Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.17 no.33 Canoas Jul./Dez. 2011
SCIENTIFIC ARTICLE
Occlusal adjustment in the treatment of secondary traumatic injury
Equilíbrio oclusal no tratamento de injúria traumática secundária
Raulino Naves Borges1; Bárbara Morais Arantes2; Denise Ferreira Vieira3; Orlando Aguirre Guedes4; Carlos Estrela5
1Professor of Dental Occlusion – UFGO, Goiânia, Brazil
2Post-graduate student – UFGO, Goiânia, Brazil
3Dental student, School of Dentistry – UFGO, Goiânia, Brazil
4Post-graduate student – UFGO, Goiânia, Brazil
5Chairman and Professor of Endodontics – UFGO, Goiânia, Brazil
ABSTRACT
The success of the rehabilitation treatment is associated with the relationship between occlusion and periodontal status. When occlusal loads exceed the ability of the periodontium to resist and distribute the resulting forces, injuries may develop, leading to failures in dental practice. A 35-year-old female patient presented at the Occlusion and Orofacial Pain Research Center at the School of Dentistry, Universidade Federal de Goiás, Brazil, complaining of pain and mobility in the maxillary central incisors and sensitivity in the mandibular left incisors and canine. Symptoms began after cast metal restoration was performed in tooth #27. Clinical examination revealed a signifi cant difference of 1 mm between centric relation and habitual occlusion, presence of a periodontal pocket 5 mm deep in the mesial aspect of tooth #11, and an increased vertical dimension of occlusion caused by occlusal interference between teeth #27 and #37. Radiographic examination detected vertical bone loss between teeth #21 and #11, on the mesial aspect of tooth #33 and between the lower incisors. The lower teeth also showed radiographic evidence of periapical lesions. Occlusal interference caused anterior projection of the mandible to the right, overloading the incisors. Treatment by occlusal adjustment was performed to promote an equal incidence of forces on all aspects of the teeth. Twelve sessions were required to achieve a balanced occlusion and restore the physiological vertical dimension of occlusion. Six months after treatment, there was radiographic evidence of newly formed bone tissue between teeth #11 and #21, regression of apical periodontitis in the lower teeth, and a decrease in mobility and all associated symptoms. Secondary traumatic injury may be responsible for changes in apical tooth structures. Occlusal adjustment may favor the direction of occlusal forces to the long axis of the teeth.
Keywords: Occlusal adjustment, traumatic dental occlusion, maxillomandibular relation record, occlusion.
RESUMO
O sucesso do tratamento reabilitador associa-se à relação entre a oclusão e a periodontia. Quando cargas oclusais excedem a capacidade periodontal de suportar e distribuir as forças resultantes, podem ocorrer traumas,os quais seriam responsáveis por fracassos na prática odontológica. Uma paciente de 35 anos compareceu ao Centro de Pesquisa em Oclusão e Dor Orofacial da Faculdade de Odontologia, Universidade Federal de Goiás, Brasil, com queixa de dor e mobilidade nos incisivos centrais superiores e sensibilidade nos dentes incisivo e canino esquerdos inferiores. A sintomatologia teve início após a confecção de uma restauração metálica fundida no dente 27. Ao exame clínico, observou-se diferença significativa de 1 mm entre a relação central e a oclusão habitual, presença de bolsa periodontal de 5 mm na face mesial do dente 11 e aumento da dimensão vertical de oclusão provocada por interferência oclusal entre os dentes 27 e 37. O exame radiográfi co detectou perda óssea vertical entre os dentes 21 e 11, na face mesial do dente 33 e entre os incisivos inferiores. Os dentes inferiores também apresentavam lesão radiolúcida indicativa de periapicopatia. O contato interferente provocava projeção mandibular anterior e para a direita, promovendo sobrecarga nos incisivos. O tratamento por ajuste oclusal foi indicado para promover igualdade de incidência de forças em todos os elementos dentários. Foram necessárias 12 sessões para obtenção de uma oclusão equilibrada e resgate da dimensão vertical de oclusão fisiológica. Seis meses após o tratamento, observou-se ao exame radiográfico neoformação óssea entre os dentes 11 e 21, regressão da periapicopatia nos dentes inferiores e redução da mobilidade e de toda sintomatologia associada. A lesão traumática secundária pode ser responsável por alterações nas estruturas apicais dos dentes. O ajuste oclusal pode favorecer o direcionamento das forças oclusais para o eixo longo dos elementos dentários.
Palavras-chave: Ajuste oclusal, oclusão dentária traumática, registro da relação maxilomandibular, oclusão.
INTRODUCTION
Understanding the relationship between dental occlusion and periodontal status is necessary for a correct diagnosis and for the establishment of restorative treatment in patients with periodontal disease.
Excessive occlusal forces, called traumatic occlusion, associated with bacterial plaque and microbial inflammation, can increase damage to periodontal structures and also cause damage to other elements of the stomatognathic system1-6. Traumatic occlusion may be caused by abrupt changes in occlusal forces, mechanical interference, disorders of neuromuscular origin, and bruxism1,2,7,8.
The presence of premature contacts, whether resulting from rehabilitation procedures or not, may lead to traumatic occlusion that causes damage to periodontal structures2,8-10. Common signs and symptoms include bone loss, loss of connective tissue insertion, mobility, increased periodontal space, thickening of the lamina dura, pulp symptoms, and pain1,2,7,10-12.
Periodontal tissues respond to increased occlusal forces by adaptive or degenerative changes1,2,7. Secondary occlusal trauma occurs when the ability of tissues to adapt to occlusal forces is compromised by bone loss resulting from periodontal inflammation1,2,7,8,12,13. The periodontium becomes more vulnerable to injury and to occlusal forces, and excessive occlusal forces lead to traumatic occlusion1,2.
CASE REPORT
A 35-year-old female patient presented at the Occlusion and Orofacial Pain Research Center at the School of Dentistry, Universidade Federal de Goiás, Goiânia, Brazil, with complaints of pain and mobility in the maxillary central incisors and sensitivity in the mandibular left incisors and canine.
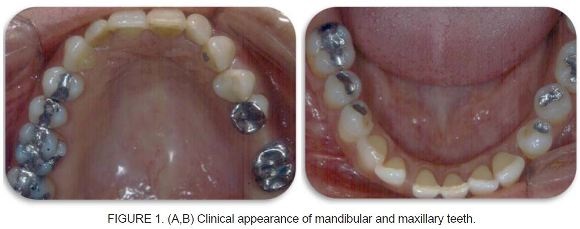
The patient reported that symptoms began after cast metal restoration (CMR) was performed in tooth #27 (Figure 1, A). Clinical examination revealed occlusal interference between teeth #27 and #37 (Figure 1, A and B). Occlusal contact promoted an increased vertical dimension of occlusion (VDO) and anterior projection of the mandible to the right. A 1-mm difference between the centric relation and habitual occlusion was observed, as well as grade II mobility and a periodontal pocket 5 mm deep in tooth #11. Mobility was also observed in the lower teeth, but at a lower degree.
Radiographic examination revealed vertical bone loss between teeth #21 and #11 (Figure 2), on the mesial side of tooth #33 (Figure 3), and between the lower
incisors (Figure 4). The lower teeth also showed radiolucent image suggestive of apical periodontitis. The pulp vitality test was positive. The clinical condition was associated with presence of bacterial plaque and marginal inflammation, rendering the periodontium more vulnerable to injury.



The patient underwent periodontal therapy (root scaling) and received guidance on oral hygiene. After starting periodontal therapy, a two-phase molding process was carried out using condensation silicone impression materials and a stock tray in the upper and lower arches. Casts were poured with special type IV improved dental stone and mounted on a semi-adjustable articulator (SAA). Thus, occlusal interference between teeth #27 and #37 and occlusal overload in the upper and lower incisors and canines, due to increased VDO, could be confi rmed. Occlusal adjustment by selective grinding was then indicated for the treatment of traumatic occlusion in order to promote an equal incidence of forces on all teeth.
Occlusal contacts were marked using a thin carbon articulating paper (Accufilm II) held by Miller clamping tweezers, noting the presence of interceptive contacts. High-speed carbide drills with a spherical-shaped tip were selected for carrying out the grinding. Twelve sessions were required to achieve a balanced occlusion and to reestablish physiological VDO.
The patient underwent only basic periodontal therapy, without using systemic medication, and occlusal adjustment by selective grinding for removal of occlusal interference and establishment of a balanced occlusion.
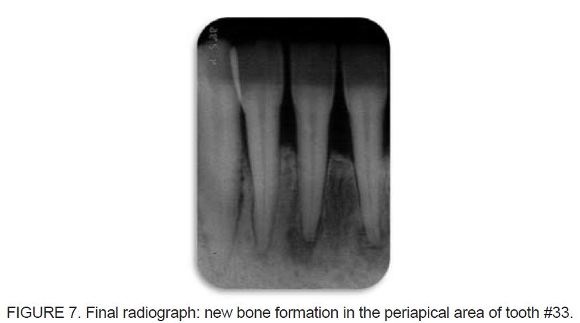
After 6 months the following outcomes were observed: a) newly formed bone tissue between teeth #11 and #21 (Figure 5); b) remission of radiolucent image suggestive of apical periodontitis in the lower teeth (Figure 6 and Figure 7); c) reduction of mobility; d) reduction of sensitivity in the lower teeth; e) centric relation coincident with habitual occlusion; f) greater patient comfort and balanced occlusion.
This study is part of a research protocol that was approved by the Local Ethics Committee (protocol no. 140/2003).


DISCUSSION
Mechanical interference promoted a change in the course of mandibular closure, leading one or more teeth to have abnormal occlusal contacts. The incorrect distribution of occlusal forces over the teeth led to increased bone loss, presence of root resorption, tooth mobility, and pain.
The relationship between occlusal trauma and periodontal health has been a subject of considerable debate and investigation. A healthy periodontium can withstand occlusal forces, thus avoiding the formation of periodontal pockets and/or gingivitis. However, the presence of inflammation caused by microbial plaque combined with traumatic occlusion leads to periodontal tissue destruction1-5,7. Occlusal trauma may develop when the intensity of the load exerted by occlusion exceeds the ability of the periodontium to resist and distribute the resulting forces1,2,7,12. Excessive occlusal load may cause changes in the periodontal ligament, alveolar bone, cementum, and dental pulp1-7,11-14.
Secondary trauma occurs when excessive occlusal forces cause damage to an already compromised periodontium, reducing periodontal attachment area and compromising the remaining tissues1,2,7,12. When there is occlusal balance, the occlusal forces occur in the axial direction and the periodontal tissues allow dental movement of approximately 0.12 to 0.25 mm inside the tooth socket. Changes in the direction of occlusal forces applied outside the long axis of the tooth cause pressure and tension on tissues, leading to injuries1,2,7.
Occlusal adjustment was indicated, because this technique can promote a harmonious relationship among the teeth, as well as with the neuromuscular mechanism, temporomandibular joints, and periodontal structures, by establishing acceptable standards8,9,15-22.
Removal of interference and the establishment of a balanced occlusion resulted in remission of periodontal injury (occlusal trauma) and remission of associated symptoms. However, initial removal of microbial plaque and inflammation by periodontal therapy was necessary, because treatment for occlusal trauma alone would not have been sufficient in the present case.
In the presence of occlusal trauma, occlusal adjustment is the treatment modality indicated. However, this treatment should be associated with periodontal therapy, for removal of microbial calcified plaque, and a strict oral hygiene program when this factor is also present. Secondary traumatic injury may be responsible for changes in apical tooth structures. Occlusal adjustment may favor the direction of occlusal forces to the long axis of the teeth.
REFERENCES
1. Lascala NT, Moussalli NH. Compendio Terapêutico Periodontal 2a ed. São Paulo: Artes Médicas; 1995. [ Links ]
2. Carranza FA. Periodontia Clínica. 9a ed. Rio de Janeiro: Guanabara Koogan; 2004. [ Links ]
3. Gher ME. Changing concepts. The effects of occlusion on periodontitis. Dent Clin North Am. 1998; 42(2): 285-299. [ Links ]
4. Harrel SK. Occlusal forces as a risk factor for periodontal disease. Periodontology 2000. 2006; 32: 111-117. [ Links ]
5. Pompei VC, Pacca CAA. Participação do Trauma Oclusal na Etiologia da Doença Periodontal. Rev Bras Odontol. 1988; 45(1): 48-50. [ Links ]
6. Silva Filho CE, Silva EMM. Periodontite – Traumatismo oclusal. Rev Bras Odontol. 1986; 43(5): 8-12.
7. Lindhe J. Tratado de Periodontia Clínica e Implantodontia Oral 3ª ed. Rio de Janeiro: Guanabara Koogan; 2004. [ Links ]
8. Paiva HJ. Oclusão; Noções e Conceitos Básicos 1ª ed: Santos, 1997. [ Links ]
9. Ash, Ramfjord, Schmidseder. Oclusão 2a ed: Santos; 2007. [ Links ]
10. Ishigaki S, Kurozumi T, Morishige E, Yatani H. Occlusal interference during mastication can cause pathological tooth mobility. J Periodont Res. 2006; 41: 189-192. [ Links ]
11. Harn WM, et al. Effect of occlusal trauma on healing of periapical pathoses: report of two cases. International Endodontic Journal. 2001; 34: 554-561. [ Links ]
12. Hallmon WH, Harrel SK. Occlusal analysis, diagnosis and management in the practice of periodontics. Periodontology. 2000; 34: 151-164. [ Links ]
13. Segura–Egea JJ, Jiménez–Rubio A, Velasco–Ortega, Ríos–Santos JV. Talon Cusp causing occlusal trauma and acute apical periodontitis: report of a case. Dental Traumatol. 2003; 19: 55-59.
14. Kumazawa, M., Kohsaka T, Yamasaki M, Nakamura H, Kameyama Y. Effect of traumatic occlusion on periapical lesions in rats. Journal of Endodontics. 1995; 21(7): 372-375. [ Links ]
15. Garcia AR. Fundamentos Teóricos e Práticos da Oclusão São Paulo: Cid Editora, 2003. [ Links ] 16. Scott WR. Application of “cusp writer” findings to practical and theoretical occlusal problems. Part I. J Prosthet Dentistry. 1976; 35(2): 211-221.
17. Au AR, Klineberg IJ. A new Approach for Accurate pre-planned occlusal adjustment. Aust Dental Journal. 1994; 39(1): 11-14. [ Links ]
18. Kerstein RB. Is patient Confirmation an Adequate Indicator of Occlusal Adjustment Completion? Dentistry Today. 1997; 16(10): 72-75. [ Links ]
19. McCullock AJ. Making Occlusion Work: 2. Practical Considerations. Dental Update. 2003; 30: 211-219. [ Links ]
20. Milosevic A. Occlusion 2: Occlusal splints, Analysis and Adjustment. Dental Update. 2003; 30; 416-422. [ Links ]
21. Gray HS. Occlusal adjustment: principles and practice. New Zealand Dental Journal. 1994; 90:13-19. [ Links ]
22. Selaimen CMP, et al. Occlusal Risk Factors for Temporomandibular Disorders. Angle Orthodontist. 2007; 77(3): 471-477. [ Links ]
 Corresponding Author:
Corresponding Author:
Professor Raulino Naves Borges
Faculdade de Odontologia – UFG
Av. Universitária Esquina com 1ª Avenida, s/nº, Setor Universitário, 3º andar Goiânia
CEP 74605-220 – Goiás – Brasil
E-mail:raulinonaves@hotmail.com













