Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.17 no.33 Canoas Jul./Dez. 2011
SCIENTIFIC ARTICLE
Occlusal adjustment in the treatment of primary traumatic injury
Equilíbrio oclusal no tratamento de injúria traumática primária
Raulino Naves Borges1; Bárbara Morais Arantes2; Denise Ferreira Vieira2; Orlando Aguirre Guedes3; Carlos Estrela4
1Professor of Dental Occlusion – UFGO, Goiânia, Brazil.
2Dental student, School of Dentistry – UFGO, Goiânia, Brazil.
3Post-graduate student – UFGO, Goiânia, Brazil.
4Chairman and Professor of Endodontics – UFGO, Goiânia, Brazil.
ABSTRACT
A major concern in dentistry is the correct distribution of occlusal forces to promote balance among the elements of the stomatognathic system. Occlusal trauma may develop in situations where the magnitude of the load exerted by occlusion exceeds the ability of the periodontium surrounding the involved teeth to resist and distribute the resulting forces without moving. A 41-year-old female patient was referred to the Occlusion and Orofacial Pain Research Center at the School of Dentistry, Universidade Federal de Goiás, Brazil, with headache, temporomandibular joint pain, toothache, and bone resorption on the distal aspect of tooth #33. During clinical examination, a 2-mm difference between centric relation and habitual occlusion was detected, with interference between teeth #28 and #38, causing anterior projection of the mandible to the right. Probing depth of the lower canine was within normal limits, with a positive pulp vitality test. We concluded that pain and (grade II) mobility in tooth #33 were caused by interference of third molars, which exerted a distal pressure on the lower canine, characterizing primary occlusal trauma. Occlusal adjustment by selective grinding was then indicated to eliminate premature contact. Ten sessions were required to obtain optimal occlusion. Three months after treatment, follow-up radiograph showed newly formed bone tissue between teeth #33 and #34, with absence of mobility and symptoms. The case reported here indicates that occlusal adjustment is recommended for the treatment of periodontal injuries caused by traumatic occlusion. The treatment allows the achievement of an optimal occlusion by directing occlusal forces to the long axis of the teeth.
Keywords: Occlusal adjustment, traumatic dental occlusion, maxillomandibular relation record, occlusion.
RESUMO
Uma das principais preocupações na odontologia é a distribuição correta das forças oclusais para que haja equilíbrio entre os elementos do complexo estomatognático. O trauma oclusal pode ocorrer quando a magnitude da carga exercida pela oclusão excede a capacidade do tecido periodontal ao redor dos elementos dentários envolvidos de resistir e distribuir as forças resultantes sem se mover. Uma paciente de 41 anos foi encaminhada ao Centro de Pesquisa em Oclusão e Dor Orofacial da Faculdade de Odontologia, Universidade Federal de Goiás, Brasil, com quadro clínico de cefaleia, dor nas articulações temporomandibulares, dor de dente e reabsorção óssea na face distal do dente 33. Ao exame clínico, detectou-se 2 mm de diferença entre a relação central e a oclusão habitual, com interferência entre os dentes 28 e 38, causando projeção mandibular anterior e para a direita. A profundidade de sondagem do canino inferior encontrava-se dentro dos limites normais, respondendo positivamente ao teste de vitalidade pulpar. Concluiu-se que a dor e a mobilidade (grau II) no dente 33 foram causadas por interferência existente entre os terceiros molares, fazendo com que o canino inferior fosse pressionado distalmente, caracterizando trauma oclusal primário. Para eliminar o contato prematuro, o tratamento indicado foi o ajuste oclusal por desgaste seletivo. Foram necessárias dez sessões para a obtenção de uma oclusão equilibrada. Após três meses de acompanhamento verificou-se ao exame radiográfico neoformação óssea entre os dentes 33 e 34, com desaparecimento da mobilidade e dos sintomas. O caso aqui relatado indica que o ajuste oclusal é recomendado para o tratamento de injúria periodontal causada por trauma oclusal. O tratamento permite atingir ótima oclusão ao direcionar as forças oclusais para o eixo longo dos elementos dentários.
Palavras-chave: Ajuste oclusal, oclusão dentária traumática, registro da relação maxilomandibular, oclusão.
INTRODUCTION
The health of the stomatognathic system depends mostly on the correct distribution of occlusal forces. Functional balance among all elements contributes to patient satisfaction with function and aesthetics. Changes in the direction of occlusal forces, i.e., the mismatch between the physiological and geometric axes of the tooth, create resultant vectors outside the long axis of the tooth. The more frequently an intermittent force is applied, the greater the damage to the periodontium. When occlusal forces exceed the adaptive capacity of the periodontal tissue, injury occurs, and this is called occlusal trauma1-4. The effect of these forces on the periodontium is influenced by their intensity, direction, duration, and frequency2.
Tissue damage associated with occlusal trauma can be divided into two types: primary and secondary. Primary trauma occurs in teeth with a normal periodontal structure, while secondary trauma is related to (normal or excessive) occlusal forces causing damage to an already compromised periodontium2-4.
In addition to periodontal injury, excessive occlusal forces may also affect the masticatory muscles, leading to muscle spasms and damage to the temporomandibular joint (TMJ) and dental tissues2,5,6.
This study aimed to discuss the strategy adopted for the treatment of a patient with a clinical diagnosis of primary occlusal trauma, associated with occlusal interferences, TMJ sensitivity and headache.
CASE REPORT
A 41-year-old female patient was referred to the Occlusion and Orofacial Pain Research Center at the School of Dentistry, Universidade Federal de Goiás, Goiânia, Brazil, with complaints of pain in tooth #33 and severe headache.
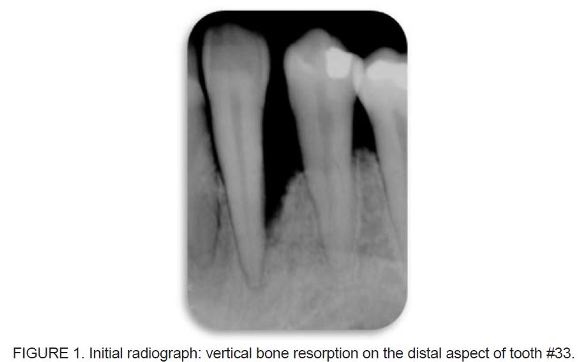
At the first visit, medical and dental history taking and clinical and radiographic examination were performed. TMJ and the following muscles were sensitive to palpation: inferior lateral pterygoid, temporal, left masseter, left medial pterygoid, and left sphenomandibular. A 2-mm difference between the centric relation (CR) and habitual occlusion (HO) was observed. Clinical examination of the lower left canine (tooth #33) revealed grade II mobility, probing depth within normal limits, and a positive pulp vitality test. Radiographic examination detected extensive vertical bone resorption on the distal aspect of tooth #33, thus confirming mobility (Figure 1). The absence of tooth #36 resulted in the mesial movement of teeth #37 and #38, causing the extrusion of tooth #28 and leading to an increased vertical dimension of occlusion (VDO) in CR. Evaluation of mandibular dynamics revealed occlusal interference between teeth #28 and #38 (Figure 2), causing anterior projection of the mandible to the right. As a result, tooth #33 in HO was pushed distally due to forced contact with the upper tooth, causing occlusal trauma and consequent vertical bone resorption on the distal aspect of tooth #33 (Figure 1).

A two-phase molding process was carried out using condensation silicone impression materials and a stock tray in the upper and lower arches. Casts were poured with type IV improved dental stone and mounted on a semi-adjustable articulator (SAA) in the CR position. Thus, it was possible to confirm occlusal interference between teeth #28 and #38, increased VDO, and occlusal overload in the lower left canine.
Treatment was initiated with removal of occlusal interference through occlusal adjustment by selective grinding in CR. Occlusal contacts were marked using a thin carbon articulating paper (Accufi lm II) held by Miller clamping tweezers, noting the presence of interceptive or deflective contacts. High-speed carbide drills with a spherical-shaped tip were selected for carrying out the grinding. Ten sessions were required to achieve a balanced occlusion. There was remission of muscle and TMJ symptoms and headache. Tooth #33 showed an improvement in mobility within 3 months of treatment (Figure 3). After 6 months, all symptoms, including pain and mobility, were no longer present. During this 6-month period, there was radiographic evidence of bone healing on the distal aspect of tooth #33 (Figure 4). This study is part of a research protocol that was approved by the Local Ethics Committee (protocol no. 140/2003).


DISCUSSION
The influence of occlusal factors on injuries to the various elements of the stomatognathic system, such as muscles, TMJ, teeth, and periodontal structures, should be thoroughly studied. Under nonpathological conditions, the periodontal structures would absorb incident forces in the axial direction. However, a change in the direction of these forces would be detrimental, because horizontal loads are not well supported by the periodontium.
Occlusal trauma occurs due to interference, as interference leads to an increased VDO. This type of injury is the result of occlusal forces applied outside the long axis of the tooth and is called traumatic occlusion2-6. Bone resorption is often observed as a result of trauma.
Tissue injury associated with occlusal trauma is divided into primary and secondary trauma. The primary form occurs when tissue reactions affect teeth with a normal periodontium, while the secondary form is related to damage to an already compromised periodontium with reduced height1-4,7-9. Any type of occlusal interference may cause abnormal muscle activity. Muscle hyperactivity can characterize damage to muscles, as their normal function is disrupted, causing pain and tenderness1,10,11, as in the case reported here.
During the functional course of mandibular closure, mechanical interference may cause a deviation in the movement of the mandible, leading one or more teeth to have abnormal occlusal contacts, causing detrimental effects on periodontal structures. In some cases, incorrect tooth positioning causes the teeth to receive all occlusal forces, thus being predisposed to changes in their supporting structures5,8,10,11. Abnormal muscle activity can cause traumatic/painful injury to joint structures. Other damage caused by traumatic occlusion occurs in the dental pulp. Several studies have reported the occurrence of pulp calcification and pulp necrosis when occlusal forces continue to act in a degenerative manner2,6,12,13. The periodontal tissues respond to this increase in occlusal force by adaptive or degenerative changes, which are reversible when the trauma is removed. The effect of occlusal forces on the periodontium is influenced by their direction, duration, and frequency.
Repair occurs when occlusal forces are reduced or the tooth is moved away from them. If these forces continue to act in a chronic fashion, tissues remodel to better absorb the impact. This fact results in changes in the periodontal ligament, alveolar bone, cementum and dental pulp, periapical inflammation, and root resorption1-9,13-16. The periodontium may also become more resistant to withstand the conditions created. The consequences of this phenomenon can be seen at the tooth level, leading to the formation of wear facets, severe attrition of the occlusal surfaces, and even tooth fractures1.
Occlusal adjustment by selective grinding was indicated, because this technique can promote an equal incidence of all forces on the teeth, which causes the physiological and geometric axes to match, thus establishing a harmonious relationship among the elements of the stomatognathic system through the elimination of occlusal interferences17-24.
Removal of interference and the establishment of a balanced occlusion resulted in reversal of periodontal injury (traumatic occlusion) and remission of all symptoms.
FINAL CONSIDERATIONS
The correct diagnosis of primary occlusal trauma allows treatment with occlusal adjustment.
REFERENCES
1. Lascala NT, Moussalli NH. Compendio Terapêutico Periodontal 2a ed. São Paulo: Artes Médicas; 1995. [ Links ]
2. Carranza FA. Periodontia Clínica. 9a ed. Rio de Janeiro: Guanabara Koogan; 2004. [ Links ]
3. Hallmon WH, Harrel SK. Occlusal analysis, diagnosis and management in the practice of periodontics. Periodontology. 2000; 34: 151-164. [ Links ]
4. Lindhe J. Tratado de Periodontia Clínica e Implantodontia Oral 3ª ed. Rio de Janeiro: Guanabara Koogan; 2004. [ Links ]
5. Paiva HJ. Oclusão; Noções e Conceitos Básicos 1ª ed: Santos, 1997. [ Links ]
6. Harn WM et al. Effect of occlusal trauma on healing of periapical pathoses: report of two cases. International Endodontic Journal. 2001; 34: 554-561. [ Links ]
7. Gher ME. Changing concepts. The effects of occlusion on periodontitis. Dent Clin North Am. 1998; 42(2): 285-299. [ Links ]
8. Ishigaki S, Kurozumi T, Morishige E, Yatani H. Occlusal interference during mastication can cause pathological tooth mobility. J Periodont Res. 2006; 41: 189-192. [ Links ]
9. Segura–Egea JJ, Jiménez–Rubio A, Velasco–Ortega e, Ríos–Santos JV. Talon Cusp causing occlusal trauma and acute apical periodontitis: report of a case. Dental Traumatol. 2003; 19: 55-59.
10. Ash, Ramfjord, Schmidseder. Oclusão 2a ed: Santos; 2007. [ Links ]
11. Garcia AR. Fundamentos Teóricos e Práticos da Oclusão São Paulo: Cid Editora, 2003. [ Links ]
12. Harrel SK. Occlusal forces as a risk factor for periodontal disease. Periodontology 2000. 2006; 32: 111-117. [ Links ]
13. Kumazawa, M., Kohsaka T, Yamasaki M, Nakamura H, Kameyama Y. Effect of traumatic occlusion on periapical lesions in rats. Journal of Endodontics. 1995; 21(7): 372-375. [ Links ]
14. Silva Filho CE, Silva EMM. Periodontite – Traumatismo oclusal. Rev Bras Odontol. 1986; 43(5): 8-12.
15. Scott WR. Application of “cusp writer” findings to practical and theoretical occlusal problems. Part I. J Prosthet Dentistry. 1976; 35(2): 211-221.
16. Pompei VC, Pacca CAA. Participação do Trauma Oclusal na Etiologia da Doença Periodontal. Rev Bras Odontol. 1988; 45(1): 48-50. [ Links ]
17. Gray HS. Occlusal adjustment: principles and practice. New Zealand Dental Journal. 1994; 90:13-19. [ Links ]
18. Bailey JO. Occlusal Adjustment. Dent Clin North Am.1995; 39(2): 441-458. [ Links ]
19. Selaimen CMP, et al. Occlusal Risk Factors for Temporomandibular Disorders. Angle Orthodontist. 2007; 77(3): 471-477. [ Links ]
20. Au AR, Klineberg IJ. A new Approach for Accurate pre-planned occlusal adjustment. Aust Dental Journal. 1994; 39(1): 11-14. [ Links ]
21. Ash Jr M, Ward ML. Occlusal Adjustment: Quo Vadi? The Journal of Craniomandibular Practice. 2003; 21(1): 1-4. [ Links ]
22. Milosevic A. Occlusion 2: Occlusal splints, Analysis and Adjustment. Dental Update. 2003; 30; 416-422. [ Links ]
23. Kerstein RB. Is patient Confirmation an Adequate Indicator of Occlusal Adjustment Completion? Dentistry Today. 1997; 16(10): 72-75. [ Links ]
24. McCullock AJ. Making Occlusion Work: 2. Practical Considerations. Dental Update. 2003; 30: 211-219. [ Links ]
 Corresponding Author:
Corresponding Author:
Professor Raulino Naves Borges
Faculdade de Odontologia – UFG
Av. Universitária Esquina com 1ª Avenida, s/nº, Setor Universitário, 3º andar
CEP 74605–220 – Goiânia – Goiás – Brasil
Tel./fax: +55 (54) 3313.3925
E-mail:raulinonaves@hotmail.com













