitable for providing the best substrate to achieve a high survival rate of the stem cells – collagen, polymer, or calcium phosphate 14.
Application of injectable scaffold
In this technique, the pulp tissue is constructed by tissue engineering on a tridimensional scaffold of colloidal gel. These so-called hydrogels are injectable through syringe. The most recent study attempt to obtain light-cured hydrogels and rigid structures after the application in the targeted tissue 14.
3D cell impression
A device similar to tint jet is used to apply cell layers suspended into hydrogel to recreate pulp tissue structure. The technique could be used to place precisely many cells and has the potential to create a tissue very similar to the natural pulp tissue. The disadvantage is the highest complexity to guide the pulp tissue all over root canal extension, that is, from coronal to apical third 14.
Gene therapy
This method consists of placing genes accounting for pulp tissue mineralization towards the root canal site. A vector is employed to introduce the therapeutic gene on the patient's targeted cells. The vector is injected though intravenous route or injected directly in the tissue where the targeted cells are. Another alternative would be to remove the targeted cells, expose them to the vector at the laboratory, and reintroduce them into the patient 14.
Genetically modified virus to maintain human DNA are vectors commonly used 14.
There are serious risks to health in genetic therapy. Accordingly, this regenerative procedure is not very promising 14.
Conclusion
Dentin-pulp complex has the potential to regenerate even in permanent teeth undergoing pulp necrosis and immature apex. However, further studies with higher scientific evidence level are necessary to confirm the findings.
References
1. Abou Neel EA, Chrzanowski W, Salih VM, Kim HW, Knowles JC. Tissue engineering in dentistry. J Dent. 2014;42(8):915-28. [ Links ]
2. Albuquerque MTP, Nagata JY, Soares AJ, Zaia AA. Pulp revascularization: an alternative treatment to the apexification of immature teeth. Rev Gaúch Odontol. 2014;62(4):401-10.
3. Andreasen JO, Farik B, Munksgaard EC. Longterm calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18(3):134-7.
4. Bansal R, Jain A, Mittal S, Kumar T, Kaur D. Regenerative endodontics: a road less travelled. J Clin Diagn Res. 2014;8(10):ZE20-4.
5. Chueh LH, Ho YC, Kuo TC, Lai WH, Chen YH, Chiang CP. Regenerative endodontic treatment for necrotic immature permanent teeth. J Endod. 2009;35(2):160-4.
6. Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod. 2009;35(5):745-9.
7. Felippe WT, Felippe MC, Rocha MJ. The effect of mineral trioxide aggregate on the apexification and periapical healing of teeth with incomplete root formation. Int Endod J. 2006;39(1):2-9.
8. Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol. 2012;28(1):33-41.
9. Gronthos S, Zannettino AC, Hay SJ, Shi S, Graves SE, Kortesidis A, Simmons PJ. Molecular and cellular characterisation of highly purified stromal stem cells derived from human bone marrow. J Cell Sci. 2003; 116(9):1827-35.
10. Hargreaves KM, Geisler T, Henry M, Wang Y. Regeneration potential of the young permanent tooth: what does the future hold? J Endod. 2008;34(7S): S51-6.
11. Huang GT, Gronthos S, Shi S. Mesenchymal stem cells derived from dental tissues vs. those from other sources: their biology and role in regenerative medicine. J Dent Res. 2009;88(9):792-806.
12. Kundabala M, Abhishek P, Neeta S. Regenerative endodontics: a review. Malays Dent J. 2010;31(2):94-100.
13. Langer R, Vacanti JP. Tissue engineering. Science. 1993;260(5110):920-6.
14. Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod. 2007;33(4):377-90.
15. Nakashima M, Akamine A. The application of tissue engineering to regeneration of pulp and dentin in endodontics. J Endod. 2005;31(10):711-8.
16. Nosrat A, Seifi A, Asgary S. Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: a review and report of two cases with a new biomaterial. J Endod. 2011; 37(4):562-7.
17. Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E. Sterilization of infected root-canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J. 1996;29(2):118-24.
18. Simon S, Rilliard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one-visit apexification treatment: a prospective study. Int Endod J. 2007;40(3):186-97.
19. Soares AP, Knop LAH, Jesus AA, Araújo TM. Células-tronco em odontologia. R Dental Pres Ortodon Ortop Facial. 2007;12(1):33-40.
20. Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatr Dent. 2007;29(1):47-50.
21. Torabinejad M, Turman M. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod. 2011;37(2):265-8.
22. Trope M. Regenerative potential of dental pulp. J Endod. 2008;34(7S):S13-7.
23. Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010;54(2):313-24.
24. Weisleder R, Benitez CR. Maturogenesis: is it a new concept? J Endod. 2003;29(11):776-8.
 Corresponding author:
Corresponding author:
Lincon Hideo Nomura
Rua Joaquim Carneiro, n. 135, sala 01
Capoeiras
CEP 88085-120
Florianópolis – SC – Brasil
E-mail: linconn@gmail.com
Received for publication: March 14, 2016
Accepted for publication: June 13, 2016













