Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RFO UPF
versão impressa ISSN 1413-4012
RFO UPF vol.16 no.2 Passo Fundo Mai./Ago. 2011
Stability of pharyngeal airway space after maxillomandibular advance surgery in patients with class II malocclusion
Estabilidade da dimensão do espaço aéreo faríngeo após o avanço maxilomandibular em pacientes com maloclusão de classe II
Marcia Angelica Peter Maahs*; Eduardo Silveira Ferreira**; Edela Puricelli***
* Specialist in Orthodontics and Facial Orthopedics – UFRGS, Doctor in Odontology (Focus Area in Clinical Stomatology) – PUCRS. Porto Alegre, RS, Brazil.
** Master's and Doctorate in Orthodontics – UFRJ, Adjunct Lecturer of Orthodontics – UFRGS, Lecturer in Course of Specialist in Orthodontics – UFRGS. Porto Alegre, RS, Brazil.
*** Doctor, University of Düsseldorf, Düsseldorf, Germany, Coordinator of Focus Area in Surgery and Buccomaxillofacial Traumatology: Master's and Doctorate Courses, Faculty of Odonthology – UFRGS, Chief of the Bucomaxillofacial Surgery Unit, Hospital da Clinicas of Porto Alegre, Faculty of Odontology – UFRGS. Porto Alegre, RS, Brazil.
Abstract
The lateral cephalometric radiographs show a high degree of visual resolution for the pharyngeal airway space, which is delimited by soft and hard tissues. Oromaxillofacial surgical treatment may be indicated for the patient with skeletal class II malocclusion, where whether or not mandibular advance is associated with interventions of the maxilla. Objective: The objective of this study was to determine the stability of the dimensional alterations of the total pharyngeal airway space (TPAS), distinguishing the airway space of the nasopharynx (NP), oropharynx (OP) and hypopharynx (HP), in cm2, after maxillomandibular advance. Methods: Cephalometric radiographs were taken in the preoperative (PRE), early postoperative (EPOST) and late postoperative (LPOST) periods of patients who submitted to combining surgeries. Based on proposals of cephalometric studies for this area, a statistical analysis was accomplished to determine the presence or absence of significant differences between PRE and EPOST, between EPOST and LPOST, and between PRE and LPOST. Results: There was an increase in values of the OP area and of TPAS in EPOST and decrease in LPOST. However, for these airway spaces, area values in LPOST differed from those in PRE, which were always much lower. Conclusions: These results may contribute to the treatment of obstructive sleep apnea and hypopnea, even if relapse occurs, where the pharyngeal airway space is still greater in LPOST than in PRE.
Key words: Sleep apnea. Orthognathic surgery. Relapse.
Resumo
As radiografias cefalométricas de perfil apresentam um alto grau de resolutibilidade visual para a via aérea faríngea, que é delimitada por tecidos moles e duros. O paciente portador de maloclusão esquelética de Classe II pode ter indicação de tratamento cirúrgico bucomaxilofacial, com avanço mandibular associado ou não a intervenções na maxila. Objetivo: O objetivo deste estudo é verificar a estabilidade das alterações dimensionais do espaço aéreo faríngeo total (EAFT), particularizando o espaço aéreo da nasofarige (NP), orofaringe (OF) e hipofaringe (HF), em cm2, após o avanço maxilomandibular. Metodologia: Foram utilizadas radiografias cefalométricas de perfil pré-operatórias (PRE), pós-operatórias mediatas (POSM) e pós-operatório tardias (POST) de pacientes que realizaram cirurgias combinadas. Baseado em propostas de estudos cefalométricos para essa área, realizou-se uma análise estatística para avaliação da presença ou não de diferenças significativas entre o PRE e o POSM, entre o POSM e POST e entre o PRE e o POST. Resultados: Houve aumento dos valores em área da OF e do EAFT no POSM e diminuição no POST. Porém, para esses espaços aéreos os valores em área no POST diferiram dos valores em área do PRE, sempre mais baixos. Conclusão: Esse resultado pode contribuir no tratamento das apneias e hipopneias obstrutivas do sono, mesmo que a recidiva ocorra, visto que a área do espaço aéreo faríngeo ainda permanece maior no POST do que no PRE.
Palavras-chave: Apneia do sono. Cirurgia ortognática. Recidiva.
Introduction
Cephalometric analysis may reveal dento-facial anomalies1, which its cost is low and it is easy to achieve, and the individual is exposed to minimal levels of radiation. Also, it is essential for the identification of the craniofacial bone soft tissue factors that may be involved in pharyngeal collapse in obstructive sleep apnea and hypopnea syndrome (OSAHS)2. Cephalometric studies have uncovered a tendency of the retrusive position of the maxilla and mandible in patients with OSAHS3.
Surgeries fulfilled in the maxillomandibular skeleton provide benefits for the correction of facial and occlusal deformities, resulting in a favorable influence on respiratory dysfunction characterized by OSAHS, by increasing the size of the pharyngeal airway4. This increase occurs by the counterclockwise rotation of the maxillomandibular complex in patients with a high occlusal plane5. Within this concept, the surgical technique of Puricelli6,7 still allows mandibular overcorrection in cases of severe obstructions of rapid progression avoiding a possible tracheotomy.
Postoperative changes in the width of the pharyngeal airway space, in the majority of studies is measured by reference lines in specific points in the antero-posterior direction8,9. A study of this pharyngeal area found an increase in the airway space of the nasopharynx after maxillary advance surgery, and increase in the airway space of the hypopharynx and nasopharynx after advancement and maxillary impaction, probably due to adaptation of the mandible and tongue which are able to assume a more anterior position11. A previous study that measured dimensional changes of total pharyngeal airway space, focusing on the airway space of the nasopharynx, oropharynx and hypopharynx in cm2 between pre- and postoperative periods of patients with class II skeletal malocclusion submitted to buccomaxillofacial surgical treatment by maxillomandibular advancement, demonstrated an increase in pharyngeal airway space, especially in the oropharynx and hypopharynx11. The increase in posterior airway space in cases of maxillomandibular advance may be related to counterclockwise rotation and the greater quantity of soft tissues in the involved airway space previously positioned12. The stability and predictability of movements in orthognathic surgery are frequent targets of study. The stability after bone repositioning, in order of importance, depends on the magnitude and direction of the movement13, type of fixation7 and surgical technique6,14. The rigid internal fixation provides greater comfort and assurance in the postoperative period. However, the stability of the repositioned segments is a challenge to even the most experienced surgeons, because the causes are multifactorial and involve various orthodontic and surgical factors15. Eggensperger et al.16 (2005), using cephalometric analysis, followed-up 15 patients who had maxillomandibular advancement, for a period of 12 years. Based on this study, it was believed that the suprahyoid muscles can contribute to skeletal relapse, where a diminution of the upper and middle pharyngeal airway spaces can also occur, because the position of the hyoid bone is more posterior in the postoperative that the preoperative period.
The stability and predictability of movements in orthognathic surgery are frequent targets of study. The stability after bone repositioning, in order of importance, depends on the magnitude and direction of the movement13, type of fixation7 and surgical technique6,14. The rigid internal fixation provides greater comfort and guarantee in the postoperative period. However, the ruler, al lowing the calibr stability of the repositioned segments is a challenge to even the most experienced surgeons, because the causes are multifactorial and involve various orthodontic and surgical factors15. Eggensperger et al.16 (2005), using cephalometric analysis, followed-up 15 patients who had maxillomandibular advance, for a period of 12 years. Based on this study, it was believed that the suprahyoid muscles may contribute to skeletal relapse, where a diminution of the upper and middle pharyngeal airway spaces may also occur, because the position of the hyoid bone is more posterior in the postoperative that the preoperative period.The aim of the present study was to evaluate, through the cephalometric radio-graphs, the postsurgical stability of the dimensional alterations in the pharyngeal airway space, after maxillomandibular advancement surgery in patients with class II skeletal malocclusion.
A long-term stability was found in maxillomandibular advance surgery, evaluated in cephalometric radiographs in the preoperative, early postoperative and late postoperative periods of 19 patients who were also submitted to a genioplasty in the treatment of OSAHS. In the late period, the patients who had large surgical advances, maintained the permeability of the airways as planned, and the relapse rate was only 10% in both the maxilla and mandible in the horizontal direction17. Similar results were obtained in the studies of Louis et al.18 (1993) in 20 patients and Riley19 (1993) in 26 patients, who had a relapse rate around 20% or less. A study by Tiner, in 1995, demonstrated less than 10% relapse of the maxilla as well as the mandible; however, there was a high standard deviation and some cases considered individually relapsed significantly20.
The aim of the present study was to evaluate, through the cephalometric radio-graphs, the postsurgical stability of the dimensional alterations in the pharyngeal airway space, after maxillomandibular advance surgery in patients with class II skeletal malocclusion.
Subjects and method
In order to evaluate the dimensional alteration in the pharyngeal airway, we selected cephalometric radiographs of 11 patients with class II skeletal malocclusion who were submitted to orthognathic maxillomandibular advance surgery by the same surgeon (E.P.). Puricelli's technique was used for mandibular osteotomy6,21,22.
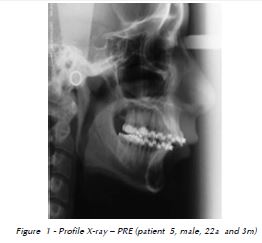
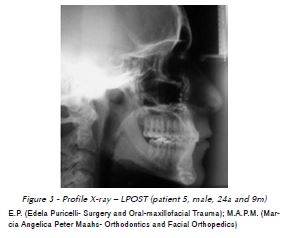
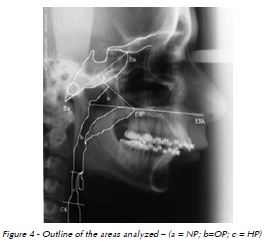
All patients had cephalometric radiographs in PRE (Fig. 1), EPOST (Fig. 2) and LPOST (Fig. 3), with variable time between them and performed in the same radiology center, when considering each patient individually. Manual cephalometric tracings were made over the hard and soft tissues landmarks by the same operator (M.A.P.M.). The images of cephalometric tracings were digitized with a millimeter ation of the measurements of the pharyngeal airway space, as in the prior study of Maahs et al.11 (2005). The measurements of the areas of the nasopharynx (NP), oropharynx (OP), hypopharynx (HP) and total pharyngeal airway space (TPAS) were obtained by using program Image Tool 3.0, tracing the outline of each of these areas, measured in cm2 in PRE, EPOST and LPOST to evaluate the dimensional alterations. After tracing the contours of each area and recording the dimensional alterations, the differences in areas were determined between PRE and EPOST, between EPOST and LPOST and between PRE and LPOST. The determination of the limits of the areas of the airway spaces was based on the cephalometric parameters of Ono et al.23 (1996) (Fig. 4 and 5), as previously published by Maahs et al.11 (2005).


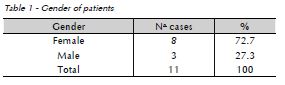
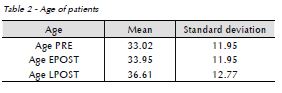
From these individuals, 8 (72.7%) were females and 3 (27.3%) males (Table 1) aging from 33.02 + 11.95 years old in PRE, 33.95 + 11.95 years old in EPOST and 36.61 +12.77 years old in LPOST. In EPOST in relation to PRE, there was an average increase in age of 1 year, in LPOST in relation to PRE, there was an average increase in age of 3.6 years, and in LPOST in relation to EPOST, there was an average increase in age of 2.7 years (Table 2).
Results
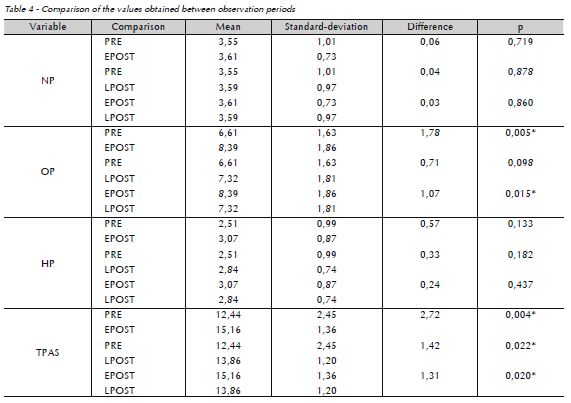
Statistical analysis (Student's t test of comparison of paired samples) of the results revealed significant differences (p < 0.05) between the PRE and EPOST periods, with higher values for the EPOST study of the measurements in area (cm2) of the dimensions of OP and TPAS, and between the EPOST and LPOST periods with lower values for the study of OP and TPAS. Between the PRE and LPOST periods, there was a significant difference in TPAS only, which showed higher values for LPOST study. Thus, TPAS values increased in EPOST and decreased in LPOST, but still differed from the lower PRE values (Table 4).
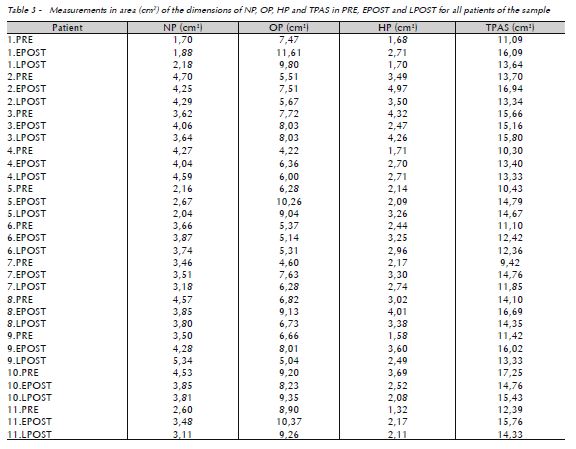
The area of the TPAS of the sample studied was increased in EPOST in nine of the eleven patients (Table 3). Mean TPAS increased from 12.44 cm2 in PRE to 15.16 cm2 in EPOST, and to 13.86 cm2 in LPOST (Table 4, Fig. 6).
The following results were obtained when evaluating each region of the pharynx individually:
In NP, seven patients showed an increase in airway space and four showed a decrease in EPOST. In LPOST, seven patients showed a decrease in relation to EPOST, but in relation to PRE, six patients had an increase in this space (Table 3). Mean NP values for the sample were 3.55 cm2 in PRE, 3.61 cm2 in EPOST, and 3.59 cm2 in LPOST (Table 4, Fig. 6).
For OP, two patients showed a decrease of this space in EPOST, while the other showed an increase. In LPOST, eight patients showed a decrease, two an increase and one remained the same in relation to EPOST. However, in relation to PRE, nine patients had an increase and two a decrease (Table 3). Mean OP area values varied from 6.61 cm2 in PRE to 8.39 cm2 in EPOST and to 7.32 cm2 in LPOST (Table 4, Fig. 6).
For HP, three patients showed a reduction of the airway space in EPOST, while the others showed an increase. In LPOST, eight patients had a decrease in relation to EPOST, and nine patients showed an increase in relation to PRE (Table 3). Mean HP for the sample varied from 2.51 cm2 in PRE to 3.07 cm2 in EPOST and to 2.84 in LPOST (Table 4, Fig. 6).
The mean increase in TPAS in EPOST was 2.72 cm2, mainly due to the mean increase in OP airway space of 1.78 cm2, greater than the one for the NP airway space (0.06 cm2) and the HP airway space (0.57 cm2). The mean decrease in TPAS in LPOST in relation to EPOST was 1.31 cm2, mainly due to the mean decrease in airway space of OP of 1.07 cm2, because for NP, it was 0.03 cm2 and HP 0.24 cm2. The mean increase in TPAS in LPOST in relation to PRE was 1.42 cm2, mainly due to the mean increase in airway space of OP of 0.71 cm2, because for NP it was 0.04 cm2 and HP 0.33 cm2. However, this last increase in OP was not statistically significant.

Discussion
Cephalometric analysis has been utilized by many authors to quantify specific parameters of the airways3. The possibility to analyze the pharyngeal airway three-dimensionally by cone beam computed tomography is substantially current24. The present study was retrospective in nature; archive radiographs were used in which the difference was to use a two-dimensional evaluation, measuring the pharyngeal airway space in cm2 in the pre and postoperative periods in patients with class II skeletal malocclusion11. In this study, the spaces were measured not only in preoperative and early postoperative periods, but also in the late postoperative period, in order to determine the stability of the dimension of the pharyngeal airway space after maxillomandibular advance in patients with class II malocclusion. Although a two-dimensional study it differed from that not only cephalometric reference points and lines were used, as by the majority of published studies8,9, thus including multiple points of the airway space. In addition, the pharynx was divided into 3 airway spaces to measure the areas of NP, OP and HP, besides that of TPAS. In this manner, it was possible to determine that the results were significant at the OP level, which was the most important in the alterations in TPAS, both between PRE and EPOST and EPOST and LPOST. Between PRE and LPOST, only TPAS showed a significant difference, with higher values in LPOST. The results showed that, although there was some relapse in size of TPAS, it remained increased in relation to the beginning of the treatment.
A study by Márquez et al.2 (2005) found that the upper posterior airway space of the pharynx is less in patients with OSAHS, This space would correspond to the upper limit of the oropharynx of this study. This suggests that the results obtained in this study would contribute to the treatment of OSAHS, due to the increase in this space in EPOST and LPOST in relation to PRE. Gonçalves et al.25 in (2006) found that maxillomandibular advance produces an immediate increase in airway space in the middle and lower regions of the oropharynx, which remains stable in the postoperative periods where there is a long-term increase in the upper region after surgery, due to the regression of the postsurgical edema that occurs at this location.
Maxillomandibular advance surgery provides benefits to patients with facial and occlusal deformities, eliminating or diminishing the symptoms of OSAHS, due to its effect in increasing the dimensions of the pharyngeal airway5. Thus, our results are similar to those studies that reported an increase of these dimensions in the postoperative period19,26,27. On the contrary, there are studies that evaluated the effects of mandibular setback surgery on the pharyngeal airway, and decreased in size28,29,30. Before the surgical advance of the mandible, the aspects related with OSAHS should be investigated to determine the degree of advance that could be of respiratory benefit. In the present study, maxillomandibular advance surgery accomplished in patients with class II malocclusion, increased the dimensions of TPAS in the postoperative period, suggesting benefits to the patients with this radiographic space previously diminished. The possible increase in the lateral dimension of the airway after maxillomandibular advance31 was not evaluated in this study.
The results of this study demonstrate benefits for the widening of the pharyngeal airway space. However, there was no significant sagittal increase in the NP and HP areas in the postoperative period, because the increase was significant for TPAS, mainly due to the increase in the OP area. The results are similar to those of De Ponte et al8. (1999) who reported an increase in the lower part of the oropharynx, after impaction of the maxilla in patients with class II malocclusion. However, their measurements were not in specified areas. The present results are also in line with those of Pereira Filho who showed an increase in pharyngeal airway space in the majority of the measurements analyzed, but there were linear measurements12. In this study, 2 patients did not show an increase in the dimensions of TPAS in EPOST, which could be related to the fact that this study was carried out in patients who underwent the surgical procedure for the purpose of treating class II skeletal malocclusion and not for treatment of OSAHS, which is aimed at increasing the dimensions of the pharyngeal airway. We believe that if this study were done in patients treated with maxillomandibular advance, improving the pharyngeal airway in the treatment of OSAHS, the results would be more significant, because surgical advances would probably be of greater proportions.
Although the majority of studies have analyzed skeletal stability in the postoperative period17,19, there are studies examining the stability of the dimensions of the pharyngeal airway space after maxillomandibular advance. We believe that the suprahyoid muscles may contribute to skeletal relapse, leading to diminution of upper and lower pharyngeal airway spaces in the postoperative period16. During the surgical procedure, this musculature (ventral anterior of the digastric and suprahyoid) can be stretched to diminish its forces, thereby reducing the tendency of relapse in mandibular advancements32. In the present study, LPOST values of TPAS decreased, but still differed from the lower PRE values. This indicates that there was relapse in LPOST, but the dimensions of TPAS were still greater than in PRE. Although the values were greater in LPOST in relation to PRE in each specified area (NP, OP and HP), they were not statistically significant, but certainly contributed to the significant results obtained for TPAS.
Conclusions
• Patients with class II skeletal malocclusion, submitted to oral maxillofacial surgical treatment by maxillomandibular advance, showed an increase in pharyngeal airway space, especially in the oropharynx.
• Patients with class II skeletal malocclusion, submitted to oral maxillofacial surgical treatment by maxillomandibular advance, showed a decrease in total pharyngeal airway space in late postoperative, indicating relapse postorthosurgical treatment, but still maintaining this space increased compared to the beginning of the treatment.
• This method of cepholometric evaluation may contribute to analyze the results of preoperative and postoperative in patients with obstructive sleep apnea and hypopnea.
References
1. Pereira CB, Mundstock CA, Berthold TB. Histórico. In: Pereira CB, Mundstock CA, Berthold TB. Introdução a cefalometria radiográfica. Porto Alegre: Pancast; 1989. p. 23-30. [ Links ]
2. Márquez CG, Maniglia JV. Estudo cefalométrico de indivíduos com síndrome da apnéia obstrutiva do sono: revisão da literatura. Arq Cien Saúde 2005; 12(4):206-12.
3. Lowe AA, Santamaría JD, Fleetham JA. Facial morphology and obstructive sleep apnea. Am J Orthod Dentofacial Orthop 1986; 90(6):484-91.
4. Won CHJ, Li KK, Guilleminaut C. Surgical treatment of obstructive sleep apnea: upper airway and maxillomandibular surgery. Proc Am Thorac Soc 2008; 5(2):193-9.
5. Mehra P, Downic M, Pita MC, Wolford LM. Airway space changes after counterclockwise rotation of the maxillomandibular complex. Am J Orthod Dentofacial Orthop 2001; 120(2):154-9.
6. Puricelli E. A new technique for mandibular osteotomy. Head Face Med 2007; 3:15.
7. Puricelli E. Menor tempo de fixação intermaxilar nas cirurgias de prognatismo. Rev Gaúcha Odontol 1982; 30:95-8.
8. De Ponte FS, Brunelli A, Marchetti E, Bottini DJ. Cephalometric study of posterior airway space in patients affected by class II occlusion and treated with orthognathic surgery. J Craniofac Surg 1999; 10(3):252-9.
9. Li KK, Guilleminaut CRR, Powell NB. Obstructive sleep apnea and maxillomandibular advancement: an assessment of airway changes using radiographic and nasopharyngoscopic examinations. J Oral Maxillofac Surg 2002; 60(5):526-30.
10. Greco JM, Frohberg U, Van Sickeels JE. Cephalometric analysis of long-term airway space changes with maxillary osteotomies. Oral Surg Oral Med Oral Pathol 1990;70(5):552-4.
11. Maahs MAP, Puricelli E, Maahs GS, Mundstock CA, Ferreira EJB. As modificações da dimensão do espaço aéreo faríngeo decorrentes do avanço maxilo-mandibular em pacientes com maloclusão de classe II. Rev Ortodont Gaúcha 2005; 9(1):13-22.
12. Pereira Filho VA, Jeremias F, Tedeschi I, Souza RF. Avaliação cefalométrica do espaço aéreo posterior em pacientes com oclusão classe II submetidos a cirurgia ortognática, Rev Dental Press Ortodont Ortoped Facial. 2007 Set/ Out;12(5):119-25.
13. Puricelli E, Fonseca JS, De Paris MF, Sant'Anna H. Applied mecanics of the Puricelli osteotomya linear elastic analysis with the finite element method. Head Face Med 2007; 3:38.
14. Proffit WR, Turvey TA, Phillips C. Orthognatic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg 1996; 11(3):191-204.
15. Araújo AM, Araújo A, Araújo MM, Gabrielli MFR, Sakima T. Estabilidade de avanços mandibulares em cirurgias ortognáticas combinadas com a utilização de fixação interna rígida. Ortodontia; 33(2):65-75.
16. Eggensperger N, Smolka K, Johner A, Rahal A, Thüer U, Iizuka T. Long-term changes of hyoid boné and pharyngeal airway size following advancement of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99(4):404-10.
17. Nimkam Y, Miles PJ, Waite PD. Maxillomandibular advancement surgery in obstructive sleep apnea syndrome patients: long-term surgical stability. J Oral Maxillofac Surg. 1995; 53(12):1414-8.
18. Louis PJ, Waite PD, Austin RB. Long-term esqueletal stability after rigid fixation of Le Fort I osteotomies with advancements. Int J Oral Maxillofac Surg 1993; 22(2):82-6.
19. Riley RW, Powell NB, Guilleminaut C. Obstructive sleep apnea syndrome: a surgical protocol for dynamic airway reconstruction. J Oral Maxillofac Surg 1993; 51(7):742-7.
20. Tiner BD. Maxillomandibular advancement surgery in obstructive sleep apnea syndrome patients: long-term surgical stability. J Oral Maxillofac Surg 1995; 53(12):1418-9.
21. Puricelli E. Tratamento cirúrgico da ATM: casos selecionados. In: Feller C, Gorab R. Atualização na clínica odontológica. São Paulo: Apcd; 2000. Vol 2, p. 479-520.
22. Puricelli E. A multidisciplinaridade da cirurgia e traumatologia na odontologia. In: Vanzillotta OS, Gonçalves AR. Odontologia integrada. Atualização multidisciplinar para o clínico e o especialista. Rio de Janeiro: Pedro Primeiro; 2001. p. 59-94.
23. Ono T, Lowe AA, Fergunson KA, Fleetham JA. Associations among upper airway structure, body position, and obesity in skeletal class I male patients with obstructive sleep apnea. Am J Orthod Dentof Orthop 1996; 109(6):625-34.
24. Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-bean computed tomography. Am J Orthod Dentofacial Orthop 2009; 135(4):468-79.
25. Gonçalves JR, Buschang PH, Gonçalves DG, Wolford LM. Postsirurgical stability of oropharingeal airway changes following counter-clockwise maxillo-mandibular advancement surgery. J Oral Maxillofac Surg 2006; 64(5):755-62.
26. Riley RW, Powell NB, Guilleminaut C, Ware W. Sleep apnea syndrome following surgery for mandibular prognatism. J Oral Maxillofac Surg 1987; 45(5):450-2.
27. Solow B, Siersbaek-Nielsen S, Greve E. Airway adequacy, head posture, and craniofacial morphology. Am J Orthod 1984; 86(3):214-32.
28. Graber IW. Hyoid changes following orthopedic treatment of mandibular prognathism. Angle Orthod 1978; 48(1):33-8.
29. Hochban W, Schürmann R, Brandenburg U, Conradt R. Mandibular setback for surgical correction of mandibular hyperplasia- does it provoke sleep-related breathing disorders! Int J Oral Maxillofac Surg. 1986; 25(5):333-8.
30. Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg 2000; 58(3):282-5.
31. Lye KW. Effect of orthognatic surgery on the posterior airway space (PAS). Ann Acad Med Singapore. 2008; 37(8):677- 82.
32. Arnett GW. A redefinition of bilateral sagital osteotomy (BSO) advancement relapse. Am J Orthod Dentofacial Orthop 1993; 104(5):506-15.
33. Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop 1996; 110(1):8-15.
 Endereço para correspondência:
Endereço para correspondência:
Marcia Angelica Peter Maahs
6690, Ipiranga Ave. # 511, Jardim Botânico
90610000 Porto Alegre - RS
e-mail: maahs.orto@gmail.com
Recebido: 05.05.2011
Aceito: 14.07.2011













