Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.18 no.35 Canoas Jul./Dez. 2012
SCIENTIFIC ARTICLE
Relationship between sphenomandibular muscle hyperactivity and visual symptoms
Estudo da relação entre hiperatividade dos músculos esfenomandibulares e sintomatologia visual
Raulino Naves Borges1; Marcos Ávila2
1Professor of Dental Occlusion, Federal University of Goiás, Goiânia, GO, Brazil.
2Professor of Ophthalmology, Federal University of Goiás, Goiânia, GO, Brazil.
ABSTRACT
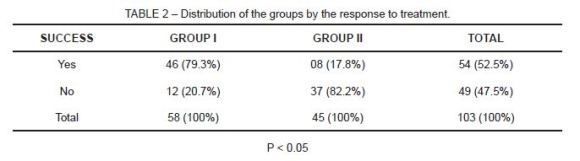
This was an observational, descriptive study developed after an anatomical investigation of cadavers to identify the sphenomandibular muscle as an independent entity. The objective here was to perform a clinical and interpretative evaluation of the physiological relationships between the functions of the sphenomandibular muscle and various symptoms, thereby associating temporomandibular disorders with ocular pain. Ten anatomical sets (five cadavers) in the Department of Anatomy of the Medicine School of the Catholic University of Goiás were examined. This study was conducted between April, 2006 and December, 2008. Patients (181 subjects) suffering from temporomandibular disorder were treated in the Federal University of Goiás Dental School. Two groups were compared: Group I consisted of 58 patients with temporomandibular disorder, referred ocular pain, and hyperactivity of the sphenomandibular muscles; Group II was comprised of 45 patients with temporomandibular disorder, ocular pain, but no hyperactivity of the sphenomandibular muscles. After a clinical exam, treatments were conducted with semi-yearly follow-up exams for 2 years. Responses to the treatment were evaluated by questionnaires thereby quantifying existing levels of ocular pain. Pain was eliminated in 46 of the 58 patients in Group I (79.31%) and 8 of the 45 patients in Group II (17.77%). Our evaluation affirms that the sphenomandibular muscle, independent of the temporal muscle, has an intimate relationship with the orbit. The clinical exam allowed an evaluation of the sphenomandibular muscles in temporomandibular disorder episodes. The hyperactivity of the sphenomandibular muscle is thus significantly related to the presence of ocular-referred pain (p<0.05).
Keywords: Temporomandibular disorder, sphenomandibular muscle, referred pain.
RESUMO
Estudo observacional e descritivo desenvolvido após estudo anatômico feito em cadáveres para a identificação do músculo esfenomandibular como entidade independente. Pretendeuse uma avaliação clínica interpretativa das relações fisiológicas entre as funções do músculo esfenomandibular e a sintomatologia que envolve desordem temporomandibular com dor ocular. Foram examinados 10 conjuntos anatômicos (cinco cadáveres) no Departamento de Anatomia da Faculdade de Medicina da Pontifícia Universidade Católica de Goiás. Além disso, foram tratados e acompanhados 181 pacientes atendidos no Ambulatório da Faculdade de Odontologia da Universidade Federal de Goiás, portadores de Desordem Temporomandibular. O trabalho foi desenvolvido entre abril de 2006 e dezembro de 2008. Foram comparados: o Grupo I, de 58 pacientes que apresentavam desordem temporomandibular, dor ocular reflexa e hiperatividade dos músculos esfenomandibulares; e o Grupo II, composto de 45 pacientes que apresentavam a desordem, dor ocular e não apresentavam hiperatividade dos músculos esfenomandibulares. O tratamento foi realizado após exame clínico com acompanhamento durante 2 anos, em avaliações semestrais. A resposta ao tratamento foi avaliada mediante questionário de opinião que estratifica o nível da dor ocular. A dor foi eliminada em 46 dos 58 pacientes do Grupo I (79,31%) e em 8 dos 45 pacientes do Grupo II (17,77%). O resultado da avaliação permite afi rmar que o músculo esfenomandibular, músculo independente do temporal, está em íntima relação com a órbita. O exame clínico permitiu a avaliação da hiperatividade dos músculos esfenomandibulares nos episódios de desordens temporomandibulares. A hiperatividade dos músculos esfenomandibulares está significativamente associada à presença de dor ocular reflexa (p < 0,05).
Palavras-chave: Desordem temporomandibular, músculo esfenomandibular, dor referida.
INTRODUCTION
Temporomandibular disorder (TMD) is a pathological condition of multifactorial origins1. Its participation in the signal and symptoms in one or more structures of the stomatognathic system is well documented2,3. This disorder might also affect organs outside the referred system4-6.
Headache is related to a TMD (more frequently the tensional type)7,8. An association between TMD, otalgia, and other auditory symptoms (such as discriminative difficulty, buzz, and other sounds) is also well established2,5.
The present study reveals the participation of TMD, with one or both sphenomandibular muscles in hyperactive state, in ophthalmological problems expressed by referred ocular pain.
After drawing the topography of the sphenomandibular muscles, now considered to be independent entities, the study’s objective was to associate the hyperactivity expressed in the sphenomandibular muscles with the presence of referred ocular pain.
METHODOLOGY
A study specifically designed to spatially map the sphenomandibular muscles preceded the development of the present proposition. The independence of the sphenomandibular muscles was determined by dissecting cadavers and then drawing the muscles’ origins and insertions while pointing out their correlation with the eyeball. This study is described in detail in another article9.
Based upon the information gathered from the above activities, clinical examinations, treatment, and follow-up were conducted with patients having TMD and visual symptoms. The clinical evaluation (anamnesis and physical examination) was performed by the investigator and complementary exams were carried out when needed.
After anamnesis, the physical exam evaluated all mastication muscles. Any hyperactivity of the sphenomandibular muscle was examined by digital palpation applying approximately 450 grams of pressure for intraoral muscles and temporomandibular joints (TMJs) and 900 grams for the extraoral palpated muscles, following the recommendations of Zarb et al.10 and Paiva et al.11.
A routine for assessing the mastication muscles was established beginning on the right side with the masseter, inferior lateral pterygoid, superior lateral pterygoid, medial pterygoid, sphenomandibular, and, finally, the temporal muscle (sequentially: anterior beam, medium beam, and posterior beam). The same routine was followed for the left side.
During the palpation of the sphenomandibular muscle, the patient was requested to quantify their level of pain from 0 to 3 points using a scale in which zero was equivalent to a sphenomandibular muscle insensitive to palpation, one indicating a light sensitivity, two representing a moderate level, and three signifying a severe sensitivity.
The inclusion criterion for the studied group was the presence of TMD followed by referred ocular pain, with or without hyperactivity of the sphenomandibular muscles. All patients were treated following identification of the etiological factor for a TMD. When the patients presented hyperactivity in one or both sphenomandibular muscles and also referred ocular pain, they were assigned to Group I. Group II was composed of patients who had TMD as well as the ocular symptom under scrutiny, but who also did not present hyperactivity of the sphenomandibular muscles.
During the physical exam the TMJs were also evaluated in an effort to reveal any symptoms of disease inherent to the TMJs – either local or systemic. Occlusal harmony was also evaluated.
During the physical examination, cross-matching of the findings with anamnesis data was tested, such as (for example) the presence of an ocular symptom with the sensitivity to palpation of the sphenomandibular muscles, the side affected by ocular symptoms and by sphenomandibular muscle hyperactivity, or an association between hyperactivity of one or both mastication muscles and spasms or headache.
This study was developed in the Dental School of the Federal University of Goiás, from April, 2006 to December, 2008. The sample was submitted to treatment for 2 years with followed-ups every 6 months, thus adhering to the same evaluation routine cited above, and registering, each time, all levels of patient ocular pain. From all registered information, a database was compiled thereby allowing the evaluation of this study proposition.
RESULTS
One hundred and one patients treated for TMD in the Clinic of the Dental School of the Federal University of Goiás were evaluated. The 100 patients who presented with TMD, hyperactive sphenomandibular muscles, and referred ocular pain were assigned to Group I. Group II was comprised of the 81 patients who exhibited TMD and related ocular pain, but without hyperactivity of the sphenomandibular muscles.
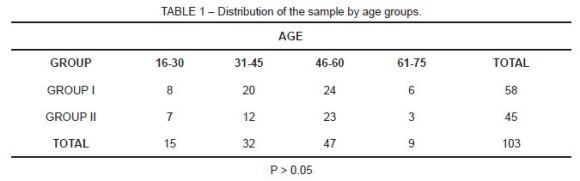
After 2 years of the proposed treatment, 42 patients were excluded from Group I and 36 patients from Group II, for they did not conclude the treatment or did not meet the periodic evaluation requirement. The present analysis was therefore performed on a sample of 103 patients (58 from Group I and 45 from Group II) whose age varied from 15 to 76 years (Table 1). Between groups, there was no significant statistical difference between the patients’ ages, no matter which cut-off point was used to make the evaluation (p > 0.05).
After the treatment period, 46 of the 58 patients from Group I (79.31%) indicated an absence of referred ocular pain, while only 8 of the 45 patients from Group II recognized relief in the ocular symptoms mentioned during their first appointment (Table 2). The difference in results between the 2 groups is statistically significant (p < 0.05).
DISCUSSION
For some time the sphenomandibular muscle was considered the deepest portion of the temporal muscle12-16 and was confused with the medial pterygoid or the temporal muscle15. But in 1994 Koritzer16 described its origin as being the osseous complex, zygomatic/frontal, in the posterior portion of the orbit, having as its limit the superior wall of the infratemporal fossa16. This muscle is now being described as an independent entity12,16-23.
A study having its origin in the dissection of human cadavers, intentionally completed previous to this study9, demonstrated that the sphenomandibular muscle has its origin in the region made up of the zygomatic portion of the frontal bone and the frontal portion of the zygomatic bone – thus in the lateral face of the orbit. The muscle describes a slight distal inclination to the edge of the anterior margin of the anterior beam of the temporal muscle and is separated from this by a fascia. The sphenomandibular muscle inserts, in an external oblique line, into the mandible, thereby gathering all the anterior margin of the coronoid process into the branch of the mandible. This muscle has a superficial origin, overlapping the fibers of the anterior beam of the temporal muscle.
The anatomical location of the sphenomandibular muscle, anterior to the temporal muscle and lateral to the orbit, deserves special emphasis in the present study, since it frequently presents hyperactivity during TMDs, not uncommonly concomitant with complaints of alterations in vision and pain in the area of the ocular region15,17,19. Complaints of ocular pain by patients with TMD justify the present study, which proposed to search out a possible association between TMDs and the ophthalmologic alteration initiated by hyperactivity of the sphenomandibular muscle.
This study began with the hypothesis that hyperactivity of the sphenomandibular muscle might be associated with ocular pain. Confirmation of this hypothesis may help the medical practitioner (especially ophthalmologists) as an auxiliary tool in the diagnosis and treatment of their patients.
Although not specifically mentioning the sphenomandibular muscle, Pereira et al. (24) asserted that treatment of TMD eliminates ocular symptoms. They believed that the pain might be an etiologic factor of the ocular symptoms, since a deep and constant pain generates an excitatory central effect4,10.
The present study proposed to demonstrate that removing the hyperactivity of the sphenomandibular muscle eliminates the ocular pain. Thus, the treatment of patients was designed to remove the hyperactivity arising from TMDs by eliminating their cause.
The results of our evaluation after 2 years of treatment show a significant difference observable in the quantified experience of the ocular pain after removing the symptoms of muscle hyperactivity (p < 0.05).
The proximity between the orbit and the sphenomandibular muscle may justify ocular pain25. Other investigators have linked headache to TMD in children3,7, a condition frequently associated with sensitivity to palpation of the masseter and temporal muscles25,26.
The literature, however, does not mention other studies that attempt to demonstrate a relationship between the hyperactivity of the sphenomandibular muscle and ocular pain. Weiner et al.27 point to a possible association between TMD and an alteration in the ophthalmic vessels.
The association between hyperactivity of the sphenomandibular muscle and painful sensations behind the eyes might be a result of its retro-orbital origin. The sphenomandibular muscle in spasm might compress the maxillary nerve, stretching and sensitizing it, thereby producing headache and retro-orbital pain21. A patient with TMD might present trigger points and referred pain both from and in the mastication muscles. The referred pain can therefore arise in different regions near its origin28.
Pereira et al.21 report the presence of TMD and ocular symptoms in 84.2% of patients from a sample of 19 individuals. The authors assert that, after the treatment with a myorelaxant plaque, there was relief from the ocular symptoms.
Dawson1 believes that the presence of deep fibers in the anterior portion of the temporal muscle, originating in the posterior region of the lateral wall of the ocular globe, might be the source of the pain behind the eyes.
Garcia et al.3, studying headache of muscular and/or articular origin in 34 examined and treated patients, indicate that 53% of their subjects presented headaches concurrently with muscular spasms17. In addition, dozens of studies have shown an association of vision or ocular symptoms with TMD1,3,19,22,24,25,27-36.
Pullinger et al.12 indicate a correlation between TMD and ocular pain (an unexceptional fact in a clinical setting), yet nothing was recorded in ophthalmological exams. Pereira et al.24 cite several ocular symptoms associated with TMD (ocular pain, abundant tearing, burning and excessive dryness of the eyes, photophobia, pressure, palpebral edema, hyperemia of the conjunctiva, feelings of sand, and sore eyes), without a well established etiological factor.
CONCLUSIONS
Given the assertion that the sphenomandibular muscle is independent of the temporal muscle and located in close proximity to the orbit, the results presented in this study justify the statement that hyperactivity of the sphenomandibular muscles in TMDs has a significant association (p < 0.05) with the manifestation of referred ocular pain.
REFERENCES
1. Dawson PE. Oclusão funcional. Da ATM ao desenho do sorriso. São Paulo: Santos; 2008. [ Links ]
2. Arlen H. Otolaryngologic manifestations of craniomandibular disorders. Dent Clin North Am. 1983;27(3):523-526. [ Links ]
3. Garcia AR, Sousa V. Desordens temporomandibulares: causa de dor de cabeça e limitação da função mandibular. Rev Assoc Paul Dent. 1998; 52(6). [ Links ]
4. Pedroni CR, Oliveira AS, Bérzin F. Pain characteristics of temporomandibular disorder – A pilot study patients with cervical spine dysfunction. J Appl Oral Sci. 2006;14(5):388–392.
5. Saueressig NS, Jaeger ACO, Gründling CA. Desordens craniomandibulares e sua interrelação com outras partes do corpo humano – Relato de caso clínico. J Bras Ocl ATM Dor Orofacial. 2002; 2(7):196–199.
6. de Wijer A, de Leeuw JR, Steenks MH, Bosman F. Temporomandibular and cervical Spine Disorders. Spine. 1996; 21(14):1638-1646. [ Links ]
7. Leistad RB, Sand T, Westgaard RH, Nilsen KB, Stovner LJ. Stress–induced pain and muscle activity in patients with migraine and tensional-type headache. Cephalalgia. 2006; 26(1):64–73.
8. Shankland WE. Headaches dentistry diseases and face alternative medicine. (unknown year and place of publication). [ Links ]
9. Borges RN, Ávila M. Topographic study of the sphenomandibular muscle. Stomatos; 2012; 35: p.3-8. [ Links ]
10. Zarb GA, Carlsson GE, Sessle BJ, Mohl ND. Disfunção das articulações temporomandibulares e dos músculos da mastigação. São Paulo: Santos Editora e Livraria; 2000. [ Links ]
11. Paiva HJ. Noções e conceitos básicos em oclusão, D.T.M. e dor orofacial. São Paulo: Santos Editora e Livraria; 2008. [ Links ]
12. Miller JA. Craniomandibular muscles: their hole in function and form. Boca Raton – Florida: Crc Press; 1991.
13. Pullinger AG, Selingman DA, Salberg WK. Temporomandibular joint tenderness and dysfunction. J Prosthet Dent. 1998; 59(3):263–267.
14. Serrano KVD, Porciúncula HF, Ramalho LTO. Feixe profundo do músculo temporal confronto entre ciência e mídia. Rev. Assoc. Paul. Dent. 2002; 56(1):50-55. [ Links ]
15. Dunn GE, Hack GD, Robinson WL, Koritzer RT. Anatomical observation of a craniomandibular muscle originating from the skull base the esfenomandibularis. J Craniomand Pract. 1996; 14(2):97-103. [ Links ]
16. Koritzer RT, St Hoyme LE. A biophysical model of craniomandibular management. In: Gelb H. New concepts in craniomandibular and chronic pain. New York: Mosbywolf; 1994. [ Links ]
17. Borges RN, Nery DTF. Estudo anatômico do músculo esfenomandibular e sua relação com estruturas anatômicas vizinhas. In: Anais do IX Congresso Internacional de Odontologia de Brasília, 2001. [ Links ]
18. Ernest EA, Martinez ME, Rydzewski DB, Salter EG. Photomicrographic evidence of insertion tendonosis: etiologic factor in pain for temporal tendonitis. J Prosthet Dent. 1991,65(1):121-131. [ Links ]
19. Lõf AS, Fernandes CSD, Bernardi FH, Garcia RS. Esfenomandibular: uma nova entidade anatômica? Rev Odonto Ciênc. 1997; 12(24):197-202. [ Links ]
20. Lille JH, Baver BA. Sectional anatomy of head and neck a detailed Atlas. New York: Oxford University Press; 1994. [ Links ]
21. Palomari ET, Picosse LR, Melquiade SFY. Músculo esfenomandibular ou feixe profundo do músculo temporal? Rev Odont Ciênc. 2000. [ Links ]
22. Shankland WE. Craniofacial pain syndromes that mimic temporomandibular joint disorder. Annals Acad Med Singapore. 1995; 24(1):83-112. [ Links ]
23. Sicher H. Oral anatomy. 4ª ed. Saint Louis: CV MASBY; 1965. [ Links ] 24. Pereira GS, Duarte JM, Vilela EM. Avaliação da sintomatologia ocular em pacientes com desordem temporomandibular. Arq Bras Oftal. 2000,63(4):263-7. [ Links ]
25. Bertoli FM, Antoniuk SA, Bruck I, Xavier GR, Rodrigues DC, Losso EM. Evaluation of the signs and symptoms of temporomandibular disorders in children with headaches. Arq Neuropsiquiatr. 2007; 65(2A):251-255. [ Links ]
26. Gazzit E, Lieberman M, Eini R, Hirsch N, Serfaty V, Fuchs C, Lilos P. Prevalence of mandibular dysfunction in 10-18 year old Israeli school children. J Oral Rehabil. 1984; 11(4):307-317. [ Links ]
27. Weiner LB, Grant LA, Grant AH. Monitoring ocular changes that may accompany use of dental appliances and/or osteopathic craniosacral manipulations in the treatment of TMJ and related problems. Cranio. 1987; 5(3):278-285. [ Links ]
28. Benoliel R, Sharav Y. Neuropathic orofacial pain. Compend Contin Educ Dent. 1998;19(11):1089-1102. [ Links ]
29. Ash MM, Ramfford P, Schmidseder J. Oclusão. 2ª Ed. São Paulo: Santos Livraria e Editora; 2007. [ Links ]
30. Barbosa GAS, Badaró Filho CR, Fonseca RB, Soares CJ, Neves FD, Fernandes Neto AJ. Distúrbios oclusais: Associação com a etiologia ou uma consequência das Disfunções Temporomandibulares. J Bras Ocl ATM Dor Orofacial. 2003;3(10):158–163.
31. Hadi LAAI. Prevalence of temporomandibular disorders in relation to some oclusal parameters. J Prosthet Dent. 1993; 20(4):345-350. [ Links ]
32. Oliveira W. Disfunção temporomandibular. In: Paiva HJ. Noções e conceitos básicos em oclusão, D.T.M. e Dor Orofacial. São Paulo: Santos Editora e Livraria; 2008. [ Links ]
33. Rasmussen OC. Clinical finding during the course of temporomandibular arthropathy. Scand. J Dent Res 1981; 89(3):283-288. [ Links ]
34. Travell JG, Simons DG. Myofascial pain and dysfunction. The trigger point manual. Baltimore: Williams e Wilkins; 1983. [ Links ]
35. Weber JM. TMJ Syndrome: A Possible Cause of Unexplained Eye Problems. 1984; January 20/20. [ Links ]
36. Wesseberg GA, Wolford LM, Zerdecki JW, Epker BN. Ophthalmologic Consideration in Maxillofacial Trauma Anatomy and Diagnostic Evaluations. Int J Oral Surg. 1981; 10(4):236-246. [ Links ]
 Corresponding Author:
Corresponding Author:
Raulino Naves Borges
Faculdade de Odontologia – UFG
Av. Universitária Esquina com 1ª Avenida, s/nº, Setor Universitário, 3º andar
CEP 74605-220 – Goiânia – Goiás – Brazil
E-mail:raulinonaves@hotmail.com













