Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista Brasileira de Odontologia
versão On-line ISSN 1984-3747versão impressa ISSN 0034-7272
Rev. Bras. Odontol. vol.73 no.1 Rio de Janeiro Jan./Mar. 2016
ARTIGO DE REVISÃO/ODONTOLOGIA PARA PACIENTES COM NECESSIDADES
Utilização da toxina botulínica no tratamento do bruxismo em pacientes portadores de paralisia cerebral: revisão de literatura
Use of botulinum toxin for the treatment of bruxism in patients with cerebral palsy: a literature review
Bruna Michalski dos SantosI; Bruna Lavinas Sayed PiccianiII; Geraldo Oliveira Silva-JúniorIII; Thays Teixeira de SouzaIV; Hyllari Curty PinheiroV; Lívia Maria S. IzahiasVI; Luciana Freitas BastosVII; Tatiane MaregaVIII
I Dental Center for Special Patients, Associação Brasileira de Odontologia (ABO-RJ), Rio de Janeiro, Brazil
II Dental Center for Special Patients, ABO-RJ, Rio de Janeiro, Brazil Postgraduate Program in Pathology, School of Medicine, Universidade Federal Fluminense (UFF), Niteroi, Rio de Janeiro, Brazil
III Dental Center for Special Patients, ABO-RJ, Rio de Janeiro, Brazil Department of Diagnostic and Therapeutic, Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, Brazil
IV Postgraduate Program in Pathology, School of Medicine, UFF, Niteroi, Rio de Janeiro, Brazil
V School of Dentistry, UFF, Niteroi, Rio de Janeiro, Brazil
VI School of Dentistry, UFF, Niteroi, Rio de Janeiro, Brazil
VII Department of Preventive Dentistry and Community, UERJ, Rio de Janeiro, Brazil
VIII Special Care Dentistry, Universidade São Leopoldo Mandic, Campinas, São Paulo, Brazil
RESUMO
A paralisia cerebral (PC) é caracterizada por lesão cerebral não progressiva, sendo a causa mais frequente de deficiência física infantil. Os problemas neuromusculares afetam a saúde bucal, sendo o bruxismo um achado frequente. Este é caracterizado pela aplicação de forças excessivas nos músculos mastigatórios, podendo causar disfunção da articulação temporomandibular, dores de cabeça e desgaste dentário. Recentemente a injeção local da toxina botulínica foi relatada como excelente opção terapêutica. O objetivo deste estudo foi realizar revisão de literatura sobre o tratamento do bruxismo com a utilização da toxina botulínica na PC.
Descritores: paralisia cerebral; bruxismo; toxina botulínica.
ABSTRACT
Cerebral palsy (CP) is characterized by nonprogressive brain injury, the most common cause of child disability. Neuromuscular problems affecting oral health, being bruxism a frequent finding. This is characterized by the application of excessive forces in the masticatory muscles, may cause temporomandibular joint dysfunction, headaches and tooth wear. Recently, the local injection of botulinum toxin was reported as excellent therapeutic option. The aim of this study was to conduct a literature review on the treatment of bruxism with the use of botulinum toxin in the PC.
Descriptors: botulinum toxin; bruxism; cerebral palsy.
Introduction
Cerebral palsy (CP) is a general term that includes very different clinical manifestations that have in common motor difficulty due to a brain injury. It is the most frequent cause of physical disability in children. The incidence reported in the literature varies widely, ranging from 2.0 to 2.5 cases per 1,000 live births 1. In addition to motor compromise, required to characterize CP, other variable frequency changes are mental retardation, seizures, language disorders, visual disturbances, behavioral disorders, orthopedic disorders 2, malnutrition conditions, obesity, and hydrocephalus 3,4. CP may occur during the prenatal, perinatal, or postnatal period; may be congenital, genetic, inflammatory, infectious, anoxic, traumatic, or metabolic 1; and may be clinically classified as spastic, athetoid, ataxic, and mixed 5.
Neuromuscular problems due to CP can significantly affect oral health in relation to the change in growth pattern of the jaws 6-9; development of parafunctional habits; problems in chewing, swallowing 10,11, and saliva control; respiratory disorders 12; and difficulties with maintaining oral hygiene 13. The oral conditions frequently encountered are caries, periodontal disease, bruxism 14,15, gingival hyperplasia 15,16, malocclusion, trauma 14,15, change in salivary flow, and oral reflections 14.
Bruxism, which means squeezing and gnashing of teeth, is a prevalent habit in patients with CP 17. It generates masseter hypertrophy, headaches, temporomandibular articulation changes, flare or thickening of the periodontal ligament, and wear facets on the posterior teeth and anterior 18,19. The cause of this involvement is unknown. Some authors have reported factors such as spasticity 17; oral myofunctional disorders 9,20; dysfunction of the vertebral column with the head projected forward, which changes the contact between the teeth and predisposes hyperactivity of the main masticatory muscles (temporal and masseteric) 17; lack of the control of mandibular posture, which can be aggravated during periods of emotional stress 17; sleep disturbances 21; use of neuroleptics 20; and malocclusion 17. In CP carriers, the damage is compounded and irritability may occur, in addition to episodes of bites on the cheeks, lips, and tongue and unilateral or bilateral hypertrophy of the masticatory muscles, particularly the masseter 22, as described by Hanson and Barret 23.
Several types of treatment for bruxism have been investigated, such as occlusal splints, medication, and psychological treatment, but they are ineffective 24,25. Recently, the local injection of botulinum toxin (BTX) has been successfully used to treat various movement disorders 26,27. BTX is a potent biological toxin also called neurotoxin. It is produced by the anaerobic bacterium Clostridium botulinum 28, which has a paralytic effect by inhibiting the release of acetylcholine at the neuromuscular junction 30. BTX is a safe and effective treatment for many forms of neurological disorders 28,29. Botulinum toxin type A (BTX-A) is a toxin scientifically recognized as being the most potent and has a longer-lasting effect. It is extensively used for treating bruxism in patients with disabilities 31. The injection of BTX-A in patients with CP reduces muscle spasticity, lower lip trauma, and bruxism and improves mouth opening and the ability to perform oral hygiene 19.
The goal of this study was to conduct a literature review about the treatment of bruxism with the use of BTX in patients with CP.
Data Collection Method
We reviewed the literature published between 1967 and 2015, comprising theses, dissertations, books, and selected scientific articles, by searching the SciELO, BIREME, MEDLINE, and LILACS databases. The database searches were performed using the keywords "cerebral palsy," "bruxism," "botulinum toxin," and "botulinum toxin A." As a result of these searches, we selected 86 studies published in the English or Portuguese language including literature reviews, case reports and scientific papers, that addressed the topics of interest for this review.
Literature Review
• Cerebral Palsy
Definition, Epidemiology, and Etiology
CP, also called nonprogressive chronic encephalopathy (NPCE) or chronic childhood encephalopathy (CCE), is defined as nonprogressive brain damage that manifests in early childhood, resulting from the injury in the immature central nervous system (CNS), resulting in changes of posture and movement 32,33. Little (1843) first described CCE as a disease with various causes and characterized mainly by muscle rigidity. In 1862, it established the relationship between this clinical picture and its intercurrences with childbirth 34,35. Freud (1897) suggested CP expression, which later was confirmed by Phelps, in a group of children who had severe motor disorders due to CNS injury 34-37. CP is the most common form of chronic motor incapacity that begins in childhood 38. The incidence of NPCE has remained constant in recent years, with a prevalence of 2.5 per 1,000 live births in the developed countries. In developing countries, the incidence is higher, reaching 7 per 1,000 live births. In Brazil, it is estimated that there are 30,000–40,000 new cases each year 1.
The etiology of CP is variable and can occur during the prenatal, perinatal, or postnatal period 40. Causes at presentation can be congenital, genetic, inflammatory, infectious, anoxic, traumatic, and metabolic 1. According to Rotta (2002), the main etiological factors in the prenatal period are infections and parasitic diseases such as syphilis, rubella, toxoplasmosis, cytomegalovirus, herpes simplex virus, and HIV. Congenital infections may reach the fetus via the placenta, causing serious lesions 14.
Some medications, such as thalidomide, have toxic and teratogenic effects 14. Exposure to X-rays for both diagnostic and therapeutic purposes has risks because it interferes with the development of the cerebral parenchyma 14,34.
Metabolic disorders of pregnant women, malnutrition (produces reduction in brain growth), and pregnancy toxemia are causes of CP 14. In addition, direct trauma to the abdomen or sitting falls among pregnant women are important factors 37. Anemia during pregnancy, cord circulation, placental abruption, uterine bleeding during pregnancy, eclampsia, and hypotension are causes of brain injuries 14. The genetic and chromosomal abnormalities, although rare, can occur at this stage 41. The factors that occur in the perinatal period (during or shortly after birth) 15 may contribute to CP 42. These events can be intracranial hemorrhage, hypoxic-ischemic encephalopathy, encephalopathy by hyperbilirubinemia, and periventricular leukomalacia. Intracranial bleeding can result from mechanical factors caused by compression of the head in the birth canal 14. Hypoxia is the most significant cause of CP due to lesions that are produced in the cerebral cortex and subcortex, the basal nucleus, and the cerebellum. During the perinatal period, the degree of acute asphyxia of the newborn can be evaluated by using the Apgar score 34. Premature dislocation of the placenta and cervical isthmus incontinence are important factors responsible for prematurity. Another factor considered is severe icterus of the newborn, which is responsible for bilirubin encephalopathy; if left untreated, bilirubin encephalopathy can produce devastating cortical lesions 14,15.
Advanced maternal age has been considered (in pregnant women >40 years of age) to increase the risk of sequelae to twice that of younger mothers 14. Postnatal factors occur between birth and 5 years 15. Postnatal causes can be infections (e.g., meningitis or encephalitis), traumatic brain injury, drowning, cardiac arrest during surgery, strokes, tumors, exposure to lead, and thrombosis by sickle cell anemia. The incidence of the causes varies according to geographic location and the availability of medical care 1,33.
Classification
CP is classified according to motor involvement and the topographic taxonomy indicating the ends involved 38 is still a matter of controversy in the literature 14. According to the affected area, CP is classified into monoplegia, hemiplegia, diplegia, and quadriplegia 44. Monoplegia is extremely rare and is characterized by the involvement of only one member (an arm or leg) 44. In hemiplegia, one side of the body is affected with the relevant amendments to the lesion suffered, where the arm is more affected than the leg. Over 60% of these individuals have normal intellectual development and are able to walk with or without assistance. They are considered at high risk for the development of partial convulsions. This type of CP is associated with vascular malformations in the brain and limited intraventricular hemorrhage in infancy 44. Diplegia occurs in 30%–40% of patients with spastic CP and is characterized by spasticity in the legs. Approximately 30% of these people have intellectual disabilities or learning difficulties. Most are able to walk independently or with assistance. Approximately 50% of these cases are associated with premature birth 44. In quadriplegia, all four of the patient's limbs are affected, and the trunk and the oromotor musculature are involved. This situation is responsible for 10%–15% of the cases of spastic CP. Most of these individuals have some degree of intellectual deficiency in addition to motor dysfunction. These patients are at high risk for seizures and sensory disabilities. This type of CP has been associated with suffocation and severe intraventricular hemorrhage in premature infants 44.
The clinical classification of CP can be divided into spastic, athetoid, ataxic, and mixed 5. As for motor impairment, the spasticity presents characteristics of the first motor neuron lesion (abnormal motor patterns, hyperreflexia, muscle weakness, reduced dexterity, and tremors) 8, hypertonia, and the presence of the Babinski sign with probable injury of the pyramidal system in the cerebral cortex motor 45. The movement of the extremities is made slowly and with great effort, and resistance to passive movements and abnormal motor patterns may not manifest clinically 46. The hypertonia is responsible for the imbalance between the agonist and antagonist muscles. Before that, it promotes an exaggerated increase in the tonus of the extensor muscles, inhibiting the flexor muscles, or otherwise increases the tone of the flexor muscles and inhibition of extensor 14. Spasticity is present in most of the cases of CP 8,14. The spastic form presents clinically as tetraparesis, hemiparesis, or diparesis 14.
Spastic tetraparesis is the most severe form of CP, owing to severe motor involvement of four members and the association with mental retardation and seizures 38. Clinical manifestations may be observed at birth and are accentuated with the development of the child 14. The increased tone and spasticity in all extremities, decrease of spontaneous movements, living reflexes, and plantar response extension are observed at neurological examination 38. Patients with CP of the tetraparesis type have facial hypertonia, little mime, upper lip retraction, lingual tension sometimes accompanied by tongue projection, open bite, bruxism, and ogival palate. Patients still have slow or shallow breathing, favoring an open mouth position and mouth breathing together with difficulty swallowing, dysphagia, absence of chewing, sucking hampered by muscle tension, and not allowing the effective labial sealing 47. These patients have difficulty in controlling the head because of the involvement of the upper limbs. These patients have frequent pulmonary infections and upper airway 14. In spastic diparesis or diplegia or Little's disease, spasticity predominates in the lower limbs, less severely affecting the upper limbs. The most common causes are prematurity with or without intraventricular hemorrhage and hydrocephalus. An adductor spasm is responsible for the leg and sharp spasticity can interfere with walking. The individual's intelligence and language are often unaffected 48.
The diplegic form is less severe than the tetraparetic form 49. The prognosis for typical intellectual development is excellent, being minimal the probability of seizures. Severe spastic diplegia is characterized by atrophy due to disuse, impaired growth of the lower extremities, and disproportionate growth with normal development of the upper trunk 48. The hemiparesis (hemiplegia) spastic elapses of an injury of the corticospinal system of a cerebral hemisphere 48. In this clinical pattern, movement disorders are observed in a hemibody 49. The causes are stroke in the intrauterine period or during childbirth. Another common cause is intraventricular hemorrhage. Seizures are frequent when the lesion affects the cortex 48. The intelligence and speech are less affected and disturbances in the articulation and rhythm may still be observed 49.
Athetoid CP, also called CP choreoathetosis or extrapyramidal CP 38, affects areas that modify or regulate movement in the extrapyramidal tract, causing involuntary movements and difficulty in voluntary movements 49. The affected patients are characteristically hypotonic, cannot support the head, and have a higher variability of tone with rigidity and dystonia over the course of several years 38. Changes in neurovegetative function are observed, such as arrhythmic breathing, mouth difficulty in sucking by incoordination of phonoarticulatory organs with chewing changes, and, in some cases, the presence of dysphagia 45. Moreover, tongue protrusion and sialorrhea are present, and nutrition can become difficult. Due to the involvement of oropharyngeal muscles, "speech" is typically affected and may be missing or indecipherable 38. Normally, these patients have exaggerated facial mime, repeated movements of opening, intraoral sensitivity, changes in the temporomandibular joint (TMJ), severe bruxism, and involuntary movements of the tongue, soft palate, or the facial musculature 47. Epileptic seizures are uncommon, and the intellect is preserved in many patients 38.
Ataxic CP is related to impairment of the cerebellum or cerebellar pathways. The main function of the cerebellum is to control balance and coordinate movements, and children with cerebellar lesions present ataxia 49. Clinical manifestations are motor incoordination 5 and static and dynamic balance disorders 49. In an ataxic clinical state, hypotonia is present and results in failure of the sequence of movements, generating some potential for tremor, postural maintenance deficiency, straightening reactions, and altered protection and balance, producing dysmetria in all actions 50. These patients present with lingual tremor and difficulty in graduating speed, strength, and size of movements 45. Ataxic CP is the rarest form of CP 49.
Mixed CP refers to the combination of the various manifestations of the disease, with dyskinesis and spasticity or ataxia with athetosis 48,49. The term is also used to describe patients who do not meet the written criteria for one of the main forms 48.
Clinical Characteristics and Oral Manifestations
In addition to the motor disturbances mandatory to characterize CP, affected individuals may have other variable frequency manifestations, such as mental retardation, seizures, language disorders, visual disturbances, behavioral disorders, orthopedic disorders 2, malnutrition conditions, obesity, and hydrocephaly 4,51. These patients may have difficulty in starting swallowing, inadequate sensitivity and mobility of oral structures, difficulty in controlling the tongue, hypersalivation, nasal regurgitation, inefficient mobility of laryngeal muscles, episodes of coughing, and bottleneck during feeding 52.
Swallowing disorders associated with postural deformities can result from wrong positioning of head, upper limbs, and chest, particularly kyphoscoliosis, and may lead to serious respiratory complications. Other factors that contribute to the development of respiratory problems are reduced level of consciousness, abnormal head postures, and dented respiratory function 39. The presence of diseases associated with brain damage, such as gastroesophageal reflux, oropharyngeal incoordination, and secretion accumulation, in addition to convulsions and motor incoordination, may contribute to the increased incidence of respiratory complications 53.
Patients with severe modifications of CP have learning disorders, language difficulty, behavior problems, and deficits in motor coordination and visuospatial perception 54,55. These changes interfere in children's acquisition of motor skills, which are essential for the performance of activities of daily living 56.
Neuromuscular problems typical of CP can significantly affect oral health, such as the change in growth patterns of maxillaries 6,7,57,58, the development of parafunctional habits, problems in chewing and swallowing 10,11, saliva control, respiratory disorders 12, and difficulties with maintaining oral hygiene 13.
The oral conditions often encountered are tooth decay, periodontal disease, bruxism 14,15, gingival hyperplasia 15,16, malocclusion, trauma 14,15, alteration in salivary flow, and alteration in oral reflexes 14.
Chewing alteration in these patients is conducive to different dietary habits, such as a more pasty diet rich in carbohydrates 9,14,61,62. In addition, chewing performed by kneading between the tongue dorsum and palate, incoordination of the masticatory muscles, and the accumulation of food waste associated with poor oral hygiene generate an increased prevalence of caries 14,58,59.
Patients with CP generally use medications such as phenytoin, nifedipine, and cyclosporine 14. These medications predispose individuals to gingival growth, along with the presence of bacterial plaque 14, excessive salivation due to lack of lip seal, and difficulty swallowing 16, which can induce the gingival inflammation process 14.
The malocclusion is prevalent in individuals with CP because of imbalance of the peri- and intraoral muscles 14 and mouth breathing 15. The conditions observed are protrusion of the upper anterior teeth, overbite, open bite, unilateral crossbite, and dental crowding 14. The soft tissue injury is caused by muscle contractions, malocclusions 15, bite reflexes, or suction, resulting in trauma of the lips, tongue, or jugal mucosa 14. Furthermore, these patients are prone to traumatization of the dental tissues, particularly of the upper anterior teeth, not only for their own protrusion but also due to the lack of a protective reflex 14. The saliva has several functions, including an important protective function for the maintenance and integrity of the oral tissues 60. In the setting of a neuromotor impairment, the release of saliva, which is regulated by the action of the sympathetic and parasympathetic systems, is compromised and does not occur in the normal way 63.
Hypersalivation is an involuntary increase in the salivary flow due to an inability to handle oral secretion, which can occur in patients with CP 65,66. The consequences include facial dermatitis, foul odor, increased perioral and oral infections, difficulty with hygiene, necessity of frequent changes of clothes, changes in the chewing process, and speech-related and aspiration risk 64,67. In CP, the pathophysiology of sialorrhea is not totally clear. Some authors believe it occurs through oromotor dysfunction, and others think that there is an association between hypersalivation and an insufficient mechanism for the removal of saliva 63,65. Patients with CP present with factors that predispose them to sialorrhea, such as difficulty in forming feed bolus, reduction of the lip seal, inability of sucking and chewing, poor cervical control, reduction of tongue movement, decreased oral sensitivity, malocclusion, dental incoordination of orofacial musculature, and airway obstruction 67,68. As a result of these factors, the deglutition mechanism is insufficient in promoting removal of saliva from the anterior portion of the mouth in the direction of the oropharynx 14.
Individuals with CP tend to present parafunctional habits, and bruxism is the most common 69. Lindqvist and Heibel noted that abnormal tooth wear is closely related to a low level of mental development and that severe tooth wear indicates that patients with CP have more severe bruxism than children without CP 17.
Bruxism
The term bruxism is derived from the Greek word brychein, which means clamping, abrasion, or friction between the teeth with force and without functional purpose. Bruxism is a parafunctional habit that may be considered as nonfunctional movements of the mandible, with or without sound, which may occur during the day or night 70,72.
The incidence of bruxism in the general population is around 21%, but the impact on the individual with CP is still unknown19. The causes of bruxism in CP are not yet well defined. However, some factors that may be involved are spasticity 17; oral myofunctional disorders 9,20; dysfunction of the vertebral column as the head projects forward, which changes the contact between the teeth and predisposes hyperactivity of the main masticatory muscles (temporal and masseteric) 17; lack of control of mandibular posture, which can worsen during periods of emotional stress 17; sleep disturbances 21; use of neuroleptics 20; and malocclusion 17. Some of these alterations are common in children with CP 20. During bruxism, excessive forces applied to the muscles lift the jaw (masseter, temporal, medial pterygoid, and lateral pterygoid), particularly in the closing movement, lateralization, and protrusion. When lateral forces are applied to the teeth and transcend the resistance threshold, periodontal adaptation occurs in the teeth that were subjected to these forces. Tooth mobility favors the appearance of diastemata, accumulation of food, and gum wounds 72 . In mixed dentition, bruxism can end with anterior guide 72, contributing to trauma of the posterior teeth during the movement of protrusion. In permanent teeth, this can cause crowding of the anterior teeth or aggravate already existing crowding, leading to the accumulation of bacterial plaque, tartar formation, and thereby the establishment of periodontal disease. In addition to these described changes, bruxism can cause dysfunction of the TMJ, headaches in the fibers of the temporal muscle and in the lateral and posterior regions of the neck, enlargement or thickening of the periodontal ligament, and wear facets on the posterior teeth and anterior 18.
Bruxism increases muscle tone, causing unilateral or bilateral hypertrophy of the masticatory muscles, especially the masseter. The hypertrophy and hyperfunction of this muscle can influence mandibular development during growth, leading to marked facial asymmetry 72. Hanson and Barrett (1995) related bruxism to other signs and symptoms, such as fatigue of nonmasticatory occlusion; irritability and/or tooth sensitivity; episodes of bites on the cheeks, lips, and/or tongue; and the presence of headaches 23.
Several types of treatment for bruxism has been investigated, such as occlusal plates, medication, and psychotherapy, but ineffectually 24,25. Traditionally, bruxism has been treated with occlusal plates to prevent tooth wear. However, the use of this dispositive in patients with spastic paralysis–type quadriplegia, is contraindicated because of the impossibility of voluntary removal by the same, causing a gingival enlargement, potential convulsive episodes, oral reflexes such as vomiting and tonic bite, and especially the change in intraoral sensitivity. Recently, local injection of BTX has been used in patients with various movement disorders, with BTX-A proposed to correct this disorder 26,27,73.
Botulinum Toxin
BTX is a potent biological toxin, also known as neurotoxin, produced by the anaerobic bacterium C. botulinum 29. It has a paralytic effect, inhibiting the release of acetylcholine at the neuromuscular junction 74. The toxin was initially studied for causing botulism, which is poisoning by the C. botulinum bacterium, where the neurotoxin reaches the myoneural junction, causing a clinical condition of diplopia, dysphagia, myasthenia, and respiratory insufficiency, which can be fatal 71. According to Siqueira (2004), this in fact occurs only in contact with high doses of the toxin.
The bacterium C. botulinum has eight subtypes (A–G) that produce seven distinct neurotoxins. They are similar in structure and function but differ from each other by the receptor location in neurons and their mechanism of cellular action, potency, and duration of effect. BTX-A is the toxin scientifically recognized as being the most powerful, having a longer-lasting effect and is conventionally used commercially for therapeutic purposes 76. The BTXs consist of protein complexes that include the neurotoxic subdivision, of approximately 150 kDa, and one or more nontoxic proteins that correspond to around 70% of the total mass 76. BTX is a potent biological neurotoxin that is safe and effective for the treatment of several neurological disorders 28,29. Scott (1979) used BTX therapeutically for the first time for strabismus correction by injecting toxin in the external eye muscles 74. The action of the toxin occurs by blocking the release of acetylcholine (a neurotransmitter responsible for transmitting electrical messages from the brain to the muscles) at the neuromuscular junction, causing a process of decreasing muscle contraction. As the condition first develops, when there is excessive muscle contraction, the toxin becomes beneficial clinically and therapeutically 76. In patients with CP, it has been employed in the control of muscle contraction of the gastrocnemius muscles, hamstrings, hip adductors, brachial biceps, and flexor muscles of the fingers 77.
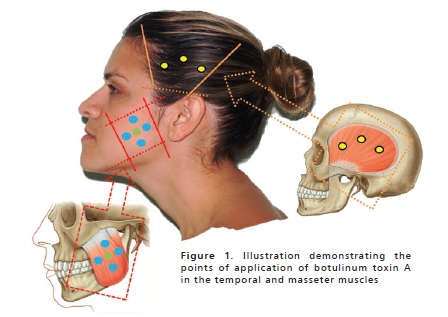
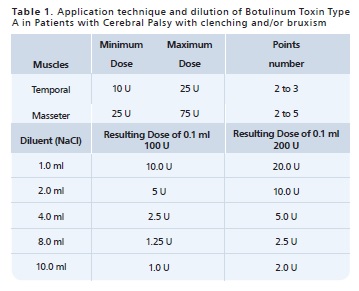
BTX-A is a biological agent obtained in the laboratory. It is a stable, crystalline substance, lyophilized with human albumin, used after dilution in saline solution, and measured in biological units. The effects begin from 1 to 7 days after administration and last an average of 3–6 months 75,76. The dosage of BTX-A used varies according to the size of the target muscle, contraction intensity, and response to initial treatment. The application of BTX-A in the masticatory muscles of patients with CP is described in Table 1. The extent of this transient denervation is dependent on the dose and volume of the toxin 29. In recovery, sprouts, reinnervation, and formation of new, smaller end plates are formed 76. BTX-A is contraindicated in patients with neuromuscular disease who are receiving aminoglycosides and in pregnant and lactating women 78. BTX has been used for therapeutic purposes in the control of pain and mandibular dysfunction such as bruxism, masseter hypertrophy, sialorrhea, gummy smile, and recently in the prophylactic reduction of muscle strength of the masseter and temporal muscles, in some cases of immediate load in implantology 79-83. The points of application in these muscles are shown in Figure 1. This substance is extensively used in the treatment of bruxism in patients with special needs 28,75.
Manzano evaluated six patients with spastic quadriplegic CP being treated with BTX-A regarding the presence or absence of bruxism, spasticity, difficulty in performing oral hygiene, and lip trauma. In that study, the injection of BTXA was well tolerated, safe, and effective for the treatment of children with spastic tetraplegic CP. That study also demonstrated a reduction in muscle spasticity, lower lip trauma, bruxism, and the ability to perform oral hygiene 19.
Freud et al. (1999) demonstrated that injection of BTX-A in the masseter and temporal muscles resulted in subjective reduction of pain and sensitivity among patients with neurological disorders diagnosed with temporomandibular dysfunction. This occurs by reduction of spasticity of the masseter and bilateral temporal muscles on palpation and increased interincisal opening 84.
Kesikburun et al. (2014) reported a case of a patient who, after a car accident, had significant brain sequelae associated with intense tooth wear caused by nocturnal bruxism that started 2 months after the accident. The application of BTX-A in the masseter and temporalis muscles led to a significant decrease in this condition 3 days after the first injections 85. Systemic side effects and local complications are uncommon with the use of BTX-A. When reported, they are related to the dose and secondary effects, such as transient weakness, nausea, and pruritus 29,86.
Wash your face with water and antiseptic soap. Apply a topical anesthetic (lidocaine cream 25 mg and prilocaine 25 mg or lidocaine cream to 4%) and ice mask. For dilution, remember that after toxin reconstitution, it should be used after 72 h. The early effect of toxin action takes 48–72 h with a peak of 7 and 15 days of accommodation with a duration of 4–6 months.
Conclusion
Bruxism is observed more frequently in patients with CP than in individuals without such compromise. This fact is related to clinical conditions present in individuals with CP that contribute to the increased prevalence of parafunctional habits. BTX-A is well tolerated, safe, and effective as an alternative treatment modality for bruxism in patients with CP, leading to reduced muscle spasticity and lower lip trauma and improved opening of the mouth and oral hygiene.
Referências
1. Zanini G, Cemin, NF, Peralles SN. Cerebral Palsy: Causes and prevalence. Fisioter Mov. 2009; 22:375-81. [ Links ]
2. Leite JMRS, Prado GF. Cerebral palsy Physiotherapeutic and Clinical aspects. 2004.
3. Bacheschi LA. The Neurology wich Every Doctor Should Know. 2. ed. São Paulo: Atheneu, 2003.
4. Sawyer JR. Cerebral palsy. In: Canale ST, Beaty JH, eds. Campell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby Elsevier. 2008:1333e1399.
5. Gauzzi LDV, Fonseca LF. Cerebral Palsy Classification. In: Lima CLA, Fonseca LF. Cerebral Palsy- Neurology, Orthopedics, Rehabilitation. 1. ed. Rio de Janeiro: Guanabara Koogan. 2004.
6. Abanto J, Bortolotti R, Carvalho TS et al. Nutrition habits evaluation of dental interest in children with cerebral palsy. Rev Inst Cienc Health. 2009;27(3):244-8.
7. Miamoto CB, Ramos-Jorge ML, Pereira LJ et al. Severity of malocclusion in patients with cerebral palsy: determinant factors. Am J Orthod Dentofacial Orthop. 2010;138(4):394-5.
8. Arruda MCV. Condições bucais de pacientes com paralisia cerebral: aspectos clínicos e microbiológicos. Dissertação. Faculdade de Odontologia de Araçatuba, Universidade Estadual Paulista "Júlio de Mesquita Filho". 2011.
9. Santos MT, Nogueira ML. Infantile reflexes and their effects on dental caries and oral hygiene in cerebral palsy individuals. J Oral Rehabil. 2005;32(12):880-5.
10. Buchholz D, Robbins J. Neurologic diseases affecting oropharingeal swallowing. In: Perlman A, Schulze-Delrieu K, editors. Deglutition and its disorders. San Diego: Singular Publishing Group. 1997:319-42.
11. Mariri BP, Levy SM, Warren JJ et al. Medically administered antibiotics, dietary habits, fluoride intake and caries experience in the primary dentition. Community Dent Oral Epidemiol. 2003;31:40-51.
12. Ribeiro J, Caon G, Beltrame JS. Perfil motor de criança com encefalopatia crônica não progressiva- implicações para a intervenção profissional. Dyn rev tecno- científ 2008;3:42-5.
13. Dougherty NJ. A review of cerebral palsy for the oral health professional. Dent Clin North Am. 2009;53(2):329-38.
14. Haddad AS. Odontologia para Pacientes com Necessidades Especiais. Editora Santos. 2007, p.164.
15. Varellis MLZ. O paciente com necessidades especais na Odontologia. Manual prático. Santos. 2005.
16. Aurélio SR, Genaro KF, Macedo-Filho ED. Análise comparativa dos padrões de deglutição de crianças com paralisia cerebral e crianças normais. Revista Brasileira de Otorrinolaringologia. 2002;68(2):167-73.
17. Oliveira AIA, Golin MOM, Cunha MCB. Aplicabilidade do sistema de classificação da função motora grossa (GMFCS) na paralisia cerebral- revisão de literatura. Arq Bras Ciên Saúde, Santo André.set/dez 2010;35(3):220-4.
18. Molina OF. Fisiopatologia Craniomandibular. São Paulo, Pancast, 1995.677p.
19. Manzano FS, Granero LM, Masiero D. Treatment of muscle spasticity in patients with cerebral palsy using BTX-A: a pilot study, Special Care in Dentistry. 2004; 24(4):235-9.
20. Peres ACD, Ribeiro MO, Juliano Y. "Occurrence of bruxism in a sample of Brazilian children with cerebral palsy," Special Care in Dentistry. 2007;27(2):73-6.
21. Weideman CL, Bush DL, Yan-Go FL. "The incidence of parasomnias in child bruxers versus nonbruxers," Pediatric Dentistry. 1996;18(7):456-60.
22. Ramfjord S, Ash MM. Oclusion. Rio de Janeiro, Interamérica, 1972. 400p.
23. Hanson ML, Barret RH. Fundamentos de Miologia Orofacial. Rio de Janeiro: Enelivros, 1995.
24. Lee SJ, Mccall WDJR, Kim YK. Effect of botulinum toxin injection on nocturnal bruxism: A randomized controlled trial. Am J Phys Med Rehabil. 2010;89:16-23.
25. Saletu A, Parapatics S, Saletu B, et al. On the pharmacotherapy of sleep bruxism: Placebo-controlled polysomnographic and psychometric studies with clonazepam. Neuropsychobiology. 2005;51:214-25.
26. Van Zandijcke M, Marchau MM. Treatment of bruxism with botulinum toxin injections. J Neurol Neurosurg Psychiatry. 1990;53:530.
27. Guarda-Nardini L, Manfredini D, Salamone M, et al. Efficacy of botulinum toxin in treating myofascial pain in bruxers: A controlled placebo pilot study. Cranio 2008;26:126-35.
28. Levitt SO. Tratamento da Paralisia Cerebral e do Retardo Motor. 3. ed. São Paulo: Manole, 2001.
29. Jankovic J, Schwartz K. Botulinum toxin treatment of cranial cervical dystonia, spasmodic dysphonia, other focal dystonias and hemifacial spasm. J Neurol Neurosurg Psychiatty. 1990; 53(8):633-9.
30. Choi YS, Choung PH, Moon HS, et al. Temporomandibular Disorders in 19-Year-Old Korean Men. J Oral Maxillofac Surg. 2002;60:797-803.
31. Phillip G, Monroy DDS, Marcio AFDDS. The Use of Botulinum Toxin-A in the Treatment of Severe Bruxism in a Patient with Autism: A Case ReportSpec Care Dentist. 2006;26(1).
32. Boyle C, Decoufle P, Yeargin-Allsopp M. Prevalence and health impact of developmental disabilities in US children. Pediatrics. 1994:93:399-403.
33. Thorogood, C. Cerebral palsy. E Medicine. 2001.
34. Rotta NT. Paralisia cerebral, novas perspectivas terapêuticas. J Pediatr (Rio J). 2002;78(Supl.1):S48-S54.
35. Diament, A, Cypel, A. Neurologia Infantil. 3ª ed. São Paulo, Atheneu. 1996. p.781-98.
36. Robertson C, Sauve RS, Christianson HE. Province-based study of neuro- logic disability among survivors weighing 500 through 1249 grams at birth. Pediatrics. 1994;93:636-40.
37. Rotta NT. Encefalopatia crônica da infância ou paralisia cerebral. In: Por¬to CC. Semiologia Médica. 4. ed. Rio de Janeiro: Guanabara Koogan. 2001, p.1276-8.
38. Behrman RE, Robert M, Kliegman HJ, et al. Nelson Tratado de Pediatria. 18ª Ed. Editora Elsevier, 2009.
39. Furkim AM, Behlau MS, Weckx LLM. Avaliação clínica e videofluoroscópi¬ca da deglutição em crianças com paralisia cerebral tetraparética espástica. Arq Neuro-Psiquiatr. 2003;61:611-6.
40. Kuban KCK, Leviton A. Cerebral palsy. N Engl J Med. 1994;20:188-95.
41. Assis-Madeira EA, Carvalho SG. Paralisia cerebral e fatores de risco ao desenvolvimento motor: Uma revisão teóricacadernos. Cardenos de Pós-Graduação em Distúrbios do Desenvolvimento, São Paulo. 2009;9(1):142-63.
42. Kok F. As Principais Afecções em Neurologia Infantil – Encefalopatias Não-Progressivas: deficiência mental e paralisia cerebral. 2003.
43. Katherine T, Ratliffe MA. Paralisia Cerebral. In: Katherine T, Ratliffe MA. Fisioterapia na Clínica Pediátrica: guia para equipe de fisioterapeutas. São Paulo: Editora Santos, 2002. p. 163-217.
44. Thorogood C, Alexander MA. Cerebral palsy e medicine [cited 2009 Dec.14]. 2007.
45. Mayer NH. Clinicophysiologic Concepts of Spasticity and Motor Dys-function in Adults with an Upper Motoneuron Lesion. Muscle & Nerve. 1997;supl.6:1-13.
46. Bobath K. Uma Base Neurofisiológica para o Tratamento da Paralisia Cerebral. 2. ed., São Paulo: Manole,1989.
47. Segovia ML. Interrelaciones entre la odontoestomatología y la fonoaudiologia. 2. ed. Buenos Aires: Panamericana, 1995.
48. Rowland LP. Merritt - Tratado De Neurologia – 18. ed. Editora Guanabara Koogan, 2007.
49. Gomes C, Santos CA, Silva JUA, et al. Paralisia Cerebral. In: Lianza S. Medicina de Reabilitação. 3. ed. Rio de Janeiro: Guanabara Koogan, 2001. Cap. 20, p.281-98.
50. Edwards S, Silva MGF. Fisioterapia Neurológica: uma abordagem centrada na resolução de problemas. Porto Alegre: Artes Médicas, 1999.
51. Hoffer MM, Brink J. Orthopedic management of acquired cerebrospasticity in childhood. Clin Orthop Relat Res. 1975;110:244-8.
52. Clavé P, De Kraa M, Arreola V, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24(9): 1385-94.
53. Mello SS, Marques RS, Saraiva RA. Complicações respiratórias em pacien-tes com paralisia cerebral submetidos à anestesia geral. Rev Bras de Anestesil. 2007;57:455-64.
54. Magalhães LC, Catarina PW, Barbosa VM, et al. Estudo comparativo sobre o desempenho percptual e motor na idade escolar em crianças nascidas em pré-termo e a termo. Arq Neuro-Psiquiatr. 2003;61(2A):250-5.
55. Rosenbaum P. Cerebral palsy: What parents and doctors want to know. BMJ. 2003;326:970-4.
56. Cury VCR, Mancini MC, Melo AP, et al. Efeitos do uso de órtese na mobilidade funcional de crianças com paralisia cerebral. Ver Bras Fisioter. 2006;10(1) 326:970-4.
57. Reuland-Bosma W, Van Der Reijden WA, Van Winkelhoff AJ. Absence of a specific subgingival microflora in adults with Down's syndrome. J Clin Periodontol. 2001;28(11):1004-9.
58. Rodrigues dos Santos MT, Masiero D, Novo NF, et al. Oral conditions in children with cerebral palsy. J Dent Child. 2003;70(1):40-6.
59. Guare RE, Ciamponi AL. Dental caries prevalence in the primary dentition of cerebral-palsied children. J Clin Pediatr Dent. 2003;27(3):287-92.
60. Edgar WM. Saliva: Its secretion, composition and functions. Br Dent J. 1992;17:305-12.
61. Camargo MA, Antunes JL. Untreated dental caries in children with cerebral palsy in the Brazilian context. Int J Paediatr Dent. 2008;18(2):131-8.
62. Nicholson AL, Eddy TP. Food habits in cerebral palsy. Public Health. 1967;81(4):167-75.
63. Rosa CMR, Lopes RA, Santos FF, et al. A crioterapia como recurso para diminuir a sialorréia em crianças com disfunção motora: relato de caso. Revista CEFAC. 2006;7(3):300-6.
64. Masiero D, Simionato MR. Risk factors for dental caries in children with cerebral palsy. Spec Care Dentist. 2002;22:103-7.
65. Meningaud JP, Pitak-Arnnop P, Chikhani L, et al. Drooling of saliva: A review of the etiology and management options. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2006;101:48-57.
66. Lal D, Hotaling AJ. Drooling. Curr Opin Otolaryngol Head Neck Surg. 2006;14:381-6.
67. Morales-Chávez MC, Nualart-Grollmus ZC, Silvestre-Donat FJ. Clinical prevalence of drooling in infant cerebral palsy. Med Oral Patol Oral Cir Bucal. 2008;13:E22-6.
68. Rosen F, Bailey B. Anatomy and physiology of the salivary glands. Grand Round Presentation, UTMB, Dept of Otolaryngology. [on line] 2001.
69. Ortega AO, Guimaraes AS, Ciamponi AL, et al. Frequency of parafunctional oral habits in patients with cerebral palsy. J Oral Rehabil. 2007;34(5):323-8.
70. Varedas AP, Manetas KJ. Relationship between malocclusion and bruxism in children and adolescents: a review. Pediatr Dent. 1995;17(1):7-12.
71. Junqueira CKVC. Toxina botulínica aplicada nas desordens temporomandibulares. Monografia apresentada a Faculdade de Odontologia São Leopoldo Mandic para obtenção de Especialista em Disfunção Temporomandibular e Dor Oro-facial. 2008.
72. Cezaro, GG. Bruxismo e suas implicações no sistema estomatognático e no crescimento craniofacial. Monografia de conclusão do curso de especialização em Motricidade Oral. Porto Alegre,1999.
73. Redaelli A. Botulinum Toxin A in Bruxers. Saudi Med J. 2011;32(2):156-8.
74. Laskawi R. The use of botulinum toxin in head and face medicine: An interdisciplinary field. Head & Face Medicine. 2008;4:5.
75. Siqueira B. A utilização da toxina botulínica do tipo A (BOTOX®) no tratamento da espasticidade [texto na internet]. 2004 [citado 2008 jan 18].
76. Unno EK, Sakata RK, Issy AM. Estudo comparativo entre toxina botulínica e bupivacaína para infiltração de pontos-gatilho em Sindrome miofascial crônica. Rev Bras Anestesiologia. 2005;55(2):250-5.
77. Tedesco AP, Martins JS, Nicolini-Panisson RD. Tratamento focal da espasticidade com toxina botulínica A na paralisia cerebral GMFCS nível V – Avaliação de efeitos adversos. Rev Bras Ortop. 2014;49:359-63.
78. Brin MF. Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Supp.l 1997;6:S146-68.
79. Hoque A, Mc Andrew M. Use of botulinum toxin in dentistry. N Y State Dent J. Nov. 2009;75(6):52-5.
80. Klein FHMS, Sato MS, Helmer KA, et al. Lower facial remodeling with botulinum toxin type A for the treatment of masseter hypertrophy. An Bras Dermatol. 2014;89(5):878-84.
81. Nayyar P, Kumar P, Nayyar PV, et al. Botox: Broadening the Horizon of Dentistry. Journal of Clinical and Diagnostic Research. 2014;8(12):ZE25-9.
82. Tinastepe N, Kuçuk BB, Oral K. Botulinum toxin for the treatment of bruxism. The Journal of Craniomandibular & Sleep Practice. 2014.
83. Sevim S, Kaleagasi H, Findanci H. Sleep bruxism possibly triggered by multiple sclerosis attacks and treated successfully with botulinum toxin: Report of three cases. Multiple Sclerosis and Related Disorders. 2015;4:403-5.
84. Freund B, Schwartz M, Symington JN. The use of botulinum toxin for the treatment of temporomandibular disorders: Preliminary finding. J Oral Maxillofac Surg.1999;57:916-20.
85. Kesikburun S, Alaca R, Aras B, et al. Botulinum toxin injection for bruxism associated with brain injury: Case report. JRRD. 2014;4(51):661-3.
86. Dutton JJ. Botulinum-A toxin in the treatment of craniocervical spasms: short-and long-term, local and systemic effects. Suw Ophthalmol. 1996;4151-65.
 Endereço para correspondência:
Endereço para correspondência:
Bruna Michalski dos Santos
Brazilian Dental Association - Rio de Janeiro
Dental Center for Special Patients
Street: Barão de Sertório, 75 - Rio Comprido
Rio de Janeiro/RJ, Brasil – CEP: 20261-050
e-mail: copeaborj@yahoo.com
Recebido: 25/08/2015
Aceito: 29/09/2015













