Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.18 no.35 Canoas Jul./Dez. 2012
SCIENTIFIC ARTICLE
Diagnostic and treatment features of keratocystic odontogenic tumors
Particularidades do diagnóstico e tratamento do tumor odontogênico queratocístico
Guilherme Romano Scartezini1; Guilherme Costa Oliveira2; Orlando Aguirre Guedes3; Daniel Almeida Decurcio3; Artur Aburad de Carvalhosa4; Carlos Estrela5
1Graduate student in Health Sciences at Federal University of Goiás, Goiânia, GO, Brazil.
2Graduate student at the Dental School of Federal University of Goiás, Goiânia, GO, Brazil.
3Professor of Endodontics at the Brazilian at the Dental Association, Goiânia, GO, Brazil.
4Professor of Oral Pathology at the Dental School of University of Cuiabá, Cuiabá, MT, Brazil.
5Chairman and professor of Endodontics at the Dental School of Federal University of Goiás, Goiânia, GO, Brazil.
ABSTRACT
Keratocystic odontogenic tumors (KCOT) comprise a unique pathological entity characterized by aggressive/destructive behavior and propensity to recurrence. This study describes the diagnostic and treatment features of a KCOT lesion. A 22-year old man was referred for surgical treatment of pericoronitis on tooth no. 37. Panoramic radiography revealed a unilocular, large radiolucent area extending from tooth no. 36 to the left mandibular ramus. Aspiration and incisional biopsy were performed, and the tissue sample was sent for microscopic evaluation. Microscopically, a cystic lesion was observed, lined by keratinized squamous epithelium and filled with keratin lamellae, confirming the diagnosis of KCOT. Surgery was performed in an outpatient setting and involved osteotomy, detachment of the cystic lesion, and removal of teeth no. 36, 37, and 38. The patient was clinically and radiographically followed for 12 months, and no evidence of recurrence was observed. KCOTs should be considered in the differential diagnosis of lesions affecting the posterior region of the mandible. Accurate clinical, radiographic, and microscopic examinations are essential to establish the definitive diagnosis and choose the most effective therapy.
Keywords: Keratocystic odontogenic tumor, odontogenic keratocyst, oral neoplasms.
RESUMO
O tumor odontogênico queratocístico (TOQ) é uma entidade patológica singular, devido ao seu comportamento agressivo/destrutivo e à sua propensão a recorrências. O presente trabalho descreve as particularidades de diagnóstico e tratamento de um TOQ. Um paciente do sexo masculino, com 22 anos de idade, foi encaminhado para tratamento cirúrgico de pericoronarite no dente 37. O exame radiográfico panorâmico revelou uma área ampla, unilocular, estendendo-se do dente 36 até o ramo esquerdo da mandíbula. Punção óssea aspirativa e biópsia incisional foram realizadas, e a amostra de tecido foi encaminhada para análise microscópica. Microscopicamente, observou-se lesão cística, revestida por epitélio escamoso queratinizado e preenchida por lamelas de queratina, confirmando o diagnóstico de TOQ. O procedimento cirúrgico foi realizado em ambiente ambulatorial e envolveu osteotomia, descolamento da luz da lesão e exodontia dos dentes 36, 37 e 38. O paciente foi acompanhado clínica e radiograficamente por um período de 12 meses, e não foi observada recorrência da lesão. O TOQ deve ser considerado no diagnóstico diferencial de alterações da região posterior da mandíbula. Exames clínicos, radiográficos e microscópicos precisos são essenciais no estabelecimento do diagnóstico e na escolha da modalidade terapêutica mais eficaz.
Palavras-chave: Tumor odontogênico queratocístico, queratocisto odontogênico, neoplasias orais.
INTRODUCTION
Odontogenic keratocysts, recently reclassified as keratocystic odontogenic tumors (KCOTs)1, are among the most controversial and frequent pathological entities affecting the maxillofacial region2-4. Their aggressive/destructive behavior and proneness to recurrence have led the condition to be classified as a benign neoplasm, in spite of actually being a simple cystic lesion5.
KCOTs are twice more frequent in the mandible than in the maxilla6,7. Their main clinical manifestations are swelling and/or pain, even though some asymptomatic cases have also been reported8-10. Radiographically, KCOTs present non-pathognomonic features2,9,10: they may appear as small or large, round or ovoid radiolucent lesions, often with scalloped, multilobulated, distinct margins. Involvement of an impacted tooth has been reported in 25 to 40% of cases6,7.
Histopathologically, KCOTs present some distinguishing features compared with other odontogenic tumors. The epithelium may show budding of the basal layer into underlying connective tissue, with formation of detached microcysts, termed daughter cysts2. Treatment remains controversial, and different approaches have been reported in the literature11. As a conservative method, simple enucleation with or without curettage and marsupialization can be performed. More aggressive methods include peripheral osteotomy, chemical curettage with Carnoy’s solution, and resection8,12.
The present article describes the case of a 22-year old man who presented with a KCOT involving teeth no. 36, 37, and 38. Diagnosis and treatment features are discussed.
CASE REPORT
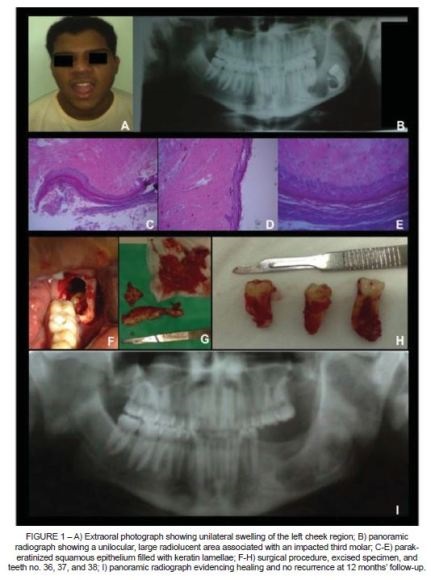
A 22-year old male patient of African descent was referred to the Department of Oral and Maxillofacial Surgery of the Municipal Health Department of Goiânia, state of Goiás, Brazil, in December 2008, for surgical treatment of pericoronitis on tooth no. 37. Patient medical history was negative for other conditions, except for allergy to sodium dipyrone. Oral examination revealed unilateral swelling of the left cheek region, of hard consistency, with no point of fluctuation, presence of purulent discharge, citric yellow in color, on the distal surface of tooth no. 37, and no eruption of tooth no. 38. There were no spontaneous complaints (Figure 1A).
Panoramic radiography revealed a unilocular, large radiolucent area extending from the mesial surface of the distal root of tooth no. 36 to the left mandibular ramus. Tooth no. 38 was completely involved in the radiolucent lesion and displaced into the left mandibular ramus. No root resorption was noted (Figure 1B). The patient underwent aspiration, incisional biopsy, and histological examination. The latter revealed a cystic lesion, lined by keratinized squamous epithelium and filled with keratin lamellae (Figure 1C-E), confirming the diagnostic hypothesis of KCOT.
The surgical procedure was performed in an outpatient setting under local anesthesia with no sedation. Preventive drug therapy with 875 mg amoxicillin/ clavulanic acid combined with 750 mg paracetamol and 100 mg nimesulide was administered 1 hour before surgery. An incision was made along the left mandibular ramus, and a mucoperiosteal flap was raised, with intrasulcular extension to teeth no. 36 and 37. Osteotomy was performed using a 701 bur attached to a high-speed handpiece, with subsequent exposure of the cystic lesion, which was then detached until the region of the coronoid process and left mandibular condyle. Thereafter, teeth no. 36, 37, and 38 were removed to avoid condylar base fractures (Figure 1FH). Occlusion sutures were made using 4.0 nylon monofilament, and the patient was instructed to keep the medication in the postoperative period (10 days). The patient was followed for 12 months and underwent clinical and radiographic examinations every visit. The healing process was satisfactory, with no evidence of recurrence throughout the follow-up period (Figure 1 I).
DISCUSSION
Odontogenic tumors comprise a rare group of lesions derived from the toothforming apparatus6. Among odontogenic tumors, KCOTs are the second most frequently diagnosed lesion, with reported prevalence rates ranging from 19 to 38%3. KCOTs are of great interest in clinical practice and require special attention due to their specific histopathological features, aggressive and infiltrative behavior, and tendency to recurrence2,11.
KCOTs are usually observed in patients aged 10-29 years and show a slight preference for men7,9,13,14. Lesions are mostly located in the mandible, especially in the posterior portion of the mandible and in the mandibular ramus, and are generally related with unerupted teeth6,7,9,10,13,14. In our case, a KCOT was diagnosed in a 22-year old man of African descent, and it involved the root apex of teeth no. 36 and 37, in addition to unerupted tooth no. 38.
Patients with KCOTs may present various symptoms and features, e.g. swelling, pain, discharge, aggressive growth, invasion of adjacent structures, and recurrence10,13. Myoung et al.13 reviewed 256 cases of KCOT and observed that the most frequent clinical manifestations upon admission were swelling, pain, or a combination of both (82.4% of all cases). Conversely, Boffano et al.14 reported that 62.8% of patients with KCOTs had no symptoms. It is important to note that KCOTs can be easily mistaken for inflammatory lesions, as patients usually show typically inflammatory symptoms, such as pain, swelling, and discharge15. In our case, the patient did not spontaneously complain of pain, and was initially referred for surgical treatment of pericoronitis on tooth no. 37.
Conventional radiographic examinations such as panoramic and intraoral periapical radiographs are usually adequate to determine the location and estimate the size of a KCOT7. Radiographically, most KCOTs present as a unilocular or multilocular wellcircumscribed radiolucent lesion with smooth or scalloped margins and sclerotic borders9,10,14. Because these radiological features are non-pathognomonic2, differential diagnosis should include dentigerous cysts, ameloblastomas, radicular cysts, simple bone cysts, central giant cell granulomas, arteriovenous malformations, and fibro-osseous lesions16,17. According to Güller et al.7, one radiographic feature suggestive of KCOT is lesion growth in an anterior-posterior direction within the medullary cavity, with no obvious bone expansion.
Histologically, KCOTs present the following features: presence of a well defined, often palisaded, basal layer consisting of columnar or cuboidal cells; intensely basophilic nuclei of columnar basal cells oriented away from the basement membrane; parakeratotic layers, often with a corrugated surface; and mitotic figures frequently present in suprabasal layers1. Some authors have classified KCOTs into parakeratotic and orthokeratotic subtypes18, according to immunohistochemical and histologic features of the lining and the type of keratin produced9,19. The parakeratotic type accounts for the majority of KCOTs (83 to 97%)9 and has a greater potential for local destruction and extension into adjacent tissues, rapid growth, recurrence, and multiplicity7. The lesion identified in our case was a parakeratotic KCOT.
The treatment of KCOTs remains a controversial topic, and several treatment options are currently available, including decompression, curettage, marsupialization, enucleation, and resection2,11,14,19. Johnson et al.11 have conducted a review of the literature to provide an updated overview of the management and recurrence rates of KCOTs. Of the 2,736 articles retrieved by the authors, only eight met the inclusion criteria. In addition, because of a large number of variables assessed and the absence of randomized controlled trials available on the topic, a meta-analytic approach could not be used to analyze results. According to Maurette et al.19, conservative treatment of KCOTs has important advantages: it is less traumatic for the patient, eliminates the need for medication, reduces hospitalization costs, and avoids the need for reconstruction using grafts or other bone extension methods. In our case, the KCOT was treated with enucleation associated with curettage, a conservative and effective treatment option. Healing was satisfactory, with no evidence of recurrence over the follow-up period.
In conclusion, KCOTs are benign uni- or multicystic intraosseous tumors of odontogenic origin and should be considered in the differential diagnosis of jaw lesions. Notwithstanding, even in the presence of clinical and radiological features indicative of KCOT, a definitive diagnosis cannot be made without microscopic analysis. Only a detailed investigation will allow to determine the most effective treatment and thus to avoid recurrences.
REFERENCES
1. Barnes L, Evenson J, Reichart P, Sidransky D. Word Health Organization classification of tumors. Pathology and genetics of head and neck tumors. Lyon: IARC Press; 2005. [ Links ]
2. Mendes RA, Carvalho JF, van der Waal I. Characterization and management of the keratocystic odontogenic tumor in relation to its histopathological and biological features. Oral Oncol. 2010;46:219-25. [ Links ]
3. Osterne RL, Brito RG, Alves AP, Cavalcante RB, Sousa FB. Odontogenic tumors: a 5-year retrospective study in a Brazilian population and analysis of 3406 cases reported in the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:474-81. [ Links ]
4. Costa DOP, Maurício AS, Faria PA, Silva LE, Mosqueda-Taylor A, Lourenço SQ. Odontogenic tumors: a retrospective study of four Brazilian diagnostic pathology centers. Med Oral Patol Oral Cir Bucal. 2012;17:e389-94. [ Links ]
5. Shear M. The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behavior. Oral Oncol. 2002;38:219-26. [ Links ]
6. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia: Saunders; 2002. [ Links ]
7. Güler N, Sençift K, Demirkol Ö. Conservative management of keratocystic odontogenic tumors of jaws. ScientificWorldJournal. 2012;2012:680397. doi: 10.1100/2012/680397. Epub 2012 Feb 14. [ Links ]
8. Hyun HK, Hong SD, Kim JW. Recurrent keratocystic odontogenic tumor in the mandible: a case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e7-10. [ Links ]
9. MacDonald-Jankowski DS. Keratocystic odontogenic tumour: systematic review. Dentomaxillofac Radiol. 2011;40:1-23. [ Links ]
10. Titinchi F, Nortje CJ. Keratocystic odontogenic tumor: a recurrence analysis of clinical and radiographic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:136-42. [ Links ]
11. Johnson NR, Batstone MD, Savage NW. Management and recurrence of keratocystic odontogenic tumor: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Jul 6. [Epub ahead of print] [ Links ].
12. Pitak-Arnnop P, Chaine A, Oprean N, Dhanuthai K, Bertrand JC, Bertolus C. Management of odontogenic keratocysts of the jaws: a ten-year experience with 120 consecutive lesions. J Craniomaxillofac Surg. 2009;38:358-64. [ Links ]
13. Myoung H, Hong S-P, Hong S-D, Lee J-I, Lim C-Y, Choung P-H, Lee J-H, Choi J-Y, Seo B-M, Kim M-J. Odontogenic keratocyst: review of 256 cases for recurrence and clinicopathologic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:328-33. [ Links ]
14. Boffano P, Ruga E, Gallesio C. Keratocystic odontogenic tumor (odontogenic keratocyst): preliminary retrospective review of epidemiologic, clinical, and radiological features of 261 lesions from university of Turin. J Oral Maxillofac Surg. 2010;68:2994-9. [ Links ]
15. Tsukamoto G, Sasaki A, Akiyama T, Ishikawa T, Kishimoto K, Nishiyama A, Matsumura T. A radiologic analysis of dentigerous cysts and odontogenic keratocysts associated with a mandibular third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:743-7. [ Links ]
16. Garlock JA, Pringle GA, Hicks ML. The odontogenic keratocyst: a potential endodontic misdiagnosing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:452-6. [ Links ]
17. Meara JG, Shah S, Li KK, Cunningham MJ. The odontogenic keratocyst: a 20-year clinicopathologic review. Laryngoscope. 1998;108:280-3. [ Links ]
18. da Silva MJ, de Sousa SO, Corrêa L, Carvalhosa AA, De Araújo VC. Immunohistochemical study of the orthokeratinized odontogenic cyst: a comparison with the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:732-7.
19. Maurette PE, Jorge J, Moraes M. Conservative treatment protocol of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg. 2006;64:379-83. [ Links ]
 Corresponding Author:
Corresponding Author:
Guilherme Romano Scartezini
Department of Stomatological Sciences
Federal University of Goiás
Praça Universitária s/ no., Setor Universitário
CEP 74605-220 – Goiânia, GO, Brazil
E-mail:g_scartezini@yahoo.com.br













