Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RFO UPF
versão impressa ISSN 1413-4012
RFO UPF vol.15 no.3 Passo Fundo Set./Dez. 2010
Evaluation of the mechanical properties of light-cure composite resins submitted to post-cure
Avaliação das propriedades mecânicas de resinas compostas fotoativáveis submetidas a ativação complementar
Luciano de Oliveira Martins JuniorI; João Maurício Lima de Figueiredo MotaII; Ricardo Rodrigues VazIII; Wagner Reis da Costa CamposIV
IMestre em Materiais Dentários, Faculdade de Odontologia da Universidade Vale do Rio Verde de Três Corações, Departamento de Odontologia Restauradora, Belo Horizonte, MG, Brasil
IIMestre e Doutor em Materiais Dentários, Faculdade de Odontologia da Universidade Federal de Minas Gerais, Departamento de Odontologia Restauradora, Belo Horizonte, MG, Brasil
IIIMestre em Reabilitação Oral e Doutor em Materiais Dentários, Faculdade de Odontologia da Universidade Federal de Minas Gerais, Departamento de Odontologia Restauradora, Belo Horizonte, MG, Brasil
IVDoutor em Metalurgia, Comissão Nacional de Energia Nuclear/Centro de Desenvolvimento da Tecnologia Nuclear, Belo Horizonte, MG, Brasil
ABSTRACT
OBJECTIVE: This study evaluated the flexural strength and Vickers hardness of a direct restorative composite resin (Filtek P-60TM), submitted or not to the post-cure, and a laboratory composite resin (ArtglassTM).
METHODS: The flexural strength tests followed the ISO 4049:1988 regulations, and the Vickers microhardness tests the ASTM E-384:1999 regulations. The Filtek P-60TM composite resin was cure activated as follows: Group I - conventional light cure; Group II - conventional light cure followed by post-cure with dry heat; Group III - conventional light cure followed by post-cure in a stroboscopic light unit; Group IV - ArtglassTM composite resin was light cured in a stroboscopic unit. After cure activation procedures, the samples were kept in deionized water at 37 ± 1 ºC for 24h and protected from light. Results were submitted to Anova and Duncan's test and revealed an increase in flexural strength and Vickers microhardness test after Filtek P-60TM post-cure.
RESULTS AND CONCLUSION: It is possible to conclude that the Vickers microhardness values for Filtek P-60TM samples were superior to the ArtglassTM composite resin values; and that the flexural resistance values for Filtek P-60TM submitted to post-cure were superior to the ArtglassTM resin values.
Key words: Resin composite. Mechanical properties. Post-cure.
RESUMO
OBJETIVO: Este estudo avaliou a resistência à flexão e microdureza Vickers de uma resina composta direta (Filtek P-60®), submetida ou não a ativação complementar, e uma resina composta laboratorial (Artglass®).
MÉTODOS: Os ensaios de resistência à flexão seguiram a normatização ISO 4049:1988, e os ensaios de microdureza Vickers seguiram a normatização ASTM E-389:1999. A resina composta Filtek P-60® foi ativada da seguinte forma: Grupo I - fotoativação convencional; Grupo II - fotoativação convencional seguida por ativação complementar com calor seco; Grupo III - fotoativação convencional seguida por ativação complementar com luz estroboscópica. O Grupo IV foi composto pela resina composta laboratorial Artglass® fotoativada numa unidade de luz estroboscópica. Após os procedimentos de ativação as amostras foram armazenadas em água deionizada a 37 ± 1 ºC por 24h num recipiente fechado, protegido de luz.
RESULTADOS E CONCLUSÃO: Os resultados foram submetidos aos testes Anova e Duncan, que revelaram um aumento na resistência à flexão e microdureza Vickers para a resina composta Filtek P-60® submetida à ativação complementar.
Palavras-chave: Resina composta. Ativação complementar. Propriedades mecânicas.
Introduction
Since the introduction of composite resins in Dentistry, significant advances have been observed in the sense of improving their physical and mechanical characteristics. However, composite resins still present limitations such as polymerization contraction, difficulties in establishing proximal contacts with adjacent teeth through direct techniques, color instability, post-operative sensitivity and inadequate resistance to abrasion1-3.
Flexural strength can be understood as the collective measurement of tensile, compression and shear stresses while hardness can be defined as the resistance a material has towards indentation of its surface4. Flexural strength and hardness tests are of great relevance or the evaluation of restorative material resistance, being the materials that present elevated flexural resistance are less prone to fractures5. The durability of esthetic restorations in composite resin is directly influenced by the polymerization of the material. Proper polymerization represents one of the main causes for clinical failure of these materials, disabling the capacity of achieving desirable physical, mechanical and biological properties3,6.
With the objective of enhancing properties such as flexural strength, microhardness and color stability, some direct composite resin systems are based on light-cure activation followed by a complementary activation with laboratory light-cure units, heating or the combination of both, named as complementary activation or post-cure7-12. There is a consensus in literature that the heat increase the mechanical properties of cured composites with improved conversion degree and a consequent reduction of unreacted monomers2,3,13.
Thus, the aim of this study was to verify the influence of two post-cure techniques on flexural resistance and Vickers microhardness of a light-cure composite resin as well as to compare these properties to those of a laboratory composite resin processed according to the manufacturer's instructions, testing the hypotheses that the composite resin submitted the post-cure produce higher flexural strength and microhardness values than laboratory composite.
Materials and method
This study was performed with the composite resin Filtek P-60TM (3M Dental Products, St. Paul, MN, EUA)14; shade A3, indicated for direct and indirect fillings, and the composite resin ArtglassTM (Heraus Kulzer, Wehrhein, Hessen, Germany), shade DA3, indicated for indirect restorations (Square 1).
The flexural strength tests were accomplished according to ISO 4049:2000 criteria. The samples were obtained through a metallic matrix split in two, forming a rectangular cavity with 25 mm length X 2 mm width X 2 mm high dimensions15.
Thirty samples of resin composite Filtek P-60TM were confectioned and randomly distributed in three experimental groups with 10 samples each: Group I - conventional light-cure; Group II post-cure with dry heat after conventional light-cure; Group III - post-cure with a laboratory light-cure unit after conventional light-cure. The composite resin Filtek P-60TM was incrementally placed in the metallic matrix and a glass lamina was positioned over the composite resin using digital pressure. In Group I, conventional light-cure was performed by using two Optlight PlusTM (Gnatus, Ribeirão Preto, SP, Brazil) light-cure units, with a pointer of 10 mm of diameter, with a irradiance of 500 mW/cm2; checked by the radiometer GnatusTM. Light-cure initially occurred at the center of the metallic matrix for 40s, and then towards both extremities, with the aid of both light-cure units for a further 40s each. The sample was then removed from the metallic matrix, placed up-side-down and the previously described light-cure procedure was achieved, totalizing 240s for each sample. In Group II, post-cure with heat was applied by using a Dental KlinTM (Odontobrás, Ribeirão Preto, SP, Brazil), previously calibrated to generate dry heat at 120 ºC for 600s. In Group III, post-cure with light was performed with a UniXSTM (Heraus Kulzer, Wehrhein, Hessen, Germany) light unit with two xenon stroboscopic light bulbs, for 180s in each side of the sample.
The laboratory composite resin ArtglassTM was incrementally placed in the metallic matrix and a glass lamina was placed over it, using digital pressure. After the insertion of the composite resin, light-cure was performed by using a UniXSTM laboratory light-cure unit for 180s. The matrix was then turned up-side-down, and the light-cure procedure described was repeated, totalizing 360s for each sample. Ten samples were confectioned with ArtglassTM laboratorial composite resin (Group IV).
After the activation procedures, the samples were kept in deionized water at 37 ± 1 ºC for 24h, in a biological kiln, in a dark receptacle, protected from light.
Flexure tests were fulfilled by means of a universal testing machine Instron which was charged with a cell of load of 100N at a cross-head speed of 0.5 mm/min.
Vickers micro-hardness testing followed the ASTM E-384:1999 criteria. Samples were confectioned with the aid of a PVC matrix with a diameter of 5 mm and 2 mm thick placed over a glass slab16.
Filtek P-60TM composite resin was incrementally placed inside the PVC matrix and a glass lamina was placed over it. After insertion with composite resin, conventional light-cure was performed by using the OptlightTM light-cure unit. The matrix was then turned up-side-down, and the previously described light-cure procedure was repeated, totalizing 80s of light exposure for each sample. The post-cure method was the same as that performed for the flexure test. Fifteen samples were confectioned with Filtek P-60TM composite resin and were randomly distributed in three experimental groups previously described.
The laboratory composite resin, ArtglassTM; was incrementally placed inside the PVC matrix and a glass lamina was placed over it using digital pressure. After the insertion of composite resin, light-cure was accomplished by using a UniXSTM laboratory light-cure unit for 180s. The matrix was then turned up-side-down, and the light-cure procedure described was repeated, totalizing 360s for each sample. Five samples were confectioned with ArtglassTM laboratorial composite resin (Group IV).
After activation, all samples were kept in deionized water at 37 ± 1 ºC for 24 hours in a bacteriological kiln, in dark receptacles, protected from light.
Vickers micro-hardness tests were performed by using a Durimet (Vickers LeitzTM; Wetzlar, Hessen, Germany) microhardness tester with a 50 gF load, for 15s. Five indentations marks were made on one surface of the each sample.
The flexural strength and Vickers microhardness values were submitted to statistic analysis and the averages to Duncan's multiple comparison tests (p < 0.05).
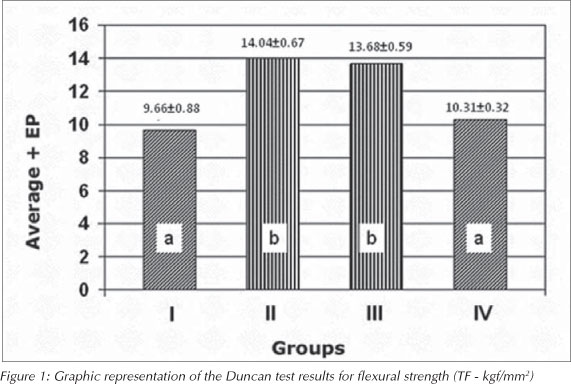
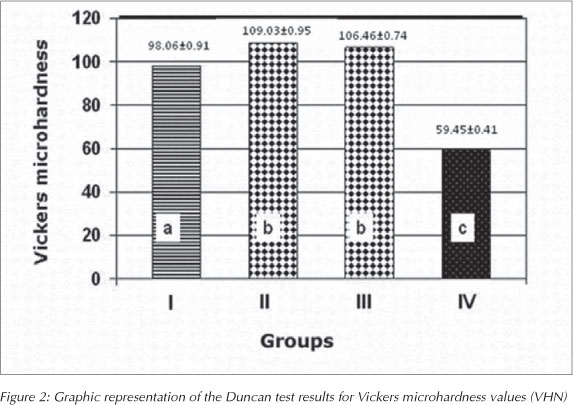
In order to evaluate differences in the interest averages between groups, Anova models and Duncan's multiple comparison tests to compare treatments (groups) in pairs were used. The results are shown on Figures 1 and 2. The analysis was performed with the SPSS 11.5 Inc. software (Statistical Package for Social Sciences).
Different colors indicate statistically significant differences
Different colors indicate statistically significant differences
Results
The mean values and standard deviations of flexural strength and microhardness and statistical grouping are shown in Tables 1 and 2.
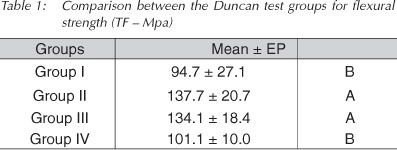
Different letters indicate statistically significant differences between groups (p < 0.05)
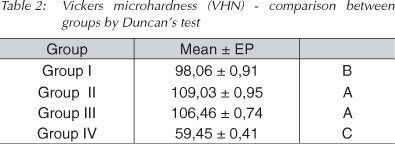
Different letters indicate statistically significant differences between groups (p < 0.05)
Discussion
The direct composite system studied submitted to post-cure produced values of flexural strength and microhardness higher than the laboratory composite resin, thus confirming the study hypotheses.
Among the esthetic materials available in the market, the choice frequently lies between ceramic or indirect resin restorations. History has shown that throughout time, interest as regards dental ceramics has been inconstant. Even so, this material became established as the first choice for reproducing natural teeth. Ceramics may be considered as an excellent option for esthetic restorative material. They are biocompatible, resistant to compression, have heat conductivity similar to that one of dental tissues, marginal integrity, color stability, good resistance to abrasion, and retain less bacterial plaque. Nevertheless, there are still limitations, such as technique sensitivity, high cost, and when compared with laboratory resin composites they are not effectively repaired17,18 .
Post-cure with 100 °C during seven minutes, between five and thirty minutes after initial activation, was responsible for a higher increase in flexural strenght19. Also, post-cure between 125 °C and 150 °C during one hour on an experimental composite, resulted in higher values of flexural strength. However, the values found were not statistically different when post-cure lasted 10 min2 only. Therefore, in this study, 10 min post-cure with heat was used, in order to considerably increase bending and hardness strength of the studied composite during a short period. This reduction in time is important to allow the dental surgeon to perform a faster procedure.
The present study both groups submitted to complementary activation (Groups II and III) showed a statistically similar increase in flexural strength: around 35% in comparison with the control group (Group I) and with the laboratorial composite resin ArtglassTM (Group IV). Composite resins submitted to post-cure, regardless the activation method, showed an increase of 11% on flexural strength11.
In this study, the composite resin Filtek P-60TM; which was not submitted to post-cure (Group I), and the composite resin ArtglassTM (Group IV), showed statistically similar mean bending strength values. It was possible to conclude that different chemical compositions and different activation units showed statistically similar flexural strength values. Another study evaluated the flexural strength and hardness of direct and indirect composites, and concludes that the direct composite systems with higher filler contents had higher mean and values than the indirect composites20.
Groups II and III, submitted to post-cure, showed mean flexural strength values and were not statistically different. Three post-cure methods using light and heat, heat and pressure and microwave cycles, did not reveal statistical differences in flexural strength of composite resins7.
Previous studies has widely described that particle incorporation in composite matrixes provide better mechanical properties9. No direct relation between the inorganic particle content of composite resins and flexural strength was found5,21. This fact makes it important to analysis the organic matrix formulation of composite resin, source, time, intensity and direction of light-cure and presence of complementary activation for the evaluation of the mechanical properties of composites.
Hardness reflects the conversion degree of composite resins and is more related to the organic matrix content of composite resins22. The presence of unpolymerize monomers in the matrix may induce surface degradation of the composite resins23. The results of the present study showed that the Vickers microhardness values for Group I were highly superior to the Vickers microhardness values found for Group IV. Therefore, the organic matrix of the composite resin Filtek P-60TM is more susceptible to the monomeric conversion than the laboratorial composite resin ArtglassTM. Another study found that the Vickers microhardness values for the composite resin ArtglassTM inferior to the values found for the direct composite resin HeliomolarTM (Ivoclar-Vivadent), with an organic matrix basically composed of Bis-GMA and UDMA24.
Similar results were observed when the direct/indirect composite resins TPHTM (Dentsply) and Filtek P-60TM (3M ESPE) were submitted to post-cure. They showed better mechanical properties (hardness and diametral strength) than the laboratorial composite resin SolidexTM (Shofu) which has an organic matrix basically composed of multifunctional resin co-polymers and UDMA3.
Evaluation of the clinical heat post-cure performance of the composite resin OclusinTM; by using the US Public Health Service criteria, showed that it was responsible for making the resin matrix more resistant to intra-oral fractures, improved the marginal integrity and reduced the rates of post-operatory sensibility. However, these results did not persist after 12 months25. Further clinical evaluations must be undertaken periodically in order to verify the maintenance of the increase in bending strength and Vickers microhardness of composite resin Filtek P-60TM submitted to post-cure.
Conclusions
- Post-cure of the composite resin Filtek P-60TM; either by light or heat, increased flexural strength and Vickers microhardness with statistically significant values compared to conventional activation.
- Flexural strength values for the composite resin Filtek P-60TM; submitted to conventional activation only, were statistically similar to flexural strength values of the laboratorial composite resin ArtglassTM.
- Vickers microhardness values of the composite resin Filtek P-60TM; submitted to conventional activation only, were statistically superior to the Vickers microhardness values of the laboratorial composite resin ArtglassTM.
References
1. Kawano F, Ohguri T, Ichikawa T, Matsumoto N. Influence of thermal cycles in water on flexural strength of laboratory-processed composite resin. J Oral Rehabil 2001; 28(8): 703-7. [ Links ]
2. Peutzfeldt A, Asmussen E. Effect of temperature and duration of post-cure on selected mechanical properties of resin composites containing carboxylic anhydrides Scand J Dent Res 1992; 100(5):296-8. [ Links ]
3. Soares C J, Pizi ECG, Fonseca RB, Martins LRM. Mechanical properties of light-cured composites polymerized with several additional post-curing methods. Oper Dent 2005; 30(3):389-94. [ Links ]
4. Anusavice K J. Phillip's Science of Dental Materials, 10. edition. W.B.: Saunders Co.; 1996. [ Links ]
5. Ersoy M, Civelek A, L'Hotelier E, Say EC, Soyman M. Physical properties of different composites. Dent. Mat. Journal 2004; 23(3):278-84. [ Links ]
6. Oertli D C B, Mandarino F, Guerreiro M C. Study of different polymerization systems for indirect aesthetic restorations. Rev Bras Odontol 2002; 59(1):61-4. [ Links ]
7. Galafassi D, Gonçalves LS , Spazzin AO, Carlini Jr. B. Influence analisys of three pos-polymerization methods in relation to flexural strenght of a clinical composite. Rev Dental Press Estet 2006; 3(3):37-42. [ Links ]
8. Kildal KK, Ruyter IE. How different curing methods affect mechanical properties of composites for inlays when tested in dry and wet conditions. Eur J Oral Sci 1997; 105(4): 353-61. [ Links ]
9. Peutzfeldt A, Asmussen E. Influence of carboxylic anhydrides on selected mechanical properties of heat-cured resin composites. J Dent Res 1991; 70(12):1537-41. [ Links ]
10. Peutzfeldt A, Asmussen E. The effect of postcuring on quantity of remaining double bonds, mechanical properties, and in vitro wear of two resin composites. J Dent 2000; 28(6):447-52. [ Links ]
11. Reinhardt JW, Boyer DB, Stephens NH. Effects of secondary curing on indirect posterior composite resins. Oper Dent 1994; 19(6): 217-20. [ Links ]
12. Wendt SL. The effect of heat used as secondary cure upon the physical properties of three composite resins. II. Wear, hardness, and color stability. Quintessence Int 1987; 18(5):351-6. [ Links ]
13. Santana IL, Lodovici E, Matos JR, Medeiros IS, Miyasaki C, Rodrigues-Filho LE. Effect of experimental heat treatment on mechanical properties of resin composites. Braz Dent J 2009; 20(3):205-10. [ Links ]
14. Technical Product Profile. Filtek™ P60 Posterior Restorative System. 3M Catalogue; 1998. [ Links ]
15. International Organization For Standardization (1988). Dentistry - Resin-Based Filling-Materials. ISO 4049:1988 (E). [ Links ]
16. Astm E-384. "Standard test method for microhardness of materials". American Society for Testing and Materials ASTM, Annual Book of Standards, v. 3; 1999. [ Links ]
17. Montenegro AC, Couto CF, Ventura PRR, Gouvea CVD, Machado AN. In vitro comparative analysis of resistance to compression of laboratory resin composites and ceramic system. Indian J Dent Res 2010; 21:68-71. [ Links ]
18. Faria ACL, Benassi UM, Rodrigues RCS, Ribeiro RF, Mattos MGC. Analysis of relationship between the surface hardness an wear resistance of indirect composites used as veneer materials. Braz Dent J 2007; 18(1):60-4. [ Links ]
19. Loza-Herrero MA, Rueggeberg FA, Caughman WF, Shuster GS, Lefebvre CA, Gardner FM. Effect of heating delay on conversion and strength of a post-cured resin composite. J Dent Res 1998; 77(2):426-31. [ Links ]
20. Borba M, Della Bona A, Cecchetti D. Flexural strength and hardness of direct and indirect composites. Braz Oral Res 2009; 23(1):5-10. [ Links ]
21. Adabo GL, Cruz CAS, Fonseca RG, Vaz LG. The volumetric fraction of inorganic particles and the flexural strength of composites for posterior teeth. J. Dent 2003; 31(5):353-9. [ Links ]
22. Loguercio AD, Poskus ARLT, Rodrigues Filho LE, Busato ALS, Bauer JRO. Evaluation of the mechanical properties of different composite resins. Rev Bras Odontol 2001; 58(6):382-5. [ Links ]
23. Satsukawa H, Hiroyasu K, Naomi T, Mika N, Tomohisa O, Hideo M. Properties of an indirect composite material polymerized with two different laboratory polymerinzing system. Dent Mater J 2005; 24(3):377-81. [ Links ]
24. Mandikos MN, McGivney GP, Davis E, Bush PJ, Carter JM. A comparison of the wear resistance and hardness of indirect composite resins. J Prosthet Dent 2001; 85(4):386-95. [ Links ]
25. Wendt SL, Leinfelder KF. The clinical evaluation of heat-treated composite resin inlays. J Am Dent Assoc 1990; 20(2):177-81. [ Links ]
 Correspondence to:
Correspondence to:
Luciano de Oliveira Martins Junior
Rua Dos Otoni, 428/402 - Santa Efigênia
30150-270 Belo Horizonte - MG
Fones: (31) 3241-1177
E-mail: lomjrodontologia@gmail.com
Recebido: 06.12.2009
Aceito: 14.07.2010













