Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RFO UPF
versão impressa ISSN 1413-4012
RFO UPF vol.17 no.3 Passo Fundo Set./Dez. 2012
Cementation of ceramics and indirect composite resin to enamel and dentin using different resin-based cements – Shear bond strength
Cimentação de cerâmica e resina composta indireta ao esmalte à dentina usando diferentes cimentos resinosos - resistência ao cisalhamento
Eurípedes Kaizo Ariki I; Carlos Augusto Pavanelli II; Alvin Tomm III; Lucas Villaça Zogheib IV
I MSc, Department of Dental Materials and Prosthodonti cs, Sao Jose dos Campos Dental School, São Paulo State University, São José dos Campos, SP, Brazil.
II DDS, MSc, PhD. Associate Professor of Removable Prosthodonti cs, São José dos Campos Dental School, São Paulo State University, São José dos Campos, SP, Brazil.
III DDS, University of Passo Fundo Dental School, Passo Fundo, RS, Brazil.
IV DDS, MSc, PhD. Professor of Prosthodonti cs and Multi disciplinary Clinics, Sacred Heart University, Dental School, Bauru, SP, Brazil.
ABSTRACT
Objective: To evaluate the shear bond strength of three different resin cements: self-etching (P), etch-and-rinse (R) and self-adhesive (U), to enamel and dentin using two types of restorative materials. Methods: One hundred twenty bovine incisors had the buccal surface ground to obtain a flat and smooth surface of approximately 25 mm2 . Half of the specimens had the enamel exposed (E), and the other half had the dentin exposed (D). An adhesive tape with a 3 mm-diameter orifice delimited the bonding area. Sixty 3 x 3 mm lithium disilicate glassceramic cylinders (C) and 60 indirect composite resin cylinders (R) were cemented to enamel or dentin using three types of resin cements, resulting in 12 experimental groups represented by symbols allusive to treatment protocols: PEC; PER; PDC; PDR; REC; RER; RDC; RDR; UEC; UER; UDC; and UDR. Shear bond strength test was performed with a crosshead speed of 0.5 mm/min. The data were subjected to ANOVA and Tukey's test with a significance level of 5%. Results (MPa ± DP): the highest mean value obtained, REC group (17.46 ± 3.29), differed significantly from others, except for the PEC group (14.60 ± 5.88). Among the groups with lower mean values, there was a predominance of those where the indirect resin was used regardless the substrate and type of resin cement, and the UDR group (1.03 ± 1.03) was statistically different from the others. Conclusion: In this study, all three experimental variables tested influenced the shear bond strength of tooth-cement-restoration interfaces.
Keywords: Dental cements. Ceramics. Composite resins. Shear strength. Dental materials.
RESUMO
Objetivo: Avaliar a resistência de união ao cisalhamento de três diferentes tipos de agentes cimentantes – autocondicionante (P), convencional (R) e autoadesivo (U) – ao esmalte e dentina usando dois tipos de materiais restauradores. Métodos: Cento e vinte incisivos bovinos tiveram a face vestibular desgastada até se obter uma superfície lisa e plana de aproximadamente 25 mm2. Metade dos espécimes tiveram o esmalte (E) exposto e, na outra metade, a dentina (D). Uma fita adesiva com orifício de 3 mm de diâmetro delimitou a área a ser testada. Sessenta cilindros (3 mm X 3 mm) de cerâmica à base de dissilicato de lítio (C) e sessenta cilindros de resina composta indireta (R) foram cimentados ao esmalte ou dentina utilizando três tipos de cimento resinosos, formando 12 grupos experimentais representados por abreviaturas alusivas aos protocolos de tratamento: PEC; PER; PDC; PDR; REC, RER; RDC; RDR: UEC; UER; UDC e UDR. Realizou-se o teste de cisalhamento com velocidade de 0,5 mm/min. Os dados foram submetidos à Anova e teste de Tukey com um nível de significância de 5%. Resultados (MPa ± DP): o maior valor médio obtido, grupo REC, (17,46 ± 3,29) diferiu significativamente dos demais, exceto do grupo PEC (14,60 ± 5,88). Dentre os grupos com menores valores médios, observou-se predominância daqueles nos quais a resina indireta foi utilizada, independentemente do substrato e do cimento resinoso, sendo o grupo UDR (1,03 ± 1,03) estatisticamente diferente dos demais. Conclusão: Neste estudo, as três variáveis testadas influenciaram a resistência adesiva entre as interfaces restauração-cimento-dente.
Palavras-chave: Cimentos dentários. Cerâmicas. Resinas compostas. Resistência ao cisalhamento. Materiais dentários.
Introduction
Dental esthetics has been given great emphasis in modern restorative dentistry. Dental materials are given much credibility when they show both functional and esthetic results, which in turn improve the quality of the treatment and patients' general oral health1.
Adhesive materials have dramatically transformed dentistry, not only in terms of conservation of tooth structure due to less invasive procedures, but also for allowing bonding between indirect restorations and the tooth2,3.
When the dimensions of the prepared cavity exceed the safe parameters for direct restorations, the use of indirect ones is a viable alternative, which will also help to strengthen the remaining tooth structure due to bonding mechanisms4. Amongst such restorative materials are dental ceramics and indirect composite resins.
Indirect composites can offer good posterior esthetics in case of large restorations5. In addition, they show lower polymerization shrinkage and other improved characteristics when compared to direct composites. Laboratory phases and higher costs are some of the disadvantages associated to indirect composites1,5.
Dental ceramics show various desirable characteristics, such as biocompatibility, high compres sion and abrasion resistance, shade stability and excellent potential for simulating the appearance of natural teeth4. However, they pose some problems such as low tensile strength, higher costs, and longer treatment courses1.
All indirect restorative materials need a dental cement for effective connection between tooth and restoration5,6. Dental cements used to bond an indirect restoration to a prepared tooth are called luting agents7. Traditionally, adhesive luting protocols involve the conditioning of the tooth structure followed by rinsing and application of an adhesive system to tooth substrate8. These luting protocols are considered time-consuming and susceptible to manipulation errors that could complicate the clinical procedure9,10.
In an attempt to simplify luting procedures, a new group of resin cements, the self-etching, self-adhesive resin cements have been introduced. The claim of these products is not requiring any pre-conditioning of enamel or dentine9,10.
According to manufacturers, self-adhesive agents contain dimethacrylate monomers and the innovative technology of polymerization in acid environment9,10. Such luting agents promote adhesion based on a specific monomer (phosphoric acid methacrylate ester), which is able to demineralize and infiltrate dentin, resulting in mechanical retention9,12. The setting reaction occurs from the polymerization of free radicals, which can be initiated by exposure to visible light or by oxyreduction12.
Self-adhesive luting agents have been recommended for full or partial indirect restorations, as well as ceramics and composites. In the case of ceramic crowns, these cements have produced better marginal adaptation by sealing the enamel and dentin when compared to etch-and-rinse ones11,13,14. Nonetheless, the bonding quality and its resistance on the internal surface of the restoration remain indeterminate.
The aim of this study was to investigate the influence of tooth substrate, type of luting agent as well as the restorative material on the shear bond strength of tooth-cement-restoration interfaces.
Materials and method
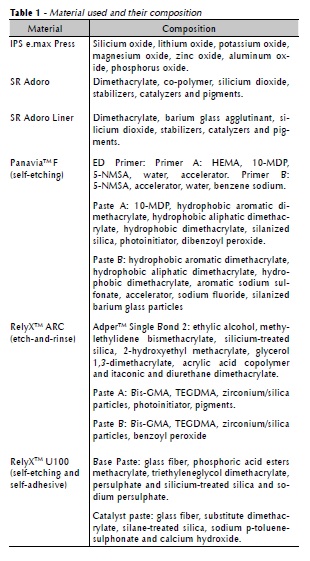
This study was approved by the Research Ethics Committee involving animals of the Sao Jose dos Campos Dental School (protocol nº 04/2009-PA/ CEP). Materials used and their specifications are found in Table 1.
One hundred and twenty bovine incisors were used as substrate. The teeth were embedded in acrylic resin with their buccal surface exposed and kept in distilled water at 37 ºC. The specimens were ground (Lab-Pol. 8-12. Extec Corp, Enfield, USA) under cooling conditions, until a flat and smooth surface of approximately 25 mm2 was obtained with 600-grit silicon carbide paper and polishing liquid. Half of the specimens were ground to expose the enamel, and the other half to expose dentin.
Specimens were randomly separated in 12 groups of 10, represented by allusive symbols according to the type of resin cement, tooth substrate, and restorative material (Table 2).
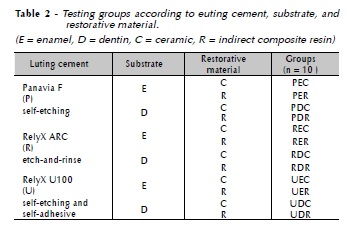
Sixty 3 x 3 mm lithium disilicate glass-ceramic cylinders (IPS e.max Press, Ivoclar Vivadent, Schaan, Liechtenstein.), and 60 indirect composite resin cylinders (SR Adoro, Ivoclar Vivadent, Schaan, Liechtenstein) were made.
The ceramic cylinders were obtained by lost wax casting. Twelve 25 mm x 3 mm cylindrical wax patterns were placed in an investment ring filled with investment material (IPS PressVest Speed, Ivoclar Vivadent, Schaan, Liechtenstein). After 45 minutes, the investment ring was placed in a furnace for the heating cycle. At 850 oC the ring was attached to the casting machine (Programat EP500, Ivoclar Vivadent, Schaan, Liechtenstein), where a ceramic block was heated and injected into the investment mold. The 12 cylinders were cut from the spring using diamond disks and taken to a precision cutting machine (Labcut 1010, Extec Corp, Enfield, USA). Sequential cuts produced 3 mm diameter x 3 mm long cylinders. One of the ends of the cylinder was identified using a permanent red marker to distinguish it from the testing surface.
For the indirect composite cylinders, a metal matrix with a central orifice (3 mm diameter x 3 mm height) was used. One of the flat surfaces of the cylinders was coated with a layer of adhesive (SR Adoro liner, Ivoclar Vivadent, Schaan, Liechtenstein) prior to the final polymerization (Lumamat 100, Ivoclar Vivadent, Schaan, Liechtenstein). The final polymerization was carried out for 25 minutes. Subsequently, the untreated surface was identified with a black permanent marker.
Three types of adhesive cements were used: Panavia F (Kuraray Medical, Kurashiki City, Japan); RelyX ARC (3M ESPE, St. Paul, MN, USA) and RelyX U100 (3M ESPE, St. Paul, MN, USA).
An adhesive tape with a 3 mm diameter orifice was placed on all specimens to determine the bonding area. Care was taken to place the orifice at an approximate distance of 3 mm from the cementum-enamel junction.
Prior to cementation, the ceramic cylinders were etched with 10% hydrofluoric acid (Porcelain etch conditioner, Dentsply, Petropolis, RJ, Brazil) for 20 s following the manufacturer's instructions. The specimens were rinsed with running water, dried, and a silane (RelyX Ceramic Primer, 3M ESPE, St. Paul, MN, USA) agent was applied.
According to the manufacturer, the composite cylinders, did not require pre-conditioning. Therefore, such step was not carried out.
Tooth substrate conditioning was performed following each resin cement manufacturer's instructions, which are described in (Box 1).
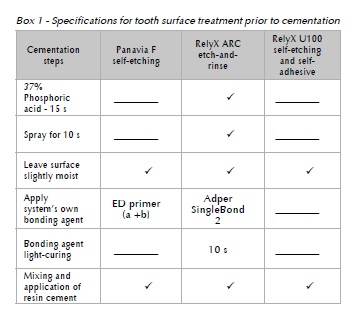
A layer of cement was applied to the treated surface of each cylinder, which in turn was positioned onto the circular tooth surface of each specimen. In order to standardize the cementation procedure, a modified parallelometer (Bio Art Equipamentos Odontológicos Ltda., São Carlos, SP, Brazil) was used. A fixed horizontal arm was adapted to the parallelometer, the spring of the vertical movable portion was removed, and a plane tip was coupled to the vertical arm so that each cylinder would be cemented in position. The weight of the vertical arm produced static and constant load of 2 Kg applied for 1 min to standardize the resin cement thickness. The excess of cement was removed using a microbrush and each quadrant of the cylinder was light-cured for 20 seconds from a 10 mm distance, with a light intensity of 600 mW/cm2. The specimens were placed in 37 oC-distilled water for one week.
Shear bond strength test was performed by a tip-shaped beveled knife fixed at the upper end of the universal test machine. This tip moved parallel to the long axis of the cementation plane and perpendicular to the restorative material cylinder with a crosshead speed of 0.5 mm/min until failure occurred. The shear strength data (MPa) were used to determine the debonding tension necessary to cause adhesion failure at the substrate/resin cement/ restorative material interfaces. The means of shear bond strength were determined by the following formula: σs = F/A, where σs is the shear bond strength, F is the applied load, and A is the bonded area.
Statistical comparisons were performed using three-way ANOVA (p<0.05) for the following factors: tooth substrate, luting cement, and restorative material. The Tukey test was used for multiple comparisons.
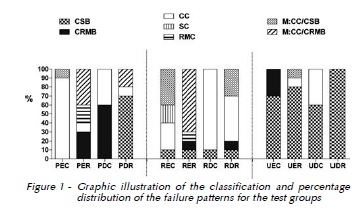
The failed surfaces were examined using a stereomicroscope (Stemi 2000C, Carl Zeiss), at 16X magnification. The failed surfaces were classified as follows: a) CSB - Cement/substrate bonding failure; b) CRMB - Cement/restorative material bonding failure; c) CC - Cement cohesive failure; d) SC - Substrate cohesive failure; e) RMC - Restorative material cohesive failure; f) M:CC/CSB - mixed failure: cement cohesive and cement/substrate bonding failure; g) M:CC/CRMB - mixed failure: cement cohesive and cement/restorative material bonding failure.
Results
The mean and standard deviation values from the shear bond strength test (MPa), according to the 12 experimental groups are shown in Table 3.

In order to determine the relationship among substrate, cement, and restorative material, the data were analyzed using three-way analysis of variance (ANOVA), after evaluating the assumptions of the model variance analysis. The residual values, resulting from the fit of the model adopted, were examined to assess their suitability for valid statistical inferences. After logarithmic transformation of the original data, residual values were adjusted to a normal distribution. Results of variance analysis are shown in Table 4.
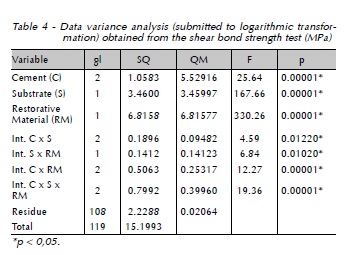
In Table 4, the interaction effect for the 3 experimental factors is statistically significant. Therefore, it is possible to establish that the relationship between the substrate (enamel and dentin), with the cement (Panavia F, RelyX ARC e RelyX U100) and the ceramic is different to that of the indirect restorative resin.
The results shown in Table 5 illustrate higher mean value for RelyX ARC cement compared to the other cements (p = 0.00001*). Regarding the substrate and restorative materials, it is also shown the superiority of the enamel and ceramic, respectively (p = 0.00001*).

Considering the experimental groups, it was demonstrated that the highest mean value was obtained for the REC group, which is significantly different from the other groups, except for the PEC group. The UDR group showed the lowest bond strength, which was significantly different from the other groups. The bond strength to enamel and to ceramic showed the highest results for all resin cements (p = 0.01020*). An unconfirmed tendency was observed for the UDC group, which revealed a relatively higher value when compared to the PER and RDC groups, but with statistically similar results as observed for the RER group. The letter C in Table 6 represents homogeneity.

Discussion
Luting cements represent a wide variety of materials used for placement of indirect restorations10. Due to their superior mechanical properties and greater retention, the use of resin cements has increased considerably in recent years15. The cements selected for this study present different composition and properties10.
Low bond strength results with self-adhesive cements have been previously reported in literature16,17. Self-adhesive cements are not capable of demineralizing/ dissolving the substrate thoroughly, and even no decalcification/demineralization can be observed17-19. It is believed that the weak interaction with the substrate, especially with dentin, occurs not only due to a low demineralization capacity, but also to the high viscosity of cement, which contains great quantities of glass particles9. Such weak interaction was also observed in this study through the low bond strength values and the high adhesive failure rates between cement and substrate in all groups where RelyX U100 was used (Figure 1).
The use of one etch-and-rinse resin cement, RelyX ARC, which requires an acid conditioning stage, resulted in the highest bond strength values. The results from the REC group, although higher, did not show statistical significance when compared with its equivalent cemented with Panavia F (PEC). This self-etching cement includes a primer which penetrates the enamel less than 1 øm-deep, however it is capable of yielding bond strength values equivalent to those of systems with a separate etching stage18.
Previous studies have shown that the adhesion of cements such as RelyX Unicem and Panavia F are reliable to enamel and dentin8,18,20. However, results obtained from the self-etch and self-adhesive were superior in dentin, except when there was a technique variation where the enamel etching was done with phosphoric acid before cementation9,20 . In the present study, RelyX U100 reached higher bond strength values to enamel and dentin when used to cement ceramic cylinder (UDC). However, the lowest bond strength value was obtained with the self-adhesive cement onto dentin using indirect composite (UDR). It is possible that this disagreement with previous study20 lies in the fact that despite being a system used in the presence of smear layer, insufficient quantity of water for ionizing the cement and/or a considerably thick smear layer may have interfered in the resin's interaction with dentin21.
The most favorable RelyX U100 results observed with enamel and ceramic (UEC) may be related to the relatively more stable bond between cement and ceramic, since most of the failures occurred between enamel and cement.
Another observation from this study was that the ceramic-bonded groups revealed higher bond strengths. The reason for this behavior can be based in two factors. First, it is known that such bond is favored by the micromechanical retention caused by the hydrofluoric acid etching as well as the silane agent, which binds chemically to the silica presented in the ceramic22,24. Second, the methodology used to assess bond strength was the shear test. The limitations involved in this type of test are well known and discussed by different studies25,26. In order to minimize the drawbacks of the shear test used on the present study, a saddle-shaped chisel was used to increase the contact area between the chisel and the specimen during the test, resulting in better distribution of forces along the adhesive interface. Even with this precaution, there is no guarantee that a uniform tension distribution occurs completely in the adhesive interface, which in this study corresponds to the cement luting. In the specimen used in this study, pure adhesive failure would be represented by cohesive failure of the cement. This indicates that both the union with the restorative material and the substrate was effective. Looking at Figure 1 it is possible to see that from twelve groups, just three showed predominantly this type of failure (PEC, RDC e RDR). From these groups, two used ceramic as restorative material. Also, these groups have not necessarily been associated with highest shear bond strengths. For these reasons, the shear bond strengths values are relative and should be analyzed with caution.
Another interesting result to be discussed is the deficient bond found between cement and indirect composite resin represented by CRMB and M:CC/ CRMB failures as seen in groups PER and RER in Figure 1. Even with the absence of any chemical or mechanical treatment of the bond surface of the indirect composite resin in order to promote bond with resin cements, it was expected the absence or fewer adhesive failures between these materials due to their chemical similarity. A possible explanation for these failures may be related to the composition of the indirect resin that has more fillers and fewer matrixes than most direct composite resins.
This study is important from the clinical point of view as the success of indirect restorations, either ceramics or resins depend upon the effectiveness of the bond with the tooth substrate. However, further investigation into the influence of other factors such as other bond strength methods, mechanical thermocycling, cavity shape, and polymerization shrinkage, simulating clinical longevity scenarios may help the clinician when choosing the best system for each individual situation.
Conclusion
Based on the methodology applied to this study, the following conclusion can be drawn: All the 3 experimental variables tested had influence on the shear bond strength of tooth-cement-restoration interfaces..
References
1. Burke EJ, Qualtrough AJ. Aesthetic inlays: composite or ceramic? Br Dent J 1994; 176:53-60. [ Links ]
2. Van Meerbeek B, Perdigão J, Lambrechts P, Vanherle G. The clinical performance of adhesives. J Dent 1998; 26:1-20.
3. Senawongse P, Harnirattisai C, Shimada Y, Tagami J. Effective bond strength of current adhesive systems on deciduous and permanent dentin. Oper Dent 2004; 29:196-202.
4. Burke FJ, Qualtrough AJ, Hale RW. Dentin-bonded allceramic crowns: current status. J Am Dent Assoc 1998; 129:455-60.
5. Nandini S. Indirect resin composites. J Conserv Dent 2010; 13:184-94.
6. De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Van Meerbeek B. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005; 84:118-32.
7. Prakki A, Carvalho RM. Dual cure resin cements: characteristics and clinical considerations. Pós-Grad Rev Fac Odontol 2001; 4:22-7.
8. Frankenberger R, Lohbauer U, Scaible RB, Nikolaenko SA, Naumann M. Luting of ceramic inlays in vitro: marginal quality of self-etch and etch-and rinse adhesives versus selfetch cements. Dent Mater 2008; 24:185-91.
9. De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater 2004 Dec; 20(10):963-71.
10. Pegoraro TA, Silva NRFA, Carvalho RM. Cements for Use in Esthetic Dentistry. Dent Clin N Am 2007; 51:453-71.
11. Behr M, Rosentritt M, Regnet T, Lang R, Handel G. Marginal adaptation in dentin of a self-adhesive universal resin cement compared with well-tried systems. Dent Mater 2004; 20:191-7.
12. Gerth HU, Dammaschke T, Züchner H, Schäfer E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites: a comparative study. Dent Mater 2006; 22:934-41.
13. Rosentrit M, Behr M, Lang R, Handel G. Influence of cement type on the marginal adaptation of all-ceramic MOD inlays. Dent Mater 2004; 20:463-9.
14. Ibarra G, Johnson GH, Geurtsen W, Vargas MA. Microleakage of porcelain veneer restorations bonded to enamel and dentin with a new self-adhesive resin-based dental cement. Dent Mater 2007; 23:218-25.
15. Fiori-Junior M, Matsumoto W, Silva RAB, Porto-Neto ST, Silva JMC. Effect of temporary cements on the shear bond strength of luting cements. J Appl Oral Sci 2010; 18:30-6.
16. Holderegger C, Sailer I, Schuhmacher C, Schläpfer R, Hämmerle C, Fischer J. Shear bond strength of resin cements to human dentin. J. Dent Mater 2008; 24:944-50.
17. Monticelli F, Osorio R, Mazzitelli C, Ferrari, Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J Dent Res 2008; 87:974-9.
18. Abo-Hamar SE, Hiller KA, Jung H, Federlin M, Schmalz G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Invest 2005; 9:161-7.
19. Al-Assaf K, Chakmakchi M, Palaghias G, Karanika-Kouma A, Eliades G. Interfacial characteristics of adhesive luting resins and composites with dentine. Dent Mater 2007; 23:829-39.
20. Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K. Bonding effectiveness of adhesive luting agents to emanel and dentin. Dent Mater 2007; 23:71-80.
21. Mazzitelli C, Monticelli F, Osorio R, Casucci A, Toledano M, Ferrari M. Effect of simulated pulpal pressure on selfadhesive cements bonding to dentin. Dent Mater 2008; 24:1156-63.
22. Söderholm KJ, Reetz EA. Factors affecting reliability of a resin-based cement joint. Gen Dent 1996; 44:296-8, 300, 302.
23. Saraçoglu A, Cura C, Cötert HS. Effect of various surface treatment methods on the bond strength of the heat-pressed ceramic samples. J Oral Rehabil 2004 Aug; 31:790-7.
24. Saavedra GSFA, Ariki EK, Federico CD, Galhano GA, Baldissara P, Bottino MA. Mechanical cycling of pre-molars restored with resinbonded glass-ceramic inlay restorations: effect of the acid neutralization and mechanical cycling on microtensile bond strength. Oper Dent 2009; 34:211-6.
25. Della Bona A, van Noort R. Shear vs. tensile bond strength of resin composite bonded to ceramic. J Dent Res 1995; 74:1591-16.
26. Della Bona A, Anusavice KJ, Mecholsky JJ, Jr. Failure analysis of resin composite bonded to ceramic. Dent Mater 2003; 19:693-9.
 Endereço para correspondência:
Endereço para correspondência:
Lucas Villaça Zogheib
Universidade do Sagrado Coração
Faculdade de Odontologia
Rua Irmã Arminda
Caixa Postal 611
99052-900 Bauru/SP
e-mail: lucaszogheib@yahoo.com.br













