Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RFO UPF
versão impressa ISSN 1413-4012
RFO UPF vol.16 no.3 Passo Fundo Set./Dez. 2011
Direct composite veneer to treat primary teeth with sequela of dental trauma: a case report
Faceta direta de resina composta para tratamento de dente decíduo com sequela de traumatismo dentário: relato de caso
Marília Leão Goettems*; Marina Sousa Azevedo*; Dione Dias Torriani**; Ana Regina Romano***; Rudimar Baldissera****; Flávio Fernando Demarco*****
* DDS, Graduate Student in Pediatric Dentistry, Department of Social and Preventive Dentistry, School of Dentistry, Federal University of Pelotas, RS, Brazil.
** DDS, MS, PhD, Associate Professor, Infant Clinic, Department of Social and Preventive Dentistry, School of Dentistry, Federal University of Pelotas, RS, Brazil.
*** DDS, MS, PhD, Associate Professor, Department of Social and Preventive Dentistry, School of Dentistry, Federal University of Pelotas, RS, Brazil.
**** Professor Livre Docente da Faculdade de Odontologia - São Leopoldo Mandic, SP.
***** DDS, MS, PhD, Associate Professor, Department of Operative Dentistry, School of Dentistry, Federal University of Pelotas, RS, Brazil.
Abstract
Introduction: Tooth discoloration can be one of the main reasons for parents to seek treatment after dental trauma. When this sequela occurs with no other clinical or radiographic symptoms, a conservative approach is recommended. However, when such alterations can compromise the patient's esthetics and his/her interaction in a social environment, an esthetic treatment may be required. Case report: Here we report the esthetic rehabilitation of a primary maxillary left central incisor presenting coronal darkening in a 5-year-old girl that had been monitored clinically and radiographically due to dental trauma in the maxillary anterior teeth since she was 1 year old. Because of the esthetic complaint, a direct composite resin veneer was performed. Final considerations: After the treatment, a good esthetic result was achieved making the patient and her parents pleased. The esthetic improvement was maintained at the six-month follow-up with no negative impact on the child's social life.
Key words: Operative dentistry. Primary dentition. Wounds and injuries. Dental esthetics.
Resumo
Introdução: A mudança de cor da coroa dentária resultante de um traumatismo pode ser uma das principais razões para os pais procurarem tratamento odontológico. Quando esta sequela ocorre sem nenhum outro sintoma clínico e radiográfico, uma abordagem conservadora é recomendada. Entretanto, quando essas alterações comprometem a estética do paciente e sua interação no meio social, um tratamento estético pode ser necessário. Relato de caso: Neste artigo, é relatada a reabilitação estética de um incisivo central superior esquerdo decíduo que apresentava escurecimento coronário em uma menina de cinco anos de idade, que estava sendo monitorada em razão de um traumatismo dentário nos dentes superiores anteriores desde que tinha um ano de idade. Em virtude da queixa, uma faceta direta de resina composta foi realizada. Considerações finais: Após o tratamento, um bom resultado estético foi conseguido, satisfazendo à paciente e aos seus pais. No retorno de seis meses, a melhora estética foi mantida e não houve nenhum impacto negativo na vida social da criança.
Palavras-chave: Dentística operatória. Dentição decídua. Traumatismos. Estética dentária.
Introduction
Traumatic dental injuries are common in primary dentition, with the maxillary central incisors being the most frequently affected because of their position1. Studies have found prevalence estimates varying from 10%2 to 36%3.
Dental trauma might generate various sequelae, including pulp necrosis, fracture lines, ankylosis, early loss, dental mobility, bone and root resorption, dental discoloration, and pulp chamber obliteration4,5. Although frequent, not all sequelae can be immediately identified and require longterm follow-up.
Crown discoloration, considered by some authors as the second most common sequela6, is one of the main reasons that parents seek treatment after dental trauma1. Around 53% of the traumatized teeth present color change4. Nowadays, when there is no other associated symptom, the conservative approach is the ideal treatment for it, which requires waiting and carefully watching the case6,7. However, when anterior teeth are involved, it is essential to satisfy basic esthetic requirements, including the tooth shade, which play a fundamental role in the children's social life.
Various treatment options are available to treat discolored teeth, including dental bleaching, direct composite, and indirect ceramic veneers8,9. Although bleaching may be the most conservative treatment with a good esthetic outcome, it should be avoided in children under 15 years of age10. Indirect veneers provide excellent esthetic results, but the procedure removes sound tissue and requires laboratory procedures11. Direct composite restorations have gained popularity because of the good results they present, with good functional and esthetics outcomes and the preservation of tooth structure12. Dental adhesives today present strong and stable bonding characteristics. The mechanical, optical, and physical properties of the composite resins allow them to recover the esthetics and function of natural teeth13. This case report presents the esthetic rehabilitation of a darkened traumatized central incisor of a 5-year-old girl using the direct composite veneer technique.
Case Report
Description of the case
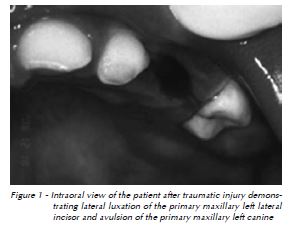
In December 2005, a girl one year and 11 months old was taken by her parents to the Center for the Study and Treatment of Dental Trauma in Deciduous Teeth at the Pelotas Federal University – School of Dentistry, RS, Brazil. The patient presented lateral luxation of the primary maxillary left lateral incisor and avulsion of the primary maxillary left canine, both caused by collision against a hard object (Fig. 1). The lip presented laceration of the soft tissue and had been sutured two days before in the emergency room where the patient had received care first. The parents reported that the girl had a previous trauma that resulted in enamel-dentin fracture without pulpal exposure of the primary maxillary left central incisor. The patient was in good general health.
The treatment followed a standard protocol: a specific trauma record file was filled in, including anamnesis; clinical and radiographic examinations of the affected area; and photographic documentation of the injuries. The treatment decision for the case was a long-term clinical and radiographic follow-up until the eruption of the permanent teeth, as permanent dentition may suffer adverse consequences as a result of such traumas14. In accordance with the International Association of Dental Trauma Guidelines, the avulsed tooth was not replanted14.
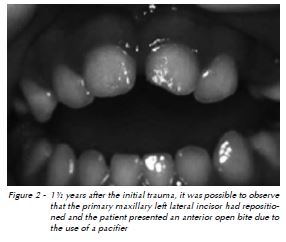
Periodic follow-ups (every six months) showed that the lip presented good healing and that the teeth were clinically and radiographically asymptomatic. The primary maxillary left lateral incisor repositioned itself, although the patient had an anterior open bite due to the use of a pacifier (Fig. 2).
In March 2008, when the patient returned for follow-up care, the parents reported that the patient had suffered another accident in February, which caused enamel fracture in the primary maxillary left central and lateral incisors. Although the central incisor showed color change, it was diagnosed as vital and exhibited no mobility. The professional explained to the parents that such an alteration would not cause damage to the maintenance of the tooth or sequelae to the permanent successor.
However, in the next examination, performed in October 2008, when the girl was at the age of four, the parents and the girl complained about the darkening of the primary maxillary left central incisor. Figure 3 shows the extent of the discoloration. The parents reported that she had changed her behavior, avoiding smiling at home and becoming shy at the daycare center she attended. There was no clear evidence of infection (Fig. 4). Considering the potential psychosocial effects over her quality of life, a restorative treatment was required. The professional team decided to perform a direct composite veneer.


Technique
Following prophylaxis, the composite shade was selected using a value-oriented shade guide (Vitapan Classical, Vita Zahnfabrik, Bad Sackingen, Germany). No local anesthesic was administered.
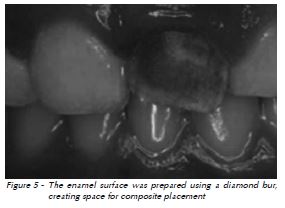
Initially the buccal enamel was reduced (approximately 1 mm thickness) using a fine granulated diamond bur (KG Sorensen, Barueri, SP, Brazil) at high speed under air-water cooling (Fig. 5).
To avoid saliva contamination, cotton rolls were used to keep the field dry. The prepared enamel was etched with 37% phosphoric acid gel (Villevie, Dentalville, Joinville, SC, Brazil) for 30 s, and then the tooth was completely rinsed and dried. The adhesive system (Adper Single Bond, 3M ESPE, St. Paul MN, USA) was applied according to the manufacturer's instructions.
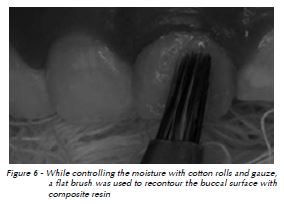
The restoration was performed using an incremental technique. A thin layer of a flow opaque composite (Opak, Angelus, Londrina, PR, Brazil) was applied to mask the darkening and then polymerized with an LED light-curing unit (Radii, SDI, Bayswater, Austrália) for 30s. A second composite layer was added to replace the dentin (Concept B2, Vigodent, Rio de Janeiro, RJ, Brazil), and a third layer of a more translucent composite was added (Filtek Z250TM B2, 3M ESPE, St. Paul MN, USA). A flat brush was used to recontour the buccal surface (Fig. 6).
Finishing and polishing procedures were performed immediately since there was no evidence of significant adverse effects15. Finishing was initiated using a fine granulated diamond bur (KG Sorensen, Barueri, SP, Brazil). Then, a #12 scalpel blade was employed to shape the cervical area. Polishing was performed using flexible discs (Sof-Lex TM; 3M ESPE, St. Paul MN, USA) and silicone points (Enhance®, Petrópolis, RJ, Dentsply, Brazil) with abrasive paste.
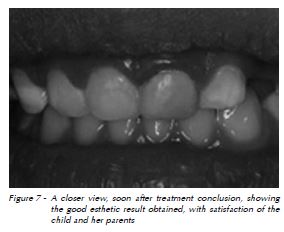
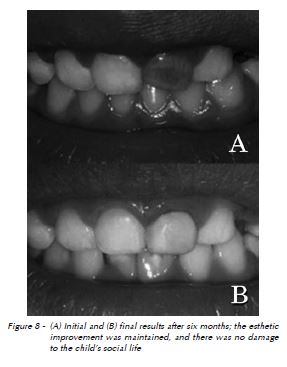
A good esthetic result was obtained, and it was well-accepted by the parents and the child (Fig. 7). After 6 months, the esthetic of the restoration was still good, and the parents reported that their daughter had a normal social life with the family and at the daycare center. A comparison between the discolored tooth and its appearance six months after its restoration can be seen in Figure 8.
Discussion
Dark coronal discoloration following trauma is a well-known phenomenon in primary maxillary incisors. This alteration should not be used as the only criteria for interceptive pulpal therapy16,17. Traumatized, dark discolored primary incisors can remain asymptomatic until their natural exfoliation, with discoloration being the only evidence that the teeth had suffered an injury7,18. The tooth should receive root canal treatment only if, in addition to discoloration, any of the following alterations are diagnosed: internal root resorption, inflammatory or replacement root resorption, periapical inflammation, or the presence of fistula6.
Alterations in the color of the teeth can compromise patients' esthetics and their interaction in a social environment. For primary dentition, some alternatives are available to treat discolored teeth that should be taken into consideration. For devitalized primary teeth, the use of a bleaching agent with 35% hydrogen peroxide has been reported19,20. However, there is limited evidence of the safety or efficacy of vital tooth bleaching in children21, and this procedure is not indicated for children younger than 15 years of old10.
When a restorative option is selected, several variables that should be considered, such as operator preferences, esthetic demands by parents, the child's behavior, and moisture and hemorrhage control22. In the case reported here, tooth vitality was preserved and the use of a direct resin composite veneer was chosen. This is an excellent technique to treat tooth discoloration, as it is relatively simple, presents low costs, and shows immediate satisfactory results.
A total etch technique was used based on previous evidence of the high bond strength values obtained with this technique23. The composites used in this case have good mechanical properties and produce a highly polished surface that is more resistant to wear and, consequently, lasts longer15. Clinical evaluations have demonstrated that direct composite veneers have long-lasting good esthetic results, and they have exhibited similar results to other indirect restorative approaches11 that are more expensive and require the removal of more sound tissue.
Dental trauma is common among children and could be considered one of the most dilacerating and stressful injuries in dentistry24. In this particular case, the main complaint was the darkening of the tooth, and, after the treatment conclusion, the esthetic expectations of the patient and her parents were completely fulfilled.
To conclude the case reported here demonstrates that direct composite veneers could be a good option to treat discolored traumatized primary incisors, as it presents predictable esthetic results that can minimize the potential psychosocial impact caused by this problem.
References
1. Garcia-Godoy F, Morban-Laucer F, Corominas LR, Franjul RA, Noyola M. Traumatic dental injuries in preschoolchildren from Santo Domingo. Community Dent Oral Epidemiol 1983; 11(2):127-30. [ Links ]
2. Nogueira AJS, Melo CB, Faria PJV, Nogueira RGM, Sampaio AMS. Prevalência de traumatismos dos dentes decíduos em crianças da faixa etária de 0 a 5 anos. J Bras Odontopediatr Odontol Bebê 2004; 7:266-71.
3. Wendt FP, Torriani DD, Assuncao MC, et al. Traumatic dental injuries in primary dentition: epidemiological study among preschool children in South Brazil. Dent Traumatol 2010; 26(2):168-73.
4. Borum MK, Andreasen JO. Sequelae of trauma to primary maxillary incisors. I. Complications in the primary dentition. Endod Dent Traumatol 1998; 14(1):31-44.
5. Cunha RF, Pugliesi DM, Percinoto C. Treatment of traumatized primary teeth: a conservative approach. Dent Traumatol 2007; 23(6):360-3.
6. Cardoso M, Rocha MJ. Federal University of Santa Catarina follow-up management routine for traumatized primary teeth - part 1. Dent Traumatol 2004; 20(6):307-13.
7. Holan G. Long-term effect of different treatment modalities for traumatized primary incisors presenting dark coronal discoloration with no other signs of injury. Dent Traumatol 2006; 22(1):14-7.
8. Meireles SS, Heckmann SS, Santos IS, Della Bona A, Demarco FF. A double blind randomized clinical trial of athome tooth bleaching using two carbamide peroxide concentrations: 6-month follow-up. J Dent 2008; 36(11):878-84.
9. Nixon PJ, Robinson S, Gahan M, Chan MF. Conservative aesthetic techniques for discoloured teeth: 2. Microabrasion and composite. Dent Update 2007; 34(3):160-162, 164, 166.
10. AssociationDentaireFrançaise. Medical Devices Commission: Tooth Bleaching Treatments – A Review. 2007; Accessed november 7, 2008.
11. Wakiaga J, Brunton P, Silikas N, Glenny AM. Direct versus indirect veneer restorations for intrinsic dental stains. Cochrane Database Syst Rev. 2004(1):CD004347.
12. Hickel R, Heidemann D, Staehle HJ, et al. Direct composite restorations: extended use in anterior and posterior situations. Clin Oral Investig 2004; 8(2):43-4.
13. Johnson WW. Use of laminate veneers in pediatric dentistry: present status and future developments. Pediatr Dent 1982; 4(1):32-7.
14. Flores MT, Malmgren B, Andersson L, et al. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dent Traumatol 2007; 23(4):196-202.
15. Cenci MS, Venturini D, Pereira-Cenci T, Piva E, Demarco FF. The effect of polishing techniques and time on the surface characteristics and sealing ability of resin composite restorations after one-year storage. Oper Dent 2008; 33(2):169-76.
16. Andreasen JO, Andreasen FM. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 3rd ed ed. Copenhagen: Munksgaard; 1994.
17. Flores MT. Traumatic injuries in the primary dentition. Dent Traumatol 2002; 18(6):287-98.
18. Holan G, Fuks AB. The diagnostic value of coronal darkgray discoloration in primary teeth following traumatic injuries. Pediatr Dent 1996; 18(3):224-7.
19. Bussadori SK, Roth F, Guedes CC, Fernandes KP, Domingues MM, Wanderley MT. Bleaching non vital primary teeth: case report. J Clin Pediatr Dent 2006; 30(3):179-82.
20. Gontijo IT, Navarro RS, Ciamponi AL, Zezell DM. Whitening techniques using the diode laser and halogen lamp in human devitalized primary teeth. J Dent Child (Chic) 2008; 75(2):164-7.
21. Donly KJ, Donly AS, Baharloo L, et al. Tooth whitening in children. Compend Contin Educ Dent 2002; 23(1A):22-8.
22. Waggoner WF. Restoring primary anterior teeth. Pediatr Dent 2002; 24(5):511-6.
23. De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005; 84(2):118-32.
24. Torriani DD, Bonow ML, Fleischmann MD, Muller LT. Traumatic intrusion of primary tooth: follow up until eruption of permanent successor tooth. Dent Traumatol 2008; 24(2):235-8.
 Endereço para correspondência:
Endereço para correspondência:
Dione Dias Torriani
Rua Gonçalves Chaves, 457, Centro
96015560 Pelotas/RS, Brazil
e-mail: dionedt@gmail.com
Recebido: 31.03.2011
Aceito: 23.08.2011













