Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.18 no.34 Canoas Jan./Jun. 2012
SCIENTIFIC ARTICLE
Diagnosing and Raising Awareness about Oral and Cervicovaginal Diseases
Diagnosticando e Alertando para as Enfermidades Bucais e Cérvico-Vaginais
Márcia Cançado Figueiredo1; Viviane Martinez Marset2; Wladimir Fabre Kuroczka2; Kátia Valença Correia Leandro da Silva3
1Associate Professor, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil; PhD in Odontopediatrics, School of Dentistry of Bauru, Universidade de São Paulo (USP), Bauru, Brazil.
2Undergraduate students, School of Dentistry, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil.
3Associate Professor, Institute of Biosciences, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil.
ABSTRACT
Little is known today about the possible correlations between oral and cervicovaginal diseases although some diseases affect these two regions of the human body. This study extensively investigated the pathologies caused by the Candida fungus and the herpes virus to establish the correlation between oral and cervicovaginal diseases. A questionnaire and a cytopathology test (Pap smear) were used to collect data from 118 women whose mean age was 41.51 years and who lived in the coastal city of Xangri-La, Brazil. Descriptive statistics and the Pearson correlation coefficient were used to analyze data (p=0.3 to p=0.7). The Pearson correlation coefficient showed that 16.9% of the women had oral herpes and oral candidiasis. Of the women who had oral herpes, 10% also had genital herpes, but there was no significant correlation between these diseases (χ2 = 0.255, p = 0.614); of those with oral candidiasis, 15% also had vaginal candidiasis, but there was also no significant correlation between these diseases (χ2 = 0.558, p = 0.455). After the cytopathology (Pap smear) results were reviewed, 45.8% of the women in the sample were referred to a gynecologist. Oral and cervicovaginal diseases, especially those that are sexually transmitted, have gained great importance in public health due to their growing incidence and because they affect women in all age groups. Their sequelae may be irreversible and, therefore, should be considered by dentists that treat women.
Keywords: Candidiasis, herpes, cytopathology test.
RESUMO
Pouco se sabe hoje em dia sobre possíveis correlações entre doenças bucais e as doenças cérvico-vaginais. Pode-se afirmar, contudo, que existem doenças que atingem ambas as regiões do corpo humano. O presente estudo foi direcionado para o aprofundado das patologias geradas por fungos Candida e vírus Herpes, com o objetivo de realizar uma correlação entre a presença e ausência de enfermidades bucais e cervico-vaginais, a partir de dados obtidos através de questionário e do exame citopatológico (Papanicolau) coletado de 118 mulheres, com uma média de idade de 41,51 anos, residentes na cidade litorânea de Xangri-Lá, Rio Grande do Sul. O teste de correlação de Pearson demonstrou que 16,9% das mulheres já tiveram herpes labial e candidíase bucal, sendo as mulheres que já apresentaram herpes labial, 10% apresentaram herpes vaginal, mas o resultado não apresentou correlação signifi cativa entre estas doenças (χ2=0,255; p=0,614) e, das mulheres que apresentaram candidíase bucal, 15% já tiveram candidíase vaginal, mas também não se encontrou correlação significativa entre as mesmas (χ2=0,558; p=0,455). 45,8% das mulheres da amostra foram encaminhados para um ginecologista. As enfermidades bucais e cérvico-vaginais femininas, em especial as sexualmente transmissíveis, adquiriram uma grande importância na área de saúde pública por sua crescente incidência, e, por acometerem mulheres em todas as faixas etárias. Suas sequelas podem ser irreversíveis e, deste modo, torna-se importante à atuação do cirurgião dentista durante o atendimento a estas mulheres no sentido de dar-lhes informações mediante a estas enfermidades bucais.
Palavras-chave: Candidíase, herpes, exame citopatológico.
INTRODUCTION
Candida albicans is, undoubtedly, the most frequent species isolated in superficial and invasive infections in different anatomic sites and in patients all over the world. They form a group of 602 types of yeast that have a well-known pathological potential. Their main pathogenic and virulent factors are their capacity to adhere to different types of mucosa and epithelial tissues, their dimorphism and the production of filamentous structures that support tissue invasion, their significant thermal tolerance, and the production of enzymes, such as proteinases and phospholipases.1 Candida may be a normal component of the oral microflora and not cause inflammation. Its incidence increases in the oral microflora with age, and is more often found in the elderly than in younger individuals.2
Oral herpes disseminates by means of intact particles of the virus in saliva in about 2% to 10% of all healthy adults without the clinical disease. The risk of infection from individuals that have the microorganism to other individuals has not been assessed, but is it likely to be low and dependent on the number of virus particles and susceptibility of the host.3
Most individuals (up to 90%) have antibodies against the herpes simplex virus (HSV), and about 40% of these individuals may develop secondary herpes. In Brazil, oral herpes affects 85% of the population, symptoms are seen in 50% of those infected with the virus every years, and about 5% to 10% have more than six recurrences per year.3 Human beings are the only natural reservoirs, and all HSV are capable of living during their whole life in infected hosts.2
Low socioeconomic and cultural conditions are correlated with early exposure to HSV. Currently, the prevalence of contaminated individuals is greater in developing than in developed countries. This incidence increases with age in both types of countries.2
Vulvovaginitis may be caused by bacteria, fungus, protozoa, or even a noninfectious cause.4 According to Oliveira et al.5, cytopathology tests, also known as Pap smears, are internationally accepted as the most appropriate and least expensive instrument to screen changes in cervical cells. The Unified Healthcare System in Brazil (SUS) provides this test as a screening procedure for all Brazilian women registered in the system.6
There are other risk factors for the development of cervical cancer: genetic predisposition, early onset of sexual activity, multiple sex partners, malnutrition, smoking and infection by the human papilloma virus (HPV).7
HPV, the name assigned to a group of over 100 types of viruses, is etiologically important in the onset of cervical cancer.5 HPV infection is transmitted sexually8, and Brazil is one of the countries with the highest HPV incidence, and 50% to 80% of all sexually active women will be infected by one or more types of HPV at some time in their lives.9 In Brazil, cervical cancer is the cause of death of 10 to 12 women per day. In the state of Rio Grande do Sul, 4 women are diagnosed with this type of cancer every day.10
In contrast, some factors associated with vaginal herpes are also associated with cervical cancer, such as early initiation of sex activities, early pregnancy, multiparity, personal or the partner’s promiscuity, viral infections by HPV types 16, 18, 31 or 33, by HSV-2 and by cytomegalovirus, smoking, immune deficiency, use of contraception, ionizing radiation and vitamin A and C deficiencies.11
Studies in the literature confirmed that there is a direct association between these diseases. HSV-1 disseminates predominantly by means of infected saliva or active perioral lesions. HSV-2 adapts better to the genital region, is transmitted predominantly by means of sexual contact and is characterized by the involvement of the genitals and the skin below the waist. There may be exceptions to these characteristics, and HSV-1 may have a pattern similar to that of the HSV-2, and vice-versa. Clinical lesions and tissue changes due to the two HSV types are identical.2
Most of the oral herpes correlations are assigned to HSV-1, although a small percentage may be caused by the HSV-2 as a result of orogenital contact. Previous infection by HSV-1 may provide some protection against infection by HSV-2 due to antibody cross-reactivity.3
In contrast, patients with a clinical diagnosis of vulvovaginal candidiasis present with greater quantities of Candida albicans, both in the vagina and the oral cavity, and have lower levels of anti-Candida IgA antibodies in saliva.12
This study established the correlation between presence and absence of oral and cervicovaginal disease according to data collected using a questionnaire and the cytopathological test (Pap smear) of 118 women residing in the coastal city of Xangri-La, in the state of Rio Grande do Sul, Brazil.
METHODOLOGY
This study was approved by the Ethics in Research Committee of the city government of Porto Alegre, Brazil, registered under CEP 557 number 001.048.151.10.6 on October 10, 2010, and conducted in the Guará Basic Healthcare Unit (UBS Guará) in the city of Xangri-Lá, Brazil, where cervical cancer screening is provided for women living in the region.
One hundred and fifty women were invited to participate in the study, and 118 accepted to be interviewed in a room assigned for that purpose before they underwent cervical cancer screening and collection of vaginal secretion samples in the UBS Guará.
Data about oral and cervicovaginal diseases were collected using a semistructured questionnaire, a type of instrument to facilitate the communication between researchers that aim to collect information about a certain phenomenon and individuals that have this information and may convey it.13 A structured form with 25 closed items was used for that. Each item approached one topic about women’s health: menstruation, hormone replacement, sexual activity, childbirth, gestations, contraception, sex partners, chronic diseases, breast self-exam, mammogram, pap smear, cervical diseases and oral health, which included oral lesions, oral herpes and oral candidiasis (Figure 1).

All women that accepted to participate in the study were informed about the protocol and signed an informed consent term before the interview and the collection of the sample for analysis.
The collection of vaginal secretion took a few minutes and was performed in the office of the UBS Guará gynecologist by only one nurse trained for that. Each sample was handled as usual in the Xangri-Lá healthcare service. The samples were:
a) fixed and correctly labeled by the nurse in charge;
b) sent to the clinical laboratory authorized by the SUS to perform Pap staining and cytopathological (CP) examination;
c) Results were printed and sent to the UBS Guará 15 days after the examination was performed.
Data about the epidemiological profile and the Pap smear were recorded and stored in a Microsoft Office Excel 2010 database for later analysis using descriptive statistics and the Pearson correlation coefficient (p=0.3 to p=0.7).
RESULTS
This study enrolled a final sample of 118 women that were examined and interviewed. Their ages ranged from 16 to 79 years, and mean age was 41.51 years.
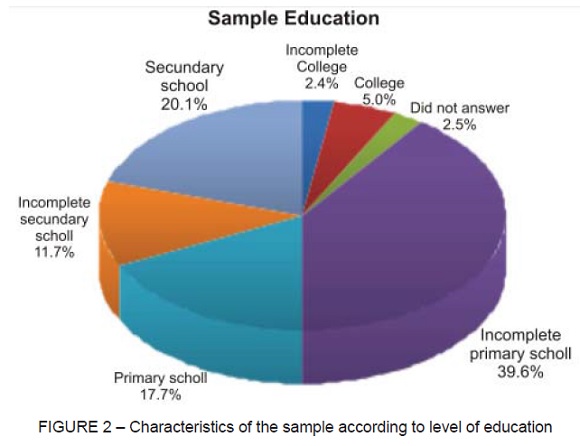
The interviews provided information about the socioeconomic, cultural and health status of the women in the sample and revealed that 29.5% were housewives (n=35) and 22%, janitors (n=26). Most women (39.6%) had not finished primary school (n=47), 20.1% finished secondary school (n=24), 17.7% (n=21) finished only primary school, 11.7% did not finish high school, 5% (n=6) had a college education, 2.4% (n=3) did not finish college, and 2.5% (n=3) did not answer (Figure 2).
When asked about their marital status, 62.7% (n=74) reported being married or having a regular partner for at least one year and 22.8% (n=27), single or having a partner for less than one year. The other results were divided into divorced, separated and widowed. Their religion was Catholic for 75.4% (n=89), and their self-reported skin color was white for 91.5% (n=108). Most (36.3%, n=43) had a family per capita income of two to three minimum wages according to the current value of the minimum wage in the state of Rio Grande do Sul, defined by Law 13.715, passed on April 13, 2011.
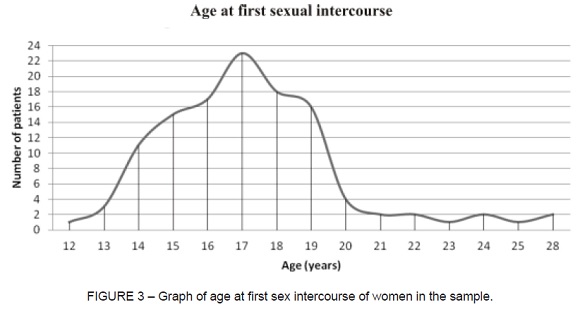
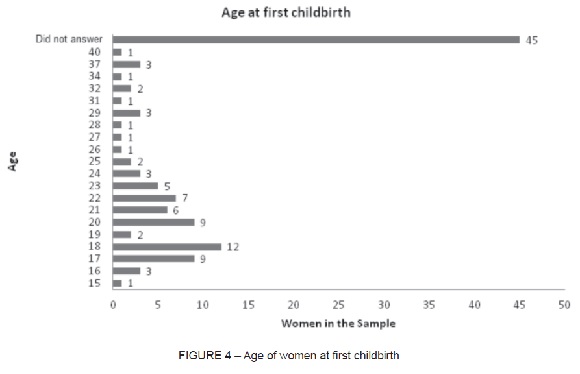
The analysis of data about health and self-care revealed that 61.9% (n=73) still menstruate and 95.8% (n=113) never received hormone replacement. Their age at first sexual intercourse ranged from 12 to 28 years and mean age was 17.2 years (Figure 3); 10.2% (n=12) had the first child at 18 years, but 37.3% (n=44) did not answer this questions (Figure 4); 28% (n=33) had two pregnancies, and mean number of pregnancies ranged from zero to eight, but 12.7% (n=15) did not answer this question; 50.9% of the sample reported not using any contraceptive method, whereas 45.8% did, and 3.3% did not answer the question; 36.4% (n=43) had only one sex partner along their lives, and number of partners ranged from zero (2.5%) to 18 (0.8%) in all the sample.
Data also showed that 19.5% of the women smoked, 58.5% did not practice physical exercises, 71.2% never had any chronic diseases, and of those that had chronic diseases, 12.7% had only one chronic disease, a percentage that reached 0.8% for 3 chronic diseases according to self-report.
When asked to evaluate their health, 55.9% said they had good health according to the choices of excellent, very good, good, average, poor and very poor, described here in decreasing order of quality.
When asked about whether they performed breast self-exam, 57.8% answered yes and 46.6% had performed it in the previous month. About 62.7% had already undergone cervical cancer screening before, and 28.8% of them had it up to one year ago, and 19.4%, to 3 years ago. In the sample, 89.6% of the women believed that this screening test was a form of prevention, when choosing from prevention, treatment or duty.
The analysis of oral diseases revealed that 29.7% (n=35) reported having had some type of oral lesion, of whom 16.9% (n=20) already had oral herpes and 8.5% (n=10) had it since childhood. For 6.7% (n=8), the frequency of herpes recurrence in the current year was 2 times; 16.9% (n-20) of the women also reported already having had oral candidiasis or thrush, and 11% (n=13) had it during childhood; 59.3% (n=70) reported having these diseases because of their weakened immunity.
When asked about whether they had already had HPV, syphilis, candidiasis, genital herpes, AIDS/HIV, gonorrhea or Chlamydia infection and whether they had undergone treatment, we found that 5.1% (n=6) had genital herpes and received treatment, 9.3% (n=11) had candidiasis and received treatment and 5.1% (n=6) had Chlamydia infection and received treatment.
The cytopathological test revealed that 51.6% (n=61) of the samples examined were within normal limits and 36.4% (n=43) had inflammation. Vaginal Candida was found in 1.7% (n=2) of the test samples.
After the results of cytopathological tests were reviewed, 45.8% (n=54) of the women were referred to a gynecologist.
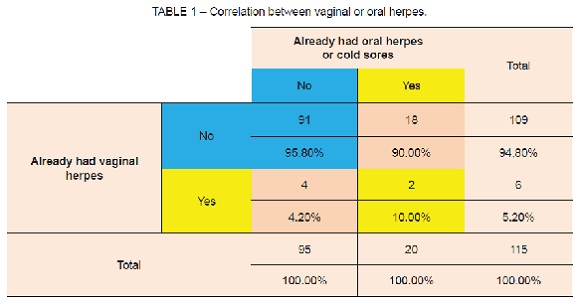
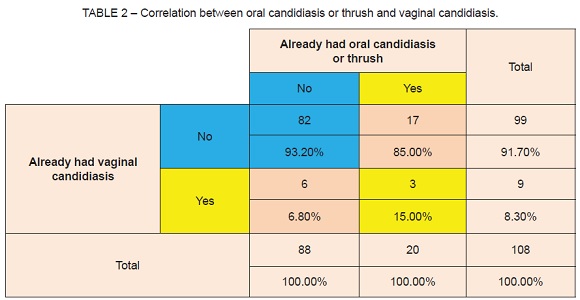
Statistical analysis showed that of the women that never had oral herpes or cold sores, 4.2% (n=4) had already had vaginal herpes, and of the women that had oral herpes, 10% (n=2) had vaginal herpes, with no significant correlation between diseases (χ2=0.255; p=0.614), as shown in Table 1. Of the women that had never had oral candidiasis or thrush, 6.8% (n=6) had already had vaginal candidiasis, and of the women that had had oral candidiasis or thrush, 15% (n=3) had already had vaginal candidiasis, with no significant correlation between the diseases (χ2=0.558; p=0.455), as shown in Table 2.
DISCUSSION
A large number of vulvovaginites are seen in clinical medicine. They are one of the main reasons for a woman to seek a gynecologist or obstetrician. They may be caused by bacteria, fungi, protozoa or even noninfectious causes. The main infectious agents are Candida albicans, Gardnerella vaginalis and Trichomonas vaginalis. However, only in the last years has Candida albicans been diagnosed in the same group, and there has been a significant increase of the number of cases elucidated recently.4 These three agents were the most representative microorganisms found in our sample, in about 12.5% of the patients, which is in agreement with numbers in the literature. However, Gardnerella vaginalis was the most frequent agent, found in 9.3% of the cases, in agreement with findings reported by Ribeiro et al.6, who found that the total prevalence of infection by Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis were 20%, 8% and 2%.
Factors in the life style of women may favor the appearance of infectious cervicovaginal lesions, such as underwear made of synthetic fabrics, inadequate hygiene habits, oral contraceptives, pregnancy, positive HIV and HPV and infections, particularly by Candida albicans. In our study, 45.8% of the women reported using contraception, but only 4.2% had vaginal herpes and 6.8%, candidiasis.
Female sex hormones stimulate the production of lactobacilli that produce lactic acid in the normal vaginal microbiota, which results in an acid pH in the vagina and prevents the proliferation of most pathogens. However, yeasts are an exception because they can proliferate extensively in environments with an acid pH.15 Only 3.4% of the patients received hormone replacement, which was a risk factor of little relevance in our sample.
In the premenstrual period, there is an elevation in the production of female hormones, particularly progesterone, which increases the availability of glycogen in the vaginal region. This environment is favorable for the development of candidiasis because there is an increase of the nutritive substrate for yeasts, which will function as an excellent source of carbon for growth and gemination. Therefore, vaginal candidiasis is associated with regular menstrual cycles.16-17 As 73% of the women still menstruated, this might have been a factor that influenced its development in our sample.
Yeasts such as Candida albicans are found in the oral cavity of 3% to 48% of all adults and 45% to 65% of all healthy children.18 Of our sample, 98.4% of the participants were adults, and 16.9% reported already having had some pathological episode of oral candidiasis or thrush, which does not mean that the microflora in the other patients may have Candida. In different types of mucosa of healthy individuals, yeasts of the Candida albicans genus are found as part of the microbiota and do not trigger infection.
Neville et al.2 reported that the incidence of Candida albicans increases with age, and its presence in the oral cavity may reach 60% among dentate patients older than 60 years who have no signs of lesions in the oral mucosa. Similarly, in our study 6.4% were 60 years or older, and 25% of them reported already having had at least one episode of oral candidiasis. Candida albicans may be found in the oral mucosa of 25% to 75% of healthy individuals. This variation is assigned to population sample size and the sensitivity of the method used to collect and retrieve these microorganisms.19-20
In the analysis of clinical diagnoses of vulvovaginal candidiasis, Silva et al.12 reported that women have greater colonization by Candida albicans, both in the vagina and the oral cavity, and lower levels of anti-Candida IgA antibodies in saliva. Of the women that had already had oral candidiasis, 15% had also had vaginal candidiasis. Although there was no statistically significant correlation between them, these women had both oral and vaginal candidiasis due to different etiological agents, but they should always be instructed to keep good hygiene habits.
Of all women, 16% already had at least one episode of oral herpes in their lives and, according to Regenzi et al.3, most individuals (up to 90%) have antibodies against HSV, and about 40% of these individuals may develop secondary herpes.
Low socioeconomic and cultural conditions are correlated with early exposure to HSV-1. In developing countries, over 50%of the population are exposed at 5 years, 95% at 15 years, and practically 100% at about 30 years of age.2 Data collected in our study showed that women had a low socioeconomic status, as 39.6% had not even finished primary school, 62.3% had a monthly income of up to three minimum wages only, and 68.6% had more than two children. However, they did not have an elevated rate of oral and cervicovaginal diseases, which may be justified by the small sample size or the little education of the participants, who did not know how to differentiate oral candidiasis and herpes because they did not know what the characteristics of these two diseases were.
HSV-1 disseminates predominantly by means of infected saliva or active perioral lesions. HSV-2 adapts better to the genital region, is transmitted predominantly by means of sexual contact and is characterized by the involvement of the genitals and the skin below the waist. There may be exceptions to these characteristics, and the HSV-1 may have a pattern similar to that of the HSV-2, or vice-versa. Clinical lesions and tissue changes due to the two types of virus are identical.2 In our study, no correlation was found between oral and vaginal herpes because of the small number of patients with the diseases under study. Only 16.9% of the women reported already having had oral herpes, and only 6% had already had vaginal herpes. A larger convenience sample only with patients that had one of the two diseases would be necessary to establish a better correlation between vaginal and oral herpes.
Most of the oral herpes correlations are assigned to HSV-1, although a small percentage may be caused by the HSV-2 as a result of orogenital contact. Previous infection by HSV-1 may provide some protection against infection by HSV-2 due to antibody crossreactivity.3 Of the patients with this oral disease, 10% had vaginal herpes.
In conclusion, oral and cervicovaginal diseases in women, particularly those sexually transmitted, are important in public health because of their growing incidence and because they affect women in all age groups. Sequelae may be irreversible and, therefore, dentists should be among the first to provide healthcare to these women and to provide information about oral diseases found during consultation before sample collection. In this study, 15% of these women needed coherent and relevant information adapted to their level of knowledge. The instructions provided by dentists should not be a regressive measure of social control, but, rather, an instrument to enable these women to understand and perceive their own reality.
Therefore, dentistry should act in favor of women’s health in prevention, education and healing, providing humanitarian support, and also promoting the qualification and training of a larger number of professionals that are prepared to understand women’s needs.
CONCLUSION
No significant correlation was found between cervicovaginal and oral diseases in this study. The small sample size may explain this conclusion, and future studies should enroll more female participants with a history of having the diseases under study.
ACKNOWLEDGEMENTS
The authors thank the collaboration of the Department of Health of the city of Xangri-Lá, in the state of Rio Grande do Sul, Brazil, and especially Rosana Fraga, the nurse responsible for the performance of cytopathological tests (Pap smears) in that city.
REFERENCES
1. Dignani MC, Solomkin JS, Anaissie E. Candida. In: Anaissie E, McGinnis MR, Pfaller MA. Medical Mycology. Filadélfia: Livingstone; 2003. P. 195-239. [ Links ]
2. Neville BW, Damm DD, Allen CM, Bouquot JE. Patologia Oral & Maxilo Facial. 2ª ed. Rio de Janeiro: Guanabara Koogan; 2004. 972p. [ Links ]
3. Regenzi JA, Sciubba JJ, Jordan R. Patologia oral – correlações clinicopatológicas. 5ª ed. Rio de Janeiro: Elsevier; 2008. 512p.
4. Zhou X, Westman R, Hickey R, Hansmann MA, Kennedy C, Osborn TW, Forney LJ. Vaginal microbiota of women with frequent vulvovaginal candidiasis. Infect. Immun. 2009;77:4130–35.
5. De Oliveira, MM , Da Silva ENF, Pinto IC, Coimbra VCC. Câncer cérvico uterino: um olhar crítico sobre a prevenção. Revista Gaúcha Enferm. 2004;25(2):176-83. [ Links ]
6. Ribeiro LP, Maradei CM, Da Silva CL, Tombolato RM, Vieira EM. Prevenção do câncer de colo uterino em uma área do programa de saúde da família em Ribeirão Preto. Revista de APS. 2004;7(2):91-95. [ Links ]
7. Greenwood SA, Machado MFAS, Sampaio NMV. Motivos que levam mulheres a não retornarem para receber o resultado do exame papanicolau. Rev Latino-am Enferm. 2006;14(4):503-9. [ Links ]
8. Smeltzer SC, Bare BG. Brunner & Suddarth – Tratado de enfermagem médico-cirúrgica. 10ª ed. Rio de Janeiro: Guanabara Koogan; 2005. 5573p.
9. INCA. Estimativa 2008 – Incidência de câncer no Brasil. INCA [internet]. 2007 [Citado em dezembro de 2011];1:1-96. Disponível em www.inca.gov.br/estimativa/2008/ versaofinal.pdf.
10. INCOLO. Instituto de prevenção do câncer do colo do útero. Porto Alegre: Instituto de prevenção do câncer do colo do útero; [atualizada em 2010; acessado em 15 setembro 2009]. Disponível em: www.incolo.com.br/index.php?option=com_content&task=view &id=91&Itemid=1. [ Links ]
11. Halbe HW. Tratado de ginecologia. 3ª ed. São Paulo: Roca; 2000. 1118p. [ Links ]
12. Silva IS, Koifman F, Koifman RJ. Contribuição dos fatores clínicos, epidemiológicos e genéticos na evolução das lesões precursoras do câncer do colo de útero. [Tese de Doutorado]. Rio de Janeiro: Fundação Oswado Cruz, Escola Nacional de Saúde Pública, Departamento de epidemiologia e métodos quantitativos em saúde; 2008. [ Links ]
13. Chizzotti A. Pesquisa em ciências humanas. 10ª ed. São Paulo: Cortez; 2009. 164p. [ Links ]
14. Mendes CL, Araújo AA, De Sena KXFR Chiappeta AA. Prevalência de Cândida sp. em infecções vaginais. Revista Newslab. 2005; 68:104–112.
15. Álvares CA, Svidzinki TI, Consolaro ME. Candidíase vulvovaginal: fatores predisponentes do hospedeiro e virulência das leveduras. Jornal Brasileiro de Patologia e Medicina Laboratorial. 2007; 43(5): 319-327. [ Links ]
16. Sobel JD. Vulvovaginal candidosis. The Lancet [internet]. 2007 june [citado em dezembro 2011]; 369:9577:1961-71. Disponível em http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2807%2960917-9/fulltext. [ Links ]
17. Ferraza MHSH, Malufi MLF, Consolaro MEL, Shinobu CS, Svidzinski TIE, Batista MR. Caracterização de leveduras isoladas da vagina e sua associação com candidíase vulvovaginal em duas cidades do sul do Brasil. Revista Brasileira de Ginecologia e Obstetrícia. 2005; 27(2):58-63. [ Links ]
18. Samaranayake YH, Samarayake LP. Experimental Oral Candidiasis. Clin Microbiol Ver. 2001;14(2):398-429. [ Links ]
19. Williams DW, Potts AJ, Wilson MJ, Matthews JB, Lewis MA. Characterisation of the inflammatory cell infiltrate in chronic hyperplastic candidosis of the oral mucosa. J Oral Pathol Med. 1997;26(2):83-9. [ Links ]
20. Sherman RG, Prusinki L, Ravenel MC, Joralmon RA. Oral candidosis. Quintessense Int. 2002;33(7):521-32. [ Links ]
 Corresponding Author:
Corresponding Author:
Márcia Cançado Figueiredo
Faculdade de Odontologia
Universidade Federal do Rio Grande do Sul
Rua Ramiro Barcelos, 2492
CEP 90003–035 – Porto Alegre, RS, Brazil
Phone: +55 51 3308.5026
E-mail:mcf1958@gmail.com













