Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Arquivos em Odontologia
versão impressa ISSN 1516-0939
Arq. Odontol. vol.46 no.3 Belo Horizonte Jul./Set. 2010
Interdisciplinary approach to treating patients with Epithelioid Angiosarcoma: a case report
Conduta Interdisciplinar para tratar paciente com Angiossarcoma Epitelióide: relato de um caso-clínico
Raquel Teodoro Santos Teixeira; Henrique Zanoni Fernandes; Haglay Palandi de Oliveira Belloti; Maria das Graças Vilela Goulart; Mônica Fernandes Gomes
Bioscience Center for Special Health Care Needs, Dental School, São Paulo State University (UNESP), São José dos Campos, SP, Brazil
ABSTRACT
Epithelioid angiosarcoma is a rare malignant neoplasm found in vascular endothelial cells. The present study aims to describe the radiological, clinicopathological, and immunohistochemical findings of a case of epithelioid angiosarcoma located in the posterior mediastinum of a 65-year-old male patient who underwent surgery and clinical treatment (Doxorubicin-based chemoterapy). It could be observed that the patient presented poor oral hygiene, severe cervical erosions in his teeth, chronic caries, periodontal disease, and periapical abscess. For this reason, the participation of a dentist in an interdisciplinary team is of utmost importance. Oral support treatment also becomes essential in an attempt to eliminate all foci of oral infections, as well as minimize morbidity and improve the general condition of the patient before, during, and after oncological treatment. In addition, the dentist will work toward the education and motivation of the patient to take on an appropriate oral hygiene so as to minimize the oral complications of chemotherapy, in turn providing better conditions for the patient to eat, speak, socialize, and maintain a high quality of life.
Uniterms: Epithelioid angiosarcoma. Drug therapy. Oral health.
RESUMO
Angiossarcoma epitelióide é uma neoplasia maligna rara das células vasculares endoteliais. Neste estudo, foram descritos os achados radiológicos, clinicopatológicos e imunohistoquímicos de um caso de angiossarcoma epitelióide no mediastino posterior, em um paciente de 65 anos de idade, submetido à cirurgia e tratamento clínico (quimioterapia com Doxorubicina). Observou-se que o paciente apresentava higiene bucal precária, erosões cervicais severas, lesões de cárie crônicas, doença periodontal e abscesso periapical. A participação do dentista em uma equipe multidisciplinar é muito importante. O tratamento de suporte é essencial para eliminar todos os focos de infecção oral, minimizar a morbidade e melhorar as condições gerais do paciente antes, durante e após o tratamento oncológico. Além disso, é importante que o dentista trabalhe na educação e motivação do paciente para conseguir uma adequada higienização bucal e para tentar minimizar as complicações orais da quimioterapia, melhorando as condições para que o paciente se alimente, fale e socialize-se, tendo uma melhor qualidade de vida.
Descritores: Angiossarcoma epitelióide. Quimioterapia. Saúde bucal.
INTRODUCTION
Angiosarcoma is a rare malignant vascular neoplasm which constitutes less than 1% of all sarcomas. Epithelioid angiosarcoma (EA) is a rare variant of angiosarcoma, which is characterized by a high-grade malignant neoplasm, which consists of an atypical, multilayered, or solid endothelial proliferation and vasoformative architecture, presenting necrosis and an area of hemorrhage1-5. The histologic hallmark of AE is represented by the presence of sheets and groups of atypical endothelial cells with prominent epithelioid morphologies. The cells are usually large and polygonal, containing abundant eosinophilic cytoplasm, a large nucleus with open chromatin, a prominent eosinophilic nucleolus, and an occasional intracellular lumina containing red blood cells1,4-7. Immunohistochemical analysis that demonstrates the endothelial nature of the neoplasm is frequently positive for specific vascular markers (CD31, CD34, factor VIII), and keratin1,2,5,6. This neoplasm has been described in a wide range of sites, such as in deep soft tissues, the uterus, the thyroid, adrenals, the breast, the pleura, the lung, the pharynx, the skin, the prostate, seminal vesicles, and bones2,4-7. Prior literature reports that this neoplasm takes on an aggressive course and has a strong tendency to recur locally and to metastasize. Therefore, the recommended treatment which offers the best chance of survival to the patient is surgery, together with radiotherapy and chemotherapy 3,4,7,8.
The patients receiving chemotherapy are susceptible to oral complications which can be associated with significant morbidity and even mortality. The myelosuppression and immunosuppression which accompany current therapies may lead to severe stomatitis, oral infections, hemorrhage, xerostomia, among other oral complications9-16.
Therefore, the present study aimed to report a case of epithelioid angiosarcoma; discuss
its radiographic, clinicopathological, and immunohistochemical findings; and correlate these findings with the characteristics found in the literature. The study will also describe the oral conditions of the patient and guide the interdisciplinary team toward the necessary preventive and therapeutic dental care to be implemented before and during chemotherapeutic treatment. The dentist, as a member of the interdisciplinary team, must prepare the patient for chemotherapy, given that the dental procedures are important in eliminating all the foci of oral infections as well as improving the patients’ quality of life before, during, and after oncological treatment.
CASE REPORT
A 65-year-old, leucoderm, male patient was referred to the Special Health Care Needs Association (ASPE, São José dos Campos, Brazil) for oral evaluation (Figure 1).
Upon examining the patient’s medical records, the patient reported to be a user of alcohol and a smoker for 52 years and complained of an intense pain in the thoracic region (Figure 2).
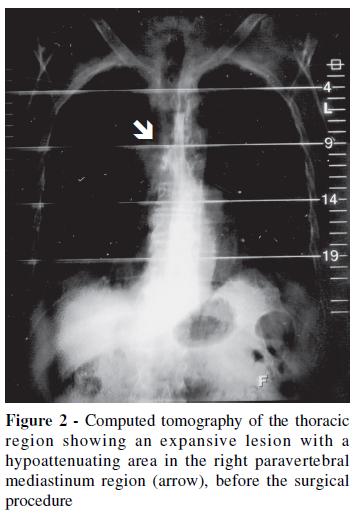
Computed tomography showed a lesion located in the right paravertebral (T6 level) posterior mediastinum region, with a size of 3.9 x 3.0 cm, in addition to pulmonary interstitial infiltration in the right base of the organ and two homogeneous hypoattenuating nodular images, of 1.0 cm in size, in the liver (Figure 3a-b).

Upon being submitted to a surgical resectioning of the mass of posterior mediastinum, the histological examination showed a malignant neoplasm consisting of well-formed irregular vascular spaces lined with atypical epithelioid cells and solid nests and cords of atypical epithelioid cells with moderate mitotic activity. Necrosis areas (less of 50%) and interstitial hemorrhages could also be observed (Figure 4a-c).
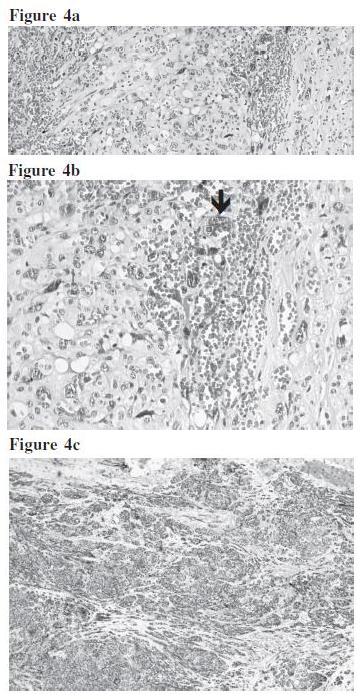
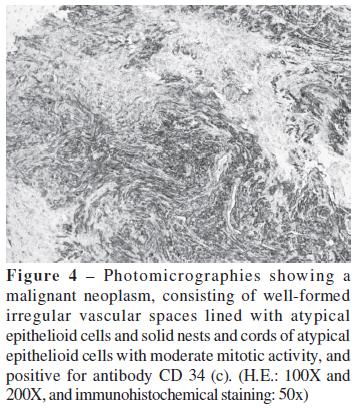
Upon immunohistochemical examination, neoplasm cells proved to be positive for CD31, CD34, and fascin. The diagnosis was epithelioid angiosarcoma, which was partially excised. Two months after surgery, postoperative treatment began with chemotherapy, which consisted of six cycles of doxorubicin (Adriblastina® RD, Pharmacia Italia S.p.A, Milan, Italy), at intervals of 21 days between each cycle. The support medications used included ondansetron HCl dihydrate (antiemetic, Zofran® Glaxo Operations UK Limited, Ware, England), and dexamethasone (Decadron®, Aché Laboratórios Farmacêuticos S.A., Guarulhos, SP, Brazil).
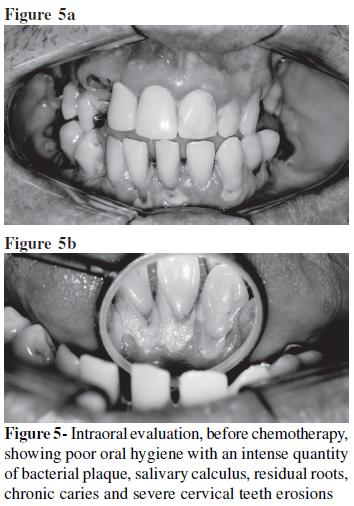
Upon extra and intraoral examination, after the first chemotherapy session, icteric face; pale lips; atrophic oral mucosa; tongue coating; poor oral hygiene with an intense quantity of bacterial plaque in all dental elements; dental calculus; and gingival bleeding associated with periodontal pockets could be observed. The patient did not have maxillary right and left first molars, a left second premolar, nor the mandibular right and left first molars. The residual roots stemmed from the maxillary right second molar and canine, the maxillary left first premolar, and the mandibular right and left second molars. In addition, the patient presented a poorly adapted dental prothesis, chronic caries, and severe cervical teeth erosions (Figure 5a-b).
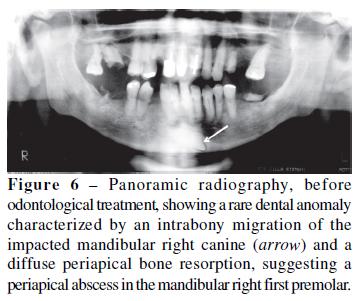
The panoramic radiography revealed a rare dental anomaly characterized by an intrabony migration of the impacted mandibular right canine and a diffuse periapical bone resorption, suggesting a periapical abscess in the mandibular right first premolar (Figure 6).
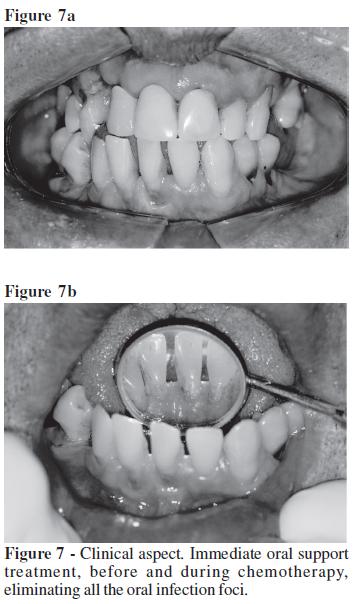
The supporting dental treatment was carried out two weeks before and during chemotherapy. First, all the extra and intraosseous infection foci were eliminated. The patient then underwent periodontal treatment and education concerning oral hygiene, including the performance of scaling, planning, and coronary and radicular polishing procedures, and the application of fluor. After antibiotic prophylaxis, the extractions of the residual roots, endodontic treatment due to presence of periapical abscess, and deep caries treatment were performed (Figure 7a-b).
During chemotherapy, the oral mucosa remained dry and erithematous, and a significant reduction in salivary flow occurred. In this phase of treatment, the patient was advised on tooth brushing techniques, used an artificial saliva solution (Salivan®, APSEN Farmacêutica S/A, São Paulo, SP, Brazil) six times daily to treat the reduction in salivary flow, and underwent oral mucosa evaluations weekly.
DISCUSSION
Epithelioid Angiosarcoma is a rare malignant neoplasm found in vascular endothelial cells which affects a wide age range, with a higher incidence among elderly patients4,7. The peak incidence in the seventh decade of life related by Teltzrow et al.17 was also found in this report.
This neoplasm has been reported to appear in diverse sites, such as deep soft tissues, the uterus, the thyroid, adrenals, the breast, the pleura, the lung, the pharynx, the skin, the prostate, seminal vesicles, the bone, the maxillary sinus, and the gingiva2-7,however, to our knowledge, this has not been previously reported in the paravertebral (T6 level) posterior mediastinum region, described in this case.
A variety of conditions are known to be associated with the development of angiosarcoma; these include chronic edematous states, sun exposure, prior irradiation, and, in more rare cases, chronic exposure to foreign material7. Although reports show no alcohol and tobacco consumption associated with epithelioid angiosarcoma, these factors may well increase the risk for further malignancy and may even compromise the chemotherapy treatment18,19. The patient in this case report had a previous history of 52 years of cigarette smoking and alcohol consumption.
Pathologic diagnosis is characterized by polygonal or oval cells with atypical irregular nuclei and vascular spaces lined with such cells and surrounded by hemorrhagic phenomena. Immunohistochemical findings that demonstrate the endothelial nature of the tumor proved to be positive for CD31, CD34, factor VIII, and keratin, whose coexpression is frequently seen in epithelioid angiosarcoma1,4-7. In this study, it was positive only for CD31, CD 34, and fascin. Poorly differentiated angiosarcomas are best distinguished from other spindle cell sarcomas with immunohistochemistry to help diagnosis, especially when the CD31 antigen is present, the most sensitive endothelial markers3,4. Fascin is a globular actin cross-linking protein that plays a key role in forming parallel actin bundles in cell protrusions, which are key specializations of the plasma membrane for environmental guidance and cell migration. Fascin is widely expressed in mesenchymal tissues and the nervous system, while it is low or absent in adult epithelia. Recent data from a number of laboratories have highlighted that fascin is up-regulated in many human carcinomas and correlated with the clinical aggressiveness of tumors and poor patient survival20,21. In this study, the neoplasm proved to be positive for fascin, which could confirm the common trend of this tumor to metastasize and reduce the patient’s life expectation.
Since angiosarcoma is characteristically a metastasizing tumor, it is always described in the literature as simultaneously involving 2 to 3 organs. In many cases, the primary focus cannot be identified, and cardiopulmonary involvement is common5,7. Lopez et al.5 found a widespread involvement of the lungs, digestive tract, spleen, liver, and kidney. In this case, the primary focus was in the right paravertebral (T6 level) posterior mediastinum region. Pulmonary interstitial infiltration and hepatic nodules could also be observed. After the diagnosis, the patient was submitted to surgical and chemotherapy treatment.
For chemotherapy, anti-neoplasm drugs presenting cytotoxic properties were used in neoplasic cells, as well as in tissues of fast proliferation, such as bone marrow, pilous follicles, oral and gastrointestinal mucosa, which are most sensible to the anti-proliferative effects of these drugs12,22. Doxorubicin is an anti-neoplasm drug which is widely used in the treatment of neoplasms, such as carcinoma of the breast, lung, bladder, thyroid and ovary; sarcomas of bone and soft tissues; Hodgkin and non-Hodgkin lymphomas; neuroblastoma; Wilms Tumor; acute lymphoblastic leukemia; and acute myeloid leukemia. This drug is obtained from the bacterium Streptomyces peuceticus. Its mechanism of action consists of connecting itself to the DNA and inhibiting the synthesis of nucleic acid. Its dose limit is determined when the patient presents myelosuppression and cardiotoxicity. Its effects include hair loss, nausea, vomiting, low number of white and red blood cells and platelets, heart arrhythmias, mucositis, xerostomia, sore mouth and taste change, discolored urine, and skin changes23,24. In this case report, the drug used was doxorubicin, whose side effects included hair loss, nausea, vomiting, myelosuppression, fever, depression, as well as saliva flow reduction and its subsequent consequences.
The most common oral complications during the chemotherapy include oral mucositis, xerostomia, hemorrhage, and an increase in the index of caries and opportunistic infections9-16,25. IN an attempt to minimize the oral complications during chemotherapy, the patient must be evaluated by the dentist prior to beginning chemotherapy to identify possible situations of oral infections, such as caries, gingivitis, periodontitis, and periapical lesions that can cause generalized infections. In addition, myelosuppression can increase a pre-existing periodontal disease. Once the oral lesions have been detected, the dentist then applies the most appropriate dental treatment to eliminate all foci of infection. The clinical procedures at this stage include oral prophylaxis, roots extractions, draining of abscesses, endodontic and surgical treatment of the periapical lesions, scaling and planning of the crown and dental roots, instructions on hygiene and topic fluoride application9-16,25,26. Our patient presented some foci of oral infections, such as severe periodontitis, extensive chronic caries, and periapical abscess. These lesions were associated with a large amount of bacterial plaque and dental calculus. Therefore, all the foci of infections had been completely removed, promoting a reduction in the gingival inflammation and bleeding and avoiding the sprouting of oral mucositis and candidiasis. In this light, oral care becomes essential in minimizing morbidity and improving the general conditions of the patient before and during oncological treatment and conditions regarding patient nutrition.
During chemotherapy, the patient also complained about dry mouth. According to Coleman27, the salivary glands are directly affected, thus resulting in a reduced salivary flow. This condition has significant consequences on both the hard and soft components of the oral cavity and can subsequently compromise its functionality. This can lead to swallowing difficulties, which also contribute to bacteria colonization and bacterial plaque formation, which in turn lead to dental caries and periodontal diseases28,29. In the present case, a severe reduction in salivary flow could be observed. Therefore, an artificial saliva solution to maintain oral health of our patient was recommended.
Furthermore, our patient presented no oral mucositis. According to Coleman28, Sonis11, and Gomes et al.16, the younger the patient, the greater the possibility of chemotherapy affecting the mouth. In the present case, the patient’s age, oral hygiene, and the use of the artificial saliva have prevented the sprouting of oral mucositis.
CONCLUSION
The participation of a dentist in an interdisciplinary team is of utmost importance. The oral support treatment is essential in eliminating all foci of oral infections as well as in minimizing morbidity and improving the general conditions of the patients before, during, and after oncological treatment. Moreover, the dentist will work on the education and motivation of the patient to take on an appropriate oral hygiene in an attempt to minimize the oral complications of chemotherapy, in turn providing better conditions for the patient to eat, speak, socialize, and maintain a high quality of life.
ACKNOWLEDGEDMENTS
We are grateful to Doctor Venâncio Avancini Ferreira Alves from the Cytophatological, Pathological, Anatomy, Cytophatological, and Imuno-histochemical Center (São Paulo, Brazil); to Doctor Carlos Eduardo de Godoy from the Cytophatological, Pathological, and Anatomy Laboratory; to Maria Alcionéia Carvalho de Oliveira from the Bioscience Center for Special Health Care Needs; and to the Quaglia Laboratory (São José dos Campos, São Paulo, Brazil).
REFERENCES
1. Mentzel T, Katenkamp D. Intraneural angiosarcoma and angiorsarcoma arising in benign and malignant peripheral nerve sheath tumours: clinicopathological and immunohistochemical analysis of four cases. Histopathology. 1999; 35:114-20. [ Links ]
2. Roh MS, Seo JY, Hong SH. Epithelioid angiosarcoma of the pleura: a case report. J Korean Med Sci. 2001; 16:792-5. [ Links ]
3. Triantafillidou K, Lazaridis N, Zaramboukas T. Epithelioid angiosarcoma of the maxillary sinus and the maxilla: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:333-7. [ Links ]
4. Deshpande V, Rosenberg AE, O’Connell JX, Nielsen GP. Epithelioid angiosarcoma of the bone: a series of 10 cases. Am J Surg Pathol. 2003; 27:709-16. [ Links ]
5. López L, Iriberri M, Cancelo L, Gómez A, Uresandi F, Atxotegui V. Persistent hemoptysis secondary to extensive epithelioid angiosarcoma. Arch Bronconeumol. 2004, 40:188-90. [ Links ]
6. Macías-Martínez V, Murrieta-Tiburcio L, Molina-Cárdenas H, Domínquez-Malagón H. Epithelioid angiosarcoma of the breast: clinicopathological, immunohistochemical, and ultrastructural study of a case. Am J Surg Pathol. 1997; 21:599-604. [ Links ]
7. Wehrli BM, Janzen DL, Shokeir O, Masri BA, Byrne SK, O’Connell JX. Epithelioid angiosarcoma arising in a surgically constructed arteriovenous fistula: a rare complication of chronic immunosuppression in the setting of renal transplantation. Am J Surg Pathol. 1998; 22:1154-9. [ Links ]
8. Refre GR, Buenconcejo LS, Aleta KNR, Tan- Liu NS, Wang AD. Breast mass in a male patient: a case of primary thoracic epithelioid angiosarcoma. Philipp J Intern Med. 2006; 44:197-203. [ Links ]
9. Rosemberg SW. Oral complications of cancer chemotherapy: a review of 398 patients. J Oral Med. 1986; 41:93-7. [ Links ]
10. Massler Jr CF. Preventing and treating oral complications of cancer therapy. Gen Dent. 2000; 48:652-5. [ Links ]
11. Sonis ST, Fey EG. Oral complications of cancer therapy. Oncology. 2002; 16:680-95. [ Links ]
12. Barasch A, Peterson DE. Risk factors for ulcerative oral mucositis in cancer patients: unanswered questions. Oral Oncol. 2003; 39:91-100. [ Links ]
13. McGuire DB. Barriers and strategies in implementation of oral care standards for cancer patients. Support Care Cancer. 2003; 11:435-41. [ Links ]
14. Redding SW. Oral complications of cancer therapy. Tex Med. 2003; 99:54-7. [ Links ]
15. Sadler GR, Stoudt A, Fullerton JT, Oberle- Edwards LK, Nguyen Q, Epstein JB. Managing the oral sequelae of cancer therapy. Medsurg Nurs. 2003; 12:28-36. [ Links ]
16. Gomes MF, Kohlemann KR, Plens G, Silva MM, Pontes EM, Rocha JC. Oral manifestations during chemotherapy for acute lymphoblastic leukemia: a case report. Quintessence Int. 2005; 36:307-13. [ Links ]
17. Teltzrow T, Hallermann C, Muller S, Schwipper V. Foreign body-induced angiosarcoma 60 years after a shell splinter injury. Mund Kiefer Gesichtschir. 2006; 10:415-8. [ Links ]
18. El-Bayoumy K, Chung FL, Richie J, et al. Dietary control of cancer. Proc Soc Exp Biol Med. 1997; 216:211-23. [ Links ]
19. Pinto BM, Trunzo JJ. Health behaviors during and after a cancer diagnosis. Cancer. 2005; 104:2614-23. Errata em: Cancer. 2006; 106:1641. [ Links ]
20. Hashimoto Y, Skacel M, Adams JC. Roles of fascin in human carcinoma motility and signaling: prospects for a novel biomarker? Int J Biochem Cell Biol. 2005; 37:1787-804. [ Links ]
21. Yoder BJ, Tso E, Skacel M, et al. The expression of fascin, an actin-bundling motility protein, correlates with hormone receptornegative breast cancer and a more aggressive clinical course. Clin Cancer Res. 2005; 11:186- 92. [ Links ]
22. Silverman S. Oral cancer: complications of therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:122-6. [ Links ]
23. Martindale. The complete drug reference. 33nded. London: The Pharmaceutical Press; 2002. [ Links ]
24. Kilickap S, Barista I, Akgul E, Aytemir K, Aksoy A, Tekuzman G. Early and late arrhythmogenic effects of doxorubicin. South Med J. 2007; 100:262-5. [ Links ]
25. Sonis ST. Oral mucositis in cancer therapy. J Support Oncol. 2004; 2:3-8. [ Links ]
26. Raut A, Huryn JM, Hwang, FR, Zlotolow, IM. Sequelae and complications related to dental extractions in patients with hematologic malignancies and the impact on medical outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:49-55. [ Links ]
27. Coleman S. An overview of oral complications of adult patients with malignant haematological conditions who have undergone radiotherapy or chemotherapy. J Adv Nurs. 1995; 22:1085-91. [ Links ]
28. Branchi R, Fancelli V, Durval E, De Salvador A. The patient with xerostomia: medical therapy, prosthetic therapy. Minerva Stomatol. 2003; 52:455-63. [ Links ]
29. Friedlander AH, Friedlander IK, Gallas M, Velasco E. Late-life depression: its oral health significance. Int Dent J. 2003; 53:41-50. [ Links ]
 Autor correspondente:
Autor correspondente:
Profª Adja Mônica Fernandes Gomes
Avenida Engenheiro José Longo, 777
CEP: 12245-000 - São José dos Campos – SP - Brazil
e-mail: mfgomes@fosjc.unesp.br
Received on 02/02/2008 – Accepted on 25/05/2008
Contato: mfgomes@fosjc.unesp.br













