Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.13 no.3 Joinville Jul./Set. 2016
LITERATURE REVIEW ARTICLE
Clinical strategies for managing emergency endodontic pain
Simone Scandiuzzi FranciscoI; Cláudia Leal Sampaio SuzukiI; Ana Paula da Silva LimaI; Marina Coelho Rodrigues MacielI; Rodrigo Dutra MurrerI
I Course of Dentistry, Leão Sampaio School – Juazeiro do Norte – CE – Brazil
ABSTRACT
Introduction: Pulpal and periradicular pain is leading cause of emergency care demand. Literature review: Pain management in endodontics includes important aspects for its control and prevention, such as reducing anxiety and preoperative pain, control of intra-operative pain and the treatment of postoperative pain. These review pointed out some important measures that may be the key for the effectiveness control and prevention of pain in endodontic procedures. One of the effective strategies currently used in these cases is structured to evaluate the painful condition through a 3-D approach which establish a differential diagnosis, definitive treatment, and rational use of drugs, based on the most appropriate scientific evidence available in the literature.
Keywords: pain; flare up; postoperative pain; pain control.
Introduction
The orofacial pain can be one of the worst human experiences, many times unbearable, leading the individual to experience physical and mental illness, so that orofacial pain is considered as a serious public health problem in many countries 20. Tooth pain is the main complaint of individuals who search for emergency dental care and involves many situations, such as: tooth-bone fractures, tooth fracture with pulp exposure, acute tooth pain (pulpitis), apical abscesses, dilaceration in oral mucosa, and hemorrhages 1,6,9,20.
The pain origin can be classified into odontogenic and non-odontogenic. Notwithstanding, most of the pain symptoms is related to the alterations in the pulp and periapical tissue, and endodontic treatment is generally indicated 24. Dourado et al. 5 verified that the pulp and periapical pathologies most prevalent in emergency care were pulp necrosis (69.3%), irreversible acute pulpitis (25%), reversible acute pulpitis (4.1%), acute apical periodontitis (30.4%), and acute apical (17.8%). Francisco et al. 9 conducted a study with 1,481 patients of emergency care, of whom 927 reported pain of pulp origin, with the most frequent diagnosis of irreversible pulpitis (563 cases), followed by pulp necrosis (173 cases), and reversible pulpitis (191 cases).
The emergency cases resulting from orofacial pain require immediate attention of the dentist, and the clinician must be apt to identify the evolution, analyze the clinical features, and establish the differential diagnosis and treatment planning capable of relieving the patient's pain 20.
In Endodontics, the management of pre- and post-operative pain should include important aspects for its controlling and prevention, such as anxiety reduction and control of pre/transoperative pain through local anesthetic techniques and pharmacological drugs 19. The effective strategy for managing the endodontic pain is based in the pain assessment through a 3-D approach that consists of establishing the differential diagnosis, definitive treatment, and rational use of drugs 13. This literature review aimed to identify and systematize the clinical approaches for pain control during endodontic emergency care through the accurate diagnosis and clinical and pharmacological intervention.
Literature review
Differential diagnostic – the first D
The diagnosis should be the starting point for pain control, because the pain cause may involve anatomic and psycho factors 19,37. The first D consists of establishing the differential diagnosis based on identifying oral pathologies and their origins through step-guided investigation, obtaining objective and subjective information on the problem. The pain can be defined as an unpleasant sensorial and emotional experience associated to a real or potential tissue damage. Acute pain is defined as a recent damage of limited duration; chronic pain is related to persistent duration 19.
The dentist should understand the differences between the pain site and the origin site. If the pain and origin sites are the same, this is socalled primary pain. If the pain and origin sites are different, this is so-called referred pain, e.g.: the heart pain after heart ischemia is frequently perceived on the left arm, shoulder, or mandible. The pain origin is the heart muscle, but the pain site is very far from the origin site. Some nonodontogenic pathologies cause referred pain on head and neck area and on sound teeth. The clinician should be able to recognize these different situations 19.
In Endodontics, the differential diagnosis requires a unique combination of knowledge and ability to understand and interact with the patient. The initial challenge is to comprehend the biological process behind the pain and identify which subjective and objective signs are necessary to establish an effective diagnosis and treatment to relieve the pain. The clinical examination is guided through a systemized step-by-step to obtain the diagnosis, as follows: 1) to establish the main complaint; 2) to perform the anamnesis; 3) to perform extra- and intraoral examination, observing the presence of alterations; and 4) to determine the need of adjunct tests 22,25.
The previous medical history is important to evaluate the general health condition of the patient. The medical anamnesis is necessary prior to any treatment, because medical emergency care may occur at the beginning of the treatment 21,39. The previous tooth history leads to a probable pathology associated to the pain history, initial symptoms and clinical evolution. The dentist can guide the process of subjective information by asking some questions, such as: When did the pain start? Is the pain constant? Which is the pain intensity? Is it a spontaneous pain or only after a stimulus? Does the pain become worst after laying down? Is it an intermittent pain? Is it a localized and diffuse pain? 11.
The (extra- and intraoral) physical examination provides objective information to observe extraoral signs as symmetry and swelling; and intraoral signs as swelling rushing, itching, and fistula. It is also relevant to identify intraorally the presence of carious lesions, their extension, defective restorations, and exposed dentin. The radiographic evaluation provides useful information on the involved structures; however, the radiograph is an adjunctive examination complementary to the clinical examination 19. The adjunctive tests op pulp diagnosis, especially the cold test, will determine the pulp sensitivity. The pulp condition is classified into normal, reversible pulpitis, irreversible pulpitis, or necrosis. Other essential semiotic resources for identifying the pain etiology are the palpation and percussion test. which indicated the inflammation of the periradicular tissues, resulting from inflammation in the fibers of the periodontal ligament or pulp necrosis 13.
All the periapical and pulp tests (radiographs, cold or heat test, palpation and percussion test, fistula tracking, transillumination, and biopsy) enable to collect information to obtain the probable diagnosis, planning, and evaluation of the pathology 11,36.
Definitive treatment – the second D
The second D is the definitive dental treatment or the emergency dental care required for pain remission. The diagnosis accuracy leads to the safe and correct treatment, using adequate procedures that allows significant pain reduction and the correct drug association that contributes to pain control and relief 13.
By confirming the diagnosis and the pain origin, the treatment for relieving the signs and symptoms is established. For example, if the patient reports a history of intense pulsatile, spontaneous pain, for many days, the probable diagnosis would be irreversible pulpitis; if the patient refers pain on a tooth recently restored, the probable diagnosis would be tooth sensitivity to thermal variation and a less invasive approach is recommended 11,22. The procedures of emergency endodontic care comprise: pulpotomy, pulpectomy, foramen/ bone cortical trepanation, incision, drainage, and occlusal reduction13.
Dental caries consequences mainly account for emergency dental care, resulting in pulp and apical pathologies. The retrospective studies on emergency care highlighted that irreversible pulpitis is the most common diagnosis, followed by pulp necrosis, and the molars are the most affected teeth 1,9.
The symptomatic irreversible pulpitis exhibits intermittent or spontaneous pain, and the fast temperature changes, especially cold, will result in episodes of longer and intense pain even after the removal of the stimulus. As the inflammatory responses increase, the intrapulpal pressure also increases, the venous return decreases, and the vascular damage shows the symptoms of spontaneous and pulsatile pain, which increases at decubitus, consequently resulting in pulp necrosis; this latter tends to show pain relief with cold and pain increasing with heat 11,22,35.
Pulp inflammations may cause unbearable pain, and emergency care is required through the complete removal of the inflamed pulp (pulpectomy), especially if pain after percussion is present 11,22. Notwithstanding, because the patient who search for emergency care is not scheduled, the operative time is very reduced to perform pulpectomy. Thus, pulpotomy is an acceptable treatment to cease the pain, aiming at removing the affected coronal pulp tissue without touching the root canals 16,29,33. The high success rate of pulpotomy is associated to the alteration in pulp hemodynamics and pressure of the interstitial fluid because the pain relief occurs due to the decompression of the enlarged pulp tissues due to the inflammatory process 16.
Partial pulpectomy can be accomplished mainly in multi-rooted teeth by completely removing the pulp tissue of the larger straighter canals (palatal canal of maxillary molars and distal canal of the mandibular molars). Because of the complex morphology of the buccal roots of the maxillary molars and mesial roots of the mandibular molars, it is not advisable to prepare these canals, due to difficult in proper cleaning during emergency care, resulting in hemorrhage and increase in inflammation and patient's discomfort. In cases presenting pain at percussion, it is recommended to establish the working length, instrument all canals up to file #25, and perform occlusal adjustment 11.
According to Agnihorry et al. 2, the irreversible pulpitis is characterized as one of the main causes motivating the patients to seek emergency care. The most indicated approach is endodontic treatment associated to analgesic or anti-inflammatory drugs. However, a significant number of dentists still prescribes antibiotics to relief the pain during irreversible pulpitis. According these authors, the literature reports little evidence that antibiotics reduce the pain. The authors still recommended that the antibiotics prescription does not replace pulpectomy in these cases 2.
According to Ruddle 35, many endodontic diagnoses are not properly executed during the routine appointments and observed that many pulp and periapical pathologies develop without pain episodes, so that the dentist accounts for the pulp and periapical clinical assessment during routine appointments 35. Michaelson and Holland24 analyzed clinically and radiographically 2,202 maxillary anterior teeth and approximately 40% had periapical lesion without history of spontaneous or thermal-stimulated prolonged pain, quietly progressing to necrosis.
When pulp necrosis occurs, the blood supply and the pulp microcirculation are damage and, before the pathologic condition progress towards the periodontium, the tooth normally is asymptomatic and do not respond to electrical or thermal tests. Notwithstanding, after pulp necrosis and development of intra-radicular infection, an inflammatory reaction in the periapex may occur, whose evolution will depend on the number and virulence of the microorganisms, intensity of the host's response, and time period 38.
The complete instrumentation is the ideal treatment for symptomatic teeth, mainly when the periodontal ligament is injured, indicating the presence of acute apical periodontitis. Thus, at the emergency appointment, all necrotic tissue must be removed. In single-rooted teeth, complete pulpectomy is easily performed, while multi-rooted teeth demand a more complicated preparation due to anatomical variations. Notwithstanding, the preparation length is at 2-3 mm below the radiographic apex for all canals 11.
By knowing that bacteria are directly involved in the etiology and perpetuation of the pulp alterations, an exacerbated inflammatory reaction may develop from the necrosis within the root canal, causing inflammatory edema and leading to periodontal ligament detachment, that clinically may appear as the characteristic signs of "grown tooth". The tooth extrusion sensation, moderate to severe spontaneous pain, and sensitivity to percussion are the features of apical periodontitis, which depending on the extension of the inflammatory response may evolve to acute dentoalveolar abscess 11. A tooth with acute dentoalveolar abscess is extremely sensible to mastication, percussion, and palpation, but does not respond to any pulp test and has many mobility degrees. At the radiographic examination, the periodontal ligament space may be enlarged and shows periradicular radiolucency. At the vestibule bottom and adjacent soft tissues, swelling may occur that complicates the treatment and demands the following-up of the remission of these signs and symptoms after emergency care. The presence of fever, swelling, prostration, cervical and submandibular lymphatic nodes sensible to palpation (lymphadenitis) evidences that the infectious process is not properly controlled by the normal defense mechanisms ant requires antibiotic therapy 23.
The treatment of the acute intraosseous alveolar abscess is not different from that of the necrosed pulp, in which there is the presence of unbearable pain and lack of extra or intraoral edema. In these cases, the exudation is confined to the apical area and the drainage is obtained through the total instrumentation of the canal with the foramen trepanation attempting to drain the pus through the canal 37. The intraoral presence of the pus localized at the vestibule bottom (fluctuating, nonfluctuating, localized or diffuse), requires surgical drainage due to the pus in the subperiosteal/ submucosal area. The emergency care in patients with swelling aims at achieving the pus drainage and 24-48 after to decontaminate the root canal 3.
In the cases that the aforementioned procedures failed to relieve the pain, the cortical trepanation is indicated. This procedure consists in the surgical trepanation of the alveolar cortical to release the tissue exudate and to relieve the pain of patients with severe and persistent periradicular pain 32,33. Notwithstanding, many studies evaluate the effectiveness of cortical trepanation in symptomatic teeth with pulp necrosis and moderate to severe pain 27,28. Some authors reported the pain relief 7,31, but others reported a post-operative increasing of the pain 32,33.
The literature is also controversial about the need of occlusal reduction after the endodontic procedure 15,34. According to Rosenberg et al.34, the occlusal reduction performed in cases with pre-operative pain, sensitivity to percussion, or biopulpectomy is a simple approach to prevent post-operative pain 34.
The endodontic therapy may lead to pain during and after treatment (post-operative pain), which makes the patient seeks emergency care. Flare-up or post-operative pain is the emergency care between endodontic appointments of root canal preparation. It is characterized by pain, swelling, or both 18,37. Many articles report the prevalence of post-operative pain, ranging from 1.4% to 16%, as well as flare-up causes, such as the use of different intracanal medications, irrigant solution, instrumentation techniques, and number of appointments 5,18,29,37.
According to Siqueira and Barnett 37, the factors causing pain during endodontic procedures are of chemical or mechanical origin and commonly associated to iatrogeny, microbial factors present in pulp and periradicular pulp, and presence of periapical lesion induced or aggravated during root canal treatment 37. The microorganisms may cause pain in between appointments due to the following situations: apical extrusion of debris, incomplete instrumentation leading to alterations in the endodontic microbiota, and secondary intraradicular infections 29.
The occurrence of mild post-operative pain is not rare, even with the endodontic treatment followed acceptable standards. The mild pain after chemical-mechanical preparation may occur in approximately 10-30% of the cases, and in most cases, the discomfort is decreased with common analgesic drugs to relieve the symptoms 5. The development of moderate to severe post-operative pain, with or without swelling, on the other hand, ins uncommon and demands emergency care 37.
Systemic drugs – pain control
The third D stands for the drugs used to control the pain and infection. The endodontic treatment and emergency care may cause pain expectation in the patients and increase the symptoms when associated with levels of anxiety and fear. The presence of the pre-operative pain also causes many difficulties in the management of the patients 26. Thus, the dentist has two strategies to modulate the pain: pain prevention and treatment3. It is important to control the preoperative anxiety because emergency care situation may cause stress during dental treatment 21.
The treatment of orofacial pain requires a comprehensive interpretation of the patient's feelings and experiences, comprising all aspects of the treatment: pre-operative, trans-operative, and post-operative 25. The control of the preoperative pain comprises the correct diagnosis of the pathology, proper anesthetic technique, and anxiety reduction through techniques and drugs; at the trans-operative period, the pain control is performed with an effective technique of local anesthesia, proper operative techniques, and systemic medication; at post-operative period, the pain management involve many drugs 19.
Despite of the advancements in modern pharmacology, the pain causes anxiety and fear, which makes pain control more difficult 19,26. It is important to emphasize that the pain perception in patients with high levels of anxiety may cause the reduction of the tolerance to pain, so that the pharmacological strategies are available to reduce the patient's anxiety, e.g.: anxiolytics taken 45 minutes before the dental procedure 3.
According to Nusstein et al. 30, 81-83% of the patients who sought emergency care with moderate to severe pain took until nine days to seek treatment and most of them had taken medication to relieve the symptoms 30. Other non-pharmacological approaches have been used to control fear, anxiety and stress, such as the behavioral techniques (modeling, conditioning, and hypnosis) 19.
The treatment should not be performed without the effective pain control through effective local anesthesia during the endodontic treatment. Thus, the dentists should be updated with the many anesthetic techniques, their advantages and limitations, and administration routs 14. According to Hargreaves and Keiser 14, the operator's inability to place the anesthetic solution in the target nerve may lead to improper blockage of sound and inflamed teeth. Patients with preexisting symptoms may not tolerate any pain stimulus, so the conventional anesthetic techniques may not be effective to obtain deep pulp anesthesia 14.
Other aspect to be taking into consideration, it is the tissue inflammation, because local anesthetics are less effective due to the more acid pH 14. Rosenberg 33 affirmed that pre-operative pain and anxiety are predictors for local anesthesia of patients with clinically normal teeth 33,39.
Clinical studies demonstrated that a single local anesthetic injection for alveolar inferior nerve blocking is ineffective in 30-80% of patients with diagnosis of irreversible pulpitis. The patients with irreversible pulpitis may have eight times more failure in anesthetic technique compared with normal patients 4,30,39,40.
Other anesthetic techniques are used for controlling endodontic pain such as intraosseous, intraligamentary, and intrapulpar 4,37,39. According to Fan et al. 8, the alveolar inferior nerve blocking may be associated with the anesthesia of the buccal nerve or intraligamentary anesthesia to increase the anesthesia success in cases of irreversible pulpitis 8. The intraosseous injection (II) enables placing the local anesthetic solution directly on the cancellous bone adjacent to the tooth to be anesthetized21. Currently, a system is available on dental market so-called Stabident. Stabident is composed by a slow-speed perforator (micro motor) coupled with burs to create a small orifice on the cortical plate. The anesthetic solution is placed on the cancellous bone through a 27-gauge needle, placed on the orifice previously made by the perforator, a very effective technique if the conventional techniques failed 30. The intrapulpar infiltrative anesthesia is an extreme resource in teeth with deep caries and pulp exposure. The anesthetic solution is directly injected on dental pulp, and the liquid injection should be fast because the injection pain is instantaneous. Regardless from the technique chosen, the dentist should have the ability to execute and know the morphology of the surrounding structures 14.
It is estimated that about 20% of the patients experience moderate to severe pain after endodontic treatment 13. Even if the treatment would be tooth extraction, systemic action drugs are necessary, e.g.: analgesic, anti-inflammatory, and antibiotics 3,13.
The use of drugs to control the pain should be planned rationally and strictly to situations requiring pharmacological management, adjunctive to the dental treatment 12,14. The dentist is allowed to prescribe any drug with proven indication in Dentistry, including those with controlled use. Such approach demands that the dentist knows the prescribed drug, including the side effects, possible interactions, indications, and contraindications 3,12.
Among many analgesic drugs available at the market, those used in Dentistry are dipyrone and paracetamol. Although the acetylsalicylic acid (AAS®, Aspirin®) would be an option, the amount of side effects limit its use, especially in surgical procedures because aspirin alters the bleeding time through inhibiting platelet aggregation. In the cases of post-mild operative pain, analgesic drugs are recommended; while in cases of severe and persistent pain, the treatment will depend on the diagnosis o 3.
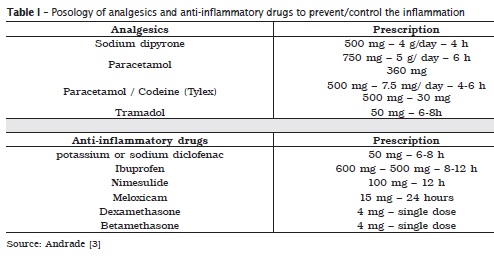
The anti-inflammatory drugs comprise two groups: non-steroidal and steroidal (corticoids). Nonsteroidal anti-inflammatory (NSAIs) are effective against dental pain 23. The dentist's experience on the expectancy of exacerbated inflammatory response will indicate the prophylactic use of anti-inflammatory drugs prior to the procedure. Moreover, in acute inflammatory processes already installed (pulpitis, pericementitis, abscesses) the use of drugs can rapidly control the pain, clinically 3,12,17. The clinician can also use the corticosteroids indicated with safe in Dentistry: dexamethasone and betamethasone 3,12. Both drugs have the same power, and can be use at single dose of 4 mg. table I shows the usual posology of analgesics and NSAIs to prevent/control dental inflammation.
The presence of systemic alterations indicates that the infectious process is not controlled by the host's defense mechanism, and antibiotics are required. According to Fouad 10, the use of antibiotics is not indicated for controlling the post-operative pain 2,10. The best criterion to decide on the use of antibiotics is related to the presence or absence of signs of dissemination and systemic manifestations of the infection, that is, when the patient shows indicative signs that the immunological defenses by themselves cannot control the infection. These signs are marked swelling (cellulitis), mandibular trismus, lymphadenitis, fever, tachycardia, appetite loss, general malaise 3,23.
The indiscriminate and incorrect use of antibiotics may lead to the appearance of multiresistant bacteria that are not sensible to any antibiotics available in the market and whose control can be complex. This problem may directly affect Dentistry because the effectiveness of the most used antibiotics may decrease. According to Andrade3, many dentists still considered erroneously The antibiotics should be considered as adjunctive treatment in controlling the infections.
Conclusion
The emergency care because of orofacial pain requires immediate dentist's attention. Accordingly, the dentist should be apt to identify the pain evolution by analyzing the characteristics and causal factors, to establish a differential diagnosis and treatment plan capable of relieving the pain. A systematic approach to understand the pathologic problem consists of establishing the precise diagnosis, effective definitive treatment, and rational use of drugs. This review pointed out some important approaches that may be key factors for the effective pain remission, control, and prevention in endodontic procedures. The pain management requires clinical approach based on scientific evidence whenever possible to choose the best treatment alternative in cases of pain. Thus, the constant updating of the therapeutic approaches is necessary.
References
1. Abbud R, Ferreira LA, Campos AG, Zanin KEG. Atendimento clínico de emergência: um estudo dos serviços oferecidos em dez anos. Rev Assoc Paul Cir Dent. 2002;56(4):271-5. [ Links ]
2. Agnihotry A, Fedorowicz Z, van Zuuren EJ, Farman AG, Al-Langawi JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev. 2016;2:1-26.
3. Andrade ED. Terapêutica medicamentosa em odontologia. São Paulo: Artes Médicas; 2014.
4. Cohen HP, Cha BY, Spangberg LS. Endodontic anesthesia in mandibular molars: a clinical study. J Endod. 1993;19:370-3.
5. Dourado AT, Caldas Jr AF, Albuquerque DS, Sá Rodrigues VM. Estudo epidemiológico de urgências odontológicas. J Bras Clin Odont Int. 2005;9(48):60-4.
6. Ehrmaann EH, Messer HH, Clark RM. Flare-ups in endodontics and their relationship to various medicaments. Aust Endod J. 2007;33:119-30.
7. Elliot JA, Holcomb JB. Evaluation of a minimally traumatic alveolar trephination procedure to avoid pain. J Endodon. 1988;14:405-7.
8. Fan S, Chen WL, Pan CB, Huang ZQ, Xian MQ, Yang ZH et al. Anesthetic efficacy of inferior alveolar nerve block plus buccal infiltration or periodontal ligament injections with articaine in patients with irreversible pulpits in the mandibular first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:89-93.
9. Francisco SF, Fur tado AP, Por to DN, Carvalho DA, Fleury EDM. Levantament o dos atendimentos odontológicos do curso de Odontologia da UniEvangélica. Revista da FOA. 2008;10(8):86-92.
10. Fouad AF. Are antibiotics effective for endodontic pain? Endod Top. 2002;3:52-6.
11. Gutmann JL, Lovdahl PE. Soluçõe s em endodontia – prevenção, identificação e procedimentos. São Paulo: Elsevier; 2012.
12. Hargreaves KM, Abot t PV. Drugs for pain management in dentistry. Aust Dent J. 2005;50(2):14-22.
13. Hargreaves KM, Keiser K. New advances in the management of endodontic pain emergencies. CDA Journal. 2004;32:469-73.
14. Hargreaves MK, Keiser K. Local anesthetic failure in endodontics: mechanisms and management. Endodontic Topics. 2002;1:26-39.
15. Harrington GW, Natkin E. Midtreatment flareups. Dent Clin North Am. 1992;36:409.
16. Hasselgren G, Reit C. Emergency pulpotomy: pain relieving effect with and without the use of sedative dressings. J Endod. 1983;15(6):254-6.
17. Holstein A, Hargreaves KM, Niederman R. Evaluation of NSAIDs for treating post-endodontic pain. A systematic review. Endodontic Topics. 2002;3:3-13.
18. Imura N, Zuolo ML. Factors associated with endodontic flare-ups. A prospective study. Int Endod J. 1995;28:261-5.
19. Keiser K, Hargreaves KM. Building effective strategies for the management of endodontic pain. Endodontic Topics. 2002;3:93-105.
20. Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124(10):115-21.
21. Malamed SF. Emergency medicine: beyond the basics. J Am Dent Assoc. 1997;128:843-54.
22. Marshall J.Planning endodontic treatment. Dental Clinics of North America. 1979;23(4):495-519.
23. Matthews DC, Sutherland S, Basrani B. Emergency management of acute apical abscess in permanent dentition: a systematic review of the literature. J Can Assoc. 2003;69(10):660.
24. Michaelson LP, Holland RG. Is pulpitis painful? J Int Endod. 2002;35:829-32.
25. Montgomery S, Ferguson CD. Endodontics. Diagnostic, treatment planning, and prognostic considerations . DentClinNorthAm. 1986;30(3):533-48.
26. Moore R, Brodsgaard I. Dentists' perceived stress and its relation to perceptions about anxious patients. Community Dent Oral Epidemiol. 2001;29(1):73-8.
27. Moos HL, Bramwell JD, Roahen JO. A comparison of pulpectomy alone versus pulpectomy with trephination for the relief of pain. J Endod. 1996;22:422-5.
28. Nist E, Reader A, Beck M. Effect of apical trephination on postoperative pain and swelling in symptomat ic necrot ic teeth. J Endod. 2001;27:415-20.
29. Nivethithan T, Raj JD. Endodontic pain – cause and management: a review. International Journal of Pharmaceutical Sciences and Reasearch. 2015:6(7):2723-7.
30. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endod. 1998;24:487-91.
31. Peters DD. Evaluation of prophylactic alveolar trephination to avoid pain. J Endod. 1980;6:518-26.
32. Rossman ER, Hasselgren G, Wolcott FJ. Diagnóstico e controle da emergência das dores dentárias orofaciais. In: Cohen S, Hargreaves MK. Caminhos da polpa. 9. ed. Rio de Janeiro: Elsevier; 2007. p.40-55.
33. Rosenberg PA. Cl inical strategies for managing endodontic pain. Endodontic Topics. 2002;3:78-92.
34. Rosenberg PA, Babick P, Schertzer L, Leung A. The effect of occlusal reduction on pain after endodontic instrumentation. J Endod. 1998;24:492-6.
35. Ruddle C. Endodontic diagnosis. Dentistry Today. 2002;21(10):90-101.
36. Sipavičiūtė E, Manelienė R. Pain and flareup after endodontic treatment procedures. Bal t ic Dental and Maxi l lofacial Journal . 2014;16(1):25-30.
37. Siqueira Jr JF, Barnett F. Interappointment pain: mechanisms, diagnosis, and treatment. Endodontic Topics. 2004;7:93-109.
38. Siqueira Jr JF. Microbial causes of endodontic flare-ups. International Endodontic Journal. 2003;36:453-63.
39. Walton R, Torabinejad M. Managing local anesthesia problems in the endodontic patient. J Am Dent Assoc. 1992;123:97-102. 40. Wong M, Jacobsen P. Reasons for local anes the siafailures . J Am Dent Assoc . 1992;12:69-73.
 Corresponding author:
Corresponding author:
Simone Scandiuzzi Francisco
Rua João Francisco Sampaio, s/n
Condomínio Terra dos Kariris, casa 01
CEP 63180-000 – Barbalha – CE – Brasil
E-mail: simonescan@gmail.com
Received for publication: December 23, 2015
Accepted for publication: June 2, 2016













