Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RFO UPF
versão impressa ISSN 1413-4012
RFO UPF vol.17 no.3 Passo Fundo Set./Dez. 2012
Angina bullosa haemorrhagica (ABH): diagnosis and treatment
Angina bolhosa hemorrágica (ABH): diagnóstico e tratamento
Carlos Alberto Medeiros Martins I; Fernando Vacilotto Gomes II; Angelo Luiz Freddo II; Cláiton Heitz I; Fabiana Ckless Moresco I; Jorge Omar Lopes da Silveira I
I Department of Oral and Maxillofacial Surgery, School of Dentistry, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
II Department of Surgery and Orthopedics, School of Dentistry, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
ABSTRACT
Angina bullosa hemorrhagica is a disorder of unknown etiology characterized by the sudden onset of blood blisters in the oral and oropharyngeal mucosa. Objective: The present study describes six cases of patients diagnosed with ABH affecting the soft palate and tongue. Lesions appeared after meals, suggesting mastication trauma as the probable causative factor. From six, 04 occurred in the soft palate and 02 in the tongue, showing firstly a bubble blood, and subsequently to its rupture, the appearing of an ulcer. Final consideration: The authors discuss diagnostic criteria, essentially based on clinical data, as well as possible treatment approaches.
Keywords: Palate oft. Tongue. Hemorrhage. Pathology oral.
RESUMO
A angina bolhosa hemorrágica é uma desordem de etiologia desconhecida, caracterizada pela formação aguda de bolhas de conteúdo sanguíneo na mucosa bucal e orofaríngea. Objetivo: Neste estudo os autores descrevem seis casos clínicos de angina bolhosa hemorrágica, localizadas no palato mole e língua, na qual as lesões se desenvolveram subsequentemente após as refeições, sugerindo o trauma mastigatório como provável fator precipitante dessas lesões. Das seis, quatro ocorreram em palato mole e duas em língua, apresentando, primeiramente, uma bolha composta por sangue e, posteriormente ao seu rompimento, o aparecimento de uma úlcera. Considerações finais: Os autores discutem o diagnóstico, que é essencialmente clínico, assim como os métodos de tratamento dessa condição.
Palavras-chave: Palato mole. Língua. Hemorragia. Patologia bucal.
Introduction
Angina bullosa hemorrhagica (ABH) is a rare disorder of unknown etiology. It was first described and characterized as the sudden onset of blisters in the oral and oropharyngeal mucosa that cannot be attributed to vesiculo-bullous disorders (pemphigus), blood dyscrasias, autoimmune conditions or vascular disease. ABH tends to be more frequent in middle-aged people and in elderly, regardless of sex1.
Discussions about the etiology of ABH remain inconclusive, although most cases described in the literature seem to be associated with the long-term use of inhaled steroids2,3. Other authors have attributed the appearance of lesions to the consumption of hot beverages (thermal injury) and mastication-related traumatic injuries1,4.
The present study describes six cases of patients diagnosed with ABH in the oral cavity and discusses the characteristics and clinical evolution of lesions, possible complications, and adequate treatment approaches, considering mastication trauma as the main suspected etiologic agent.
Description of cases
Six cases of ABH seen at the Oral and Maxillofacial Surgery and Traumatology Department of the Emergency Unit of Hospital de Pronto Socorro in Porto Alegre, RS, Brazil, are described below. The signs and symptoms common to all patients are described first, followed by specific characteristics of each case.
During clinical examination, all patients reported having suffered some type of traumatic injury while eating, although only case no. one reported the intake of foods known to cause trauma to the oral mucosa, namely, meat seasoned with coarse sea salt. Case no. 1 was also the only smoker.
None of the six patients used any type of inhaled or systemic agents or drugs known to affect blood coagulation (acetylsalicylic acid or blood-thinners). Similarly, none of the patients had any underlying conditions that could provoke systemic abnormalities. Finally, it was not possible to identify any dietary pattern, or the consumption of any solid or liquid food, common to all cases treated.
Laboratory tests (full blood count, glucose levels, prothrombin time, activated partial thromboplastin described first, followed by specific characteristics of each case.
During clinical examination, all patients reported having suffered some type of traumatic injury while eating, although only case no. one reported the intake of foods known to cause trauma to the oral mucosa, namely, meat seasoned with coarse sea salt. Case no. 1 was also the only smoker.
None of the six patients used any type of inhaled or systemic agents or drugs known to affect blood coagulation (acetylsalicylic acid or blood-thinners). Similarly, none of the patients had any underlying conditions that could provoke systemic abnormalities. Finally, it was not possible to identify any dietary pattern, or the consumption of any solid or liquid food, common to all cases treated.
Laboratory tests (full blood count, glucose levels, prothrombin time, activated partial thromboplastin time, platelet count, and blood clotting time) were within normal limits in all cases.
All blood blisters (both single-and multiple-lesion presentations) ruptured spontaneously and resulted in areas of ulceration. All the four patients with ABH affecting the soft palate developed secondary infection and were treated using oral amoxicillin 500 mg every 8 hours for 7 days. Patients with lesions affecting the uvula and tongue did not report major pain and did not develop secondary infection.
During the medical visit, patients received detailed information about the disease, with a focus on its benign nature and course. An expectant approach was adopted in all cases (no surgical drainage was performed); all lesions ruptured spontaneously within 6 hours after the visit.
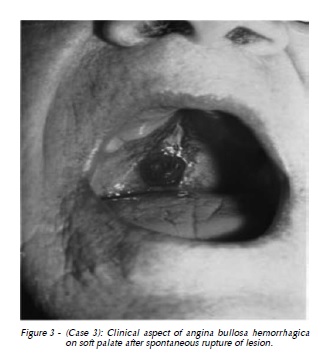
Below we briefly describe the main complaint and specific history of each patient (Table 1).
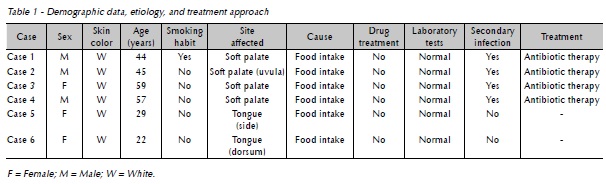
Case no 1
A 44-year old white male patient, smoker, was eating meat seasoned with coarse sea salt, when two large blood blisters appeared on the soft palate (Figure 1A). Figure 1B shows the ulcerated area observed two days after the first medical visit, following rupture of ABH.
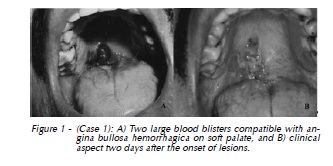
Case no 2
A 45-year old white male patient was having coffee with milk and bread with jam, when he noticed the presence of a blood blister on the soft palate, involving the uvula (Figure 2).
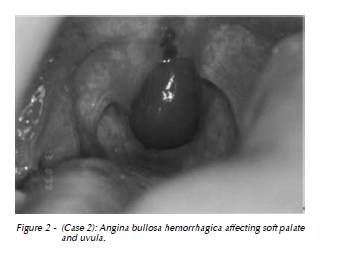
Case no 3
A 59-year old white female patient was having wine and conventional (non-crispy) foods for dinner. She then noticed the sudden onset of a blood blister on the soft palate. A few hours later, the blister ruptured spontaneously and extravasated blood contents. The patient experienced minor pain, followed by ulceration of the area (Figure 3).
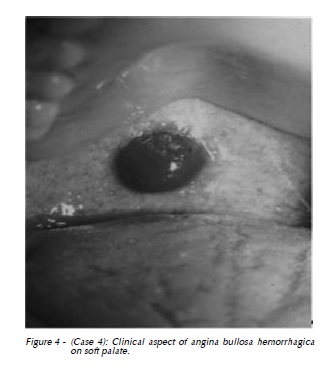
Case no 4
A 57-year old white male patient was having wine and conventional (non-crispy) foods for dinner when he noticed the onset of a blood blister on the soft palate (Figure 4).
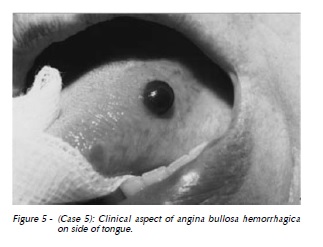
Case no 5
A 29-year old white female patient was having non-crispy foods when she noticed the sudden onset of an asymptomatic blood blister on the side of her tongue (Figure 5).
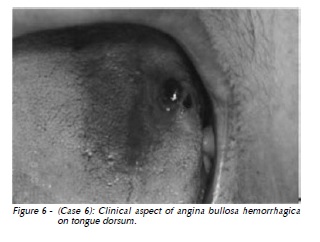
Case no 6
A 22-year old white female patient was having non-crispy sandwich cookies, when she realized her mouth was bleeding. While examining herself using a mirror, she noticed the presence of blood blisters on the tongue dorsum (Figure 6). The blisters ruptured spontaneously, extravasating blood and producing an ulcerated area.
Discussion
Several terms have been used to refer to the sudden onset of blood blisters in the oral and oropharyngeal mucosa. The term angina bullosa hemorrhagica (ABH) is currently consolidated, in spite of its apparent inaccuracy, as most blisters affecting the oral cavity and are not consistent with lesions usually referred to as angina3.
The chronic use of inhaled steroids is known to possibly affect collagen synthesis, causing atrophy of the mucous epithelium. The continuous use of these medicines may alter the synthesis of collagen and reduce its total content in the mucosa. In addition, tissue elasticity may decrease with the maturation of these fibers. As a result, the poor support provided by blood vessels present in the region could explain the development of ABH even in response to minor traumatic events5. Other authors have suggested that ABH could be caused by the use of inhaled steroids in patients with asthma and chronic obstructive pulmonary disease. This hypothesis is based on studies describing ABH in patients who had used steroid inhalers for over 5 years2,6. In our case series, none of the patients used inhaled steroids or presented any clinically relevant systemic abnormality or condition related with their complaint.
Although the precise etiology of ABH remains controversial, trauma during food intake seems to be an important precipitating factor for the disorder. Garlic et al.7 (1988) reported that excessive mechanical forces associated with mastication or minor thermal injuries are possible causes of ABH. The authors' assumption is based on the description of cases in which lesions appeared after dental procedures, sneezing, or endoscopic trauma8,9. Other authors have suggested that blisters could be the result of a weakened junction between epithelial and connective tissue, making non-keratinized mucosa more susceptible to trauma4. This fragility could allow minor traumatic events to interrupt the junction between both tissue layers and produce subepithelial oral blood blisters10.
In this sense, trauma seems to be the most common precipitating factor, especially during meals, as a result of thermal injuries to tissues or during the intake of solid foods that may traumatize the mucosa1,11. In a previous study involving 16 patients with ABH, the authors observed one common etiologic factor to all cases, namely, the consumption of hard, crispy foods, which caused trauma to the soft palate, according to patients12. In our study, trauma associated with eating also seemed to be the triggering factor in all patients, once all reported the intake of foods immediately before the onset of lesions, with no history of chronic use of inhaled steroids and normal laboratory test results.
ABH usually occurs at the junction between the hard and soft palate13. Some authors have reported that other oral areas characterized by non-keratinized mucosa, such as the lips, side and base of the tongue, floor of the mouth, and cheek mucosa, may also be affected14.
In our sample, all patients experienced a single episode of ABH, with no report of previous occurrences. Similarly, during postoperative control, there were no cases of lesion recurrence. The frequency of episodes is known to vary significantly across patients, and may recur within a few days from the first episode or after several months15.
ABH lesions have a sudden onset, during or immediately after meals, and are preceded by a burning sensation and xerostomia. Blisters are generally painless and rupture spontaneously within a few hours from their appearance, releasing red blood contents and producing erosion areas that heal within 7 to 10 days8. In the cases here described, all patients reported the sudden onset of lesions after meals. Blisters affecting the soft palate and uvula were associated with pain and burning sensation after rupture, differently from patients with blisters on the tongue, which were totally asymptomatic. All blisters in our series ruptured spontaneously, and there was no need for surgical drainage, as lesions were small and did not affect patients' dietary and respiratory functions.
The diagnosis of ABH is essentially based on clinical data; histopathological analysis reveals the presence of nonspecific ulcers containing a chronic inflammatory infiltrate consisting primarily of lymphocytes7,11,16. Thus, the previous medical and dental history of these patients should be revised to help distinguish between ABH and other systemic disorders. The assessment of hematologic and coagulation disorders should be performed so as to exclude the possibility of blood dyscrasia. Histopathological analysis is not necessary, provided the typical clinical pattern of lesions is observed.
Notwithstanding, when the diagnosis of ABH cannot be determined based solely on clinical and hematologic evaluation, then histopathological analysis becomes necessary for the establishment of a differential diagnosis in relation to other pathologies, such as erythema multiforme, bullous lichen planus, pemphigus, and epidermolysis bullosa13. Some authors have reported on the possible association between ABH and systemic disorders such as hypertension6,12 and diabetes17, although they also point to the need for further studies aimed at confirming such preliminary findings.
ABH treatment may include the use of anti-inflammatory and antibiotic agents, as well as antisepsis with mouthwash containing 0.25% or 0.12% chlorhexidine digluconate, to help relief painful symptoms and avoid secondary infections2,12,13,18,19. Because secondary infection of areas of ulceration are not uncommon, it is of paramount importance that the patient be provided with appropriate information and adequately followed. Patients presenting with lesions affecting the soft palate should be immediately prescribed antibiotic prophylactic therapy; in our study, all patients with lesions at the soft palate developed secondary infection. In other regions, patient follow-up will reveal whether the use of antibiotics is needed or not.
There is a recommendation in the literature that oral antiseptics such as chlorhexidine digluconate be prescribed to all patients, as these agents seem to have an important role in the prevention of infections after blister rupture. Our findings apparently confirm the benefit of that recommendation: no antiseptic agent was prescribed before the clinical diagnosis of infection, and all four cases with lesions affecting the soft palate developed secondary infections after rupture.
Surgical drainage is not necessary in small, localized lesions that do not functionally affect the airways, as these lesions are likely to rupture within some hours. Conversely, it is indicated whenever large blisters are present in the palate, causing a feeling of suffocation6,10. Pahl et al.9 (2004) have reported a case of ABH in a 56-year old female patient who developed a rapidly growing blood blister on the soft palate that caused oropharyngeal airway obstruction. Because of the large lesion size, nasotracheal intubation was not feasible, and tracheostomy was required to allow subsequent ABH drainage.
Final considerations
Through this study, the authors discussed the diagnostic criteria, essentially based on clinical data, as well as possible treatment approaches. It is therefore the realization of an accurate diagnosis and determining the pathology's beginning are essential for the establishment of treatment.
Conflict of interest statement: The authors have nothing to disclose.
References
1. Badham NJ. Blood blisters and the oesophageal cast. J Laryngol Otol. 1967; 81(7): 791-803. [ Links ]
2. High AS, Main DM. Angina bullosa haemorrhagica: a complication of long-term steroid inhaler use. Br Dent J. 1988;165(5):176-179.
3. Kirtschig G, Happle R. Stomatopompholyx hemorrhagica. J Am Acad Dermatol. 1994;31(5):804-805.
4. Hopkins R, Walker DM. Oral blood blisters: angina bullosa haemorrhagica. Br J Oral Maxillofac Surg. 1985;23(1):9-16.
5. Higgins EM, du Vivier AW. Angina bullosa haemorrhagica--a possible relation to steroid inhalers. Clin Exp Dermatol. 1991;16(4):244-246.
6. Serra D, De Oliveira HS, Reis JP, Vieira R, Figueiredo A. Angina bullosa haemorrhagica: a disorder to keep in mind. Eur J Dermatol. 2010;20(4):509-510.
7. Garlick JA, Calderon S. Oral blood blisters in angina bullosa haemorrhagica secondary to trauma of eating and dental injection. Br Dent J. 1988;165(8):286-287.
8. Deblauwe BM, van der Waal I. Blood blisters of the oral mucosa (angina bullosa haemorrhagica). J Am Acad Dermatol. 1994;31(2):341-344.
9. Pahl C, Yarrow S, Steventon N, Saeed NR, Dyar O. Angina bullosa haemorrhagica presenting as acute upper airway obstruction. Br J Anaesth. 2004;92(2):283-286.
10. Corson MA, Sloan P. Angina bullosa haemorrhagica: an unusual complication following crown preparation. Br Dent J. 1996;180(1):24-25.
11. Stephenson P, Lamey PJ, Scully C, Prime SS. Angina bullosa haemorrhagica: clinical and laboratory features in 30 patients. Oral Surg Oral Med Oral Pathol. 1987;63(5):560-565.
12. Horie N, Kawano R, Inaba J, Numa T, Kato T, Nasu D, et al. Angina bullosa hemorrhagica of the soft palate: a clinical study of 16 cases. J Oral Sci. 2008;50(1):33-36.
13. Giuliani M, Favia GF, Lajolo C, Miani CM. Angina bullosa haemorrhagica: presentation of eight new cases and a review of the literature. Oral Dis. 2002;8(1): 54-58.
14. de las Heras ME, Moreno R, Nunez M, Gomez MI, Ledo A. Angina bullosa hemorrhagica. J Dermatol.1996;23(7):507-509.
15. Grinspan D, Abulafia J, Lanfranchi H. Angina bullosa hemorrhagica. Int J Dermatol. 1999;38(7):525-528.
16. Martini MZ, Lemos CA, Jr., Shinohara EH. Angina bullosa hemorrhagica: report of 4 cases. Minerva Stomatol. 2010;59(3):139-142.
17. Petruzzi M. Angina bullosa haemorrhagica: a case report. J Biol Regul Homeost Agents. 2009;23(2): 125-126.
18. Gibson J. Oropharyngeal blood blisters are known as angina bullosa haemorrhagica. Br Med J. 1997;314(7094):1625.
19. Yip HK. Angina bullosa haemorrhagica: a case report and a concise review. Gen Dent. 2004;52(2):162-164.
 Endereço para correspondência:
Endereço para correspondência:
Angelo Luiz Freddo
Faculdade de Odontologia da UFRGS
Rua Ramiro Barcelos, 2492 (3º floor)
90035-003 Porto Alegre - RS
e-mail: angelofreddo@gmail.com













