Stomatos
ISSN 1519-4442
Stomatos vol.18 no.34 Canoas ene./jun. 2012
SCIENTIFIC ARTICLE
Nd:YAG Laser Influence on Bond Strength of Adhesive Resins to Dentin
Influência do Uso do Laser de Nd:YAG na Resistência de União de Materiais Resinosos à Dentina
André Amorim Lise1; Paula Cristine Guiggi2; Maurem Leitão Marcondes2; Luiz Henrique Burnett Júnior3; Ana Maria Spohr4
1Undergraduate student of Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
2D.D.S, M.S., PhD students in Restorative Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
3D.D.S., M.S., Ph.D, Adjunct Professor of Restorative Dentistry, Pontifical Catholic University of Rio Grande do Sul, Brazil.
4D.D.S., M.S., Ph.D, Adjunct Professor of Dental Materials, Pontifical Catholic University of Rio Grande do Sul, Brazil.
ABSTRACT
The aim of this study was to evaluate the influence of Nd:YAG laser on microtensile bond strength (μTBS) of different adhesive materials to human dentin. Eighteen human third molars were divided into 6 groups. Group 1 – adhesive system, Adper Single Bond 2 (SB); Group 2 – adhesive system, Clearfil SE Bond (CSEB); Group 3 – self-adhesive resin luting cement, RelyX Unicem; Group 4 – irradiation with Nd:YAG laser and application of SB; Group 5 – irradiation with Nd:YAG laser and application of CSEB; Group 6 – irradiation with Nd:YAG laser and application of RelyX Unicem. A composite resin block was built on the dentin surfaces, and sticks with a cross-sectional area of ~0.80 mm2 were obtained. Twenty specimens per group were selected and subjected to μTBS testing in a universal testing machine. According to the analysis of variance and Tukey test (α = 0.05), the highest μTBS mean was obtained with CSEB (41.75 MPa) without laser irradiation, but this value was not statistically different from CSEB with laser irradiation (33.42 MPa). Mean μTBS of SB without (32.15 MPa) and with (35.38 MPa) laser irradiation did not differ statistically. The lowest μTBS values were obtained for RelyX Unicem, and the group without laser irradiation showed statistically higher values (14.50 MPa) than those found with laser irradiation (7.53 MPa). Nd:YAG laser did not significantly reduce bond strength of the adhesive systems under study, except for the self-adhesive resin luting cement.
Keywords: Laser, Tensile Strength, Dentin-Bonding Agents, Resin Cements.
RESUMO
O objetivo desse estudo foi avaliar a influência do laser Nd:YAG na resistência à microtração de diferentes materiais adesivos à dentina humana. Dezoito terceiros molares humanos foram divididos em 6 grupos. Grupo 1 – Adesivo Adper Single Bond 2 (SB), Grupo 2 – Adesivo Clearfil SE Bond (CSEB), Grupo 3 – Cimento resinoso autoadesivo RelyX Unicem, Grupo 4 – irradiação com laser de Nd:YAG e aplicação de SB, Grupo 5 – irradiação com laser de Nd:YAG e aplicação de CSEB e Grupo 6 – irradiação com laser de Nd:YAG e aplicação de RelyX Unicem. Um bloco de resina composta foi confeccionado sobre essas superfícies de dentina tratadas e os espécimes foram seccionados para obtenção de palitos de 0,80 mm2. Vinte espécimes foram selecionadas por grupo e submetidos a resistência adesiva à microtração (μTBS) em máquina de ensaio universal. De acordo com a análise de variância e teste de Tukey (α = 0,05), a maior média μTBS foi obtida com CSEB (41,75 MPa) sem irradiação por laser, esse valor não diferiu estatisticamente do CSEB com irradiação por laser (33,42 MPa ). A μTBS média de SB sem (32,15 MPa) e com (35,38 MPa) irradiação do laser não diferiram estatisticamente entre si. Os menores valores de μTBS foram obtidos para RelyX Unicem, sendo o valor sem irradiação por laser (14,50 MPa) estatisticamente superior ao com (7,53 MPa). O Laser de Nd: YAG não diminuiu significativamente a resistência de união dos sistemas adesivos estudados, apenas para o cimento resinoso autoadesivo.
Palavras-chave: Laser, Resistência de União, Adesivos Dentinários, Cimentos de Resina.
INTRODUCTION
The development of adhesive systems has allowed restorative procedures to be carried out with minimal removal of sound tooth structure, due to a micromechanical bonding of restorative materials to enamel and dentin. Dentin presents a more complex substrate than enamel for bonding, and many studies have been devoted to understanding the mechanism of dentin bonding1.
Adhesive systems have been chemically enhanced to improve their bonding ability to dentin. Parallel to this, manufacturers have invested in simplified adhesives that are quick and easy to use. The traditional three-stage application (conditioner, primer, and adhesive) has been replaced by three different product categories, as follows: two-step etch-and-rinse adhesives – the primer and the adhesive are applied simultaneously after acid etching; self-etching primers – the acid etching and primer stages occur simultaneously, followed by the application of the adhesive; and self-etching adhesives – the acid etching, primer and adhesive stages occur at the same time. More recently, self-adhesive resin luting cements that do not need pretreatment for bonding to tooth substrates have been developed2-3.
At the same time, a number of new technologies have been developed to optimize the efficacy of adhesive systems, such as the use of laser radiation. Over the past 30 years, several types of lasers have been used with different goals in soft tissues and tooth structures, including the Nd:YAG laser, which has been shown to be effective in dentistry for tooth hypersensitivity, removal of carious tissue, sealing enamel pits and fissures, removal of soft tissue4, and disinfection of dental tissues5.
The application of Nd:YAG laser leads to morphological changes in the tooth substrate6, making dentin more resistant to demineralization by acids7, which are applied to demineralize the dentin and allow the adhesive to penetrate, aiming to reveal the hybrid layer. However, the application of laser may compromise the capacity of adhesive materials to bond to the dentin substrate8-9, and consequently the longevity of the restoration.
The aim of this study was to evaluate the influence of Nd:YAG laser on microtensile bond strength (μTBS) of different adhesive materials to dentin. The hypothesis to be analyzed is that Nd:YAG laser does not influence bond strength of adhesive materials to dentin.
METHODOLOGY
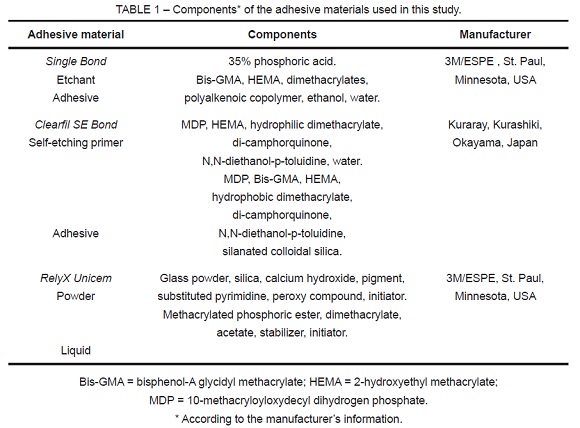
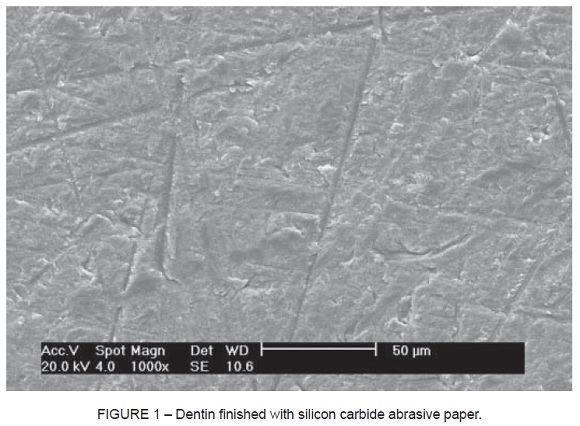
Eighteen unerupted human third molars, extracted for therapeutic reasons, were cleaned of gross debris and stored in distilled water at 4º C. The water was changed every week and the teeth were used within a period not exceeding 6 months. Roots were mounted in self-cured acrylic resin, and the occlusal surface enamel was removed with a low-concentration diamond disc mounted in a low-speed laboratory cutting machine (Labcut 1010; Extec Corp., London, England), under cooling, to obtain a flat dentin surface. Dentin surfaces were finished with 400- and 600-grit silicon carbide abrasive paper placed in a polishing machine (DPU-10; Panambra, São Paulo, SP, Brazil) under water. After polishing, the teeth were randomly divided into six groups according to the materials used (Table 1) and treatments carried out on dentin.
Group 1 – Adper Single Bond 2: the dentin was treated for 15 s with 35% phosphoric acid and rinsed for 30 s under running tap water. Excess water was removed with a cotton pellet, leaving a moist surface. Two consecutive coats of adhesive were applied, using a saturated brush tip. After gently air drying for 5 s, the material was light cured with a light-curing unit (XL 3000; 3M, St. Paul, MN, USA) for 10 s.
Group 2 – Clearfil SE Bond: the self-etching primer was applied to enamel and dentin using a brush tip and left in place for 30 s. Excess solvent was removed by air drying for 5 s. The bond was applied to the surface cavity with a brush tip and gently air dried for 3 s, followed by light curing for 20 s.
Group 3 – RelyX Unicem: the capsule was activated and its internal content was mixed using a high-frequency oscillator for 10 s. The material was applied to the dentin to approximately 1 mm thickness and light cured for 40 s.
Group 4 - Nd:YAG + Adper Single Bond 2: a coat of Nanquim (Trident, Itapuí, SP, Brazil) was applied over the dentin for better absorption of laser radiation onto the dentin surface. A Nd:YAG laser system (Pulse Master 1000; American Dental Technologies, Corpus Christi, TX, USA), with a wavelength of 1064 nm and 150 μm pulse duration, was used. The parameters used were 0.9 W, 15 Hz, 60 mJ per pulse, with an optic fiber of 400 μm, generating energy of 47.70 mJ/cm2 per pulse. The optic fiber was used in a standard position, perpendicular to the tooth surface, located approximately 1 mm from the tooth surface. A 2-min time period was stipulated for laser application over the entire dentin surface. After laser application, residual Nanquim was removed using a microbrush under running water. Then, the adhesive system was applied as described for group l.
Group 5 - Nd:YAG + Clearfil SE Bond: Nd:YAG laser was applied as described for group 4, followed by the adhesive system as described for group 2;
Group 6 - Nd:YAG + RelyX Unicem: Nd:YAG laser was applied as described for group 4, followed by the self-adhesive resin luting cement as described for group 3.
After the adhesive materials were polymerized, the surface was built up with Z250 (3M, St. Paul, MN, USA) composite resin in two layers to a height of 4 mm. Each layer was light cured for 40 s with XL 3000. The light intensity was controlled by a radiometer model 100 (Demetron/Kerr, Danbury, CT, USA), remaining between 500 and 530 mW/cm2.
After bonding procedures, specimens were stored for 24 h at 37o C in distilled water. The teeth were then sectioned perpendicular to the bonding surface using a laboratory cutting machine (Labcut 1010) at a speed of 400 rpm with a diamond disc No. 15280 (Buehler, Lake Bluff, Illinois, USA) under water cooling. The specimens had approximately 0.90 x 0.90 mm of transverse section, as measured with a digital caliper (Mitutoyo Sul Americana Ltda., Suzano, SP, Brazil), and were examined under a stereomicroscope (Olympus Corp., Tokyo, Japan) at 10x magnification to analyze the adhesive area. Those showing defects, such as bubbles, lack of material, or irregular area, were discarded. Twenty specimens were selected per group.
The test specimens were then fitted to the microtensile testing device for μTBS testing. This device has two stainless steel grips (8 x 10 mm) and sliding shafts that prevent torsion movements during the tests, associated with a fixing screw that prevents the test specimen from moving during bonding. The test specimens were fixed with cyanoacrylate glue (Loctite, São Paulo, SP, Brazil), associated with an accelerator fluid (Zip Kicker; Pacer Technology, Rancho Cucamonga, CA, USA), and stressed to failure at a crosshead speed of 0.5 mm/min in a universal testing machine (EMIC DL-2000, São José dos Pinhais, PR, Brazil) using a 50-N load cell. Experimental values for μTBS were expressed in MPa, as derived from dividing the imposed force (N) at the time of fracture by the bond area (mm2).
The fractured surfaces of 10 specimens from each group were observed by scanning electron microscopy (SEM) (Philips XL 30, Philips Electronic Instruments Inc., Mahwah, NJ, USA) at 100x magnification. Failures were classified as: a) adhesive failure (failure across the bonding interface, with or without cohesive failure in the adhesive resin for groups 1, 2, 4, and 5); b) cohesive failure in dentin (dental substrate failure); c) cohesive failure in composite resin (rupture of the composite resin for groups 1, 2, 4, and 5, and of the resin cement for groups 3 and 6); d) mixed failure (association of adhesive and cohesive failure in dentin and/or composite resin for groups 1, 2, 4, and 5, and in resin cement for groups 3 and 6).
In two human third molars, the occlusal enamel was removed to obtain a flat occlusal dentin surface. The dentin surfaces were finished with 400- and 600-grit silicon carbide abrasive paper. The Nd:YAG laser was applied to half of the dentin surface as described for group 4. The specimens were observed by SEM at 1000x magnification.
The μTBS values were analyzed by analysis of variance (ANOVA), and post-hoc multiple comparisons using the Tukey test (α = 0.05).
RESULTS
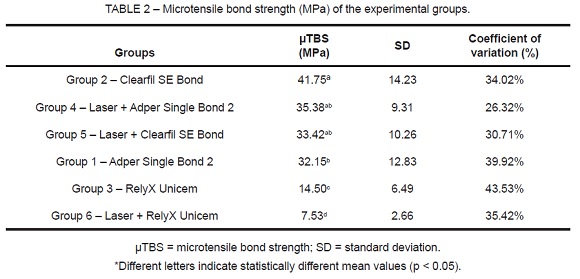
The highest μTBS mean was obtained with Clearfil SE Bond (41.75 MPa) without laser irradiation, but this value was not statistically different from Clearfil SE Bond with laser irradiation (33.42 MPa). Mean μTBS of Adper Single Bond 2 without (32.15 MPa) and with (35.38 MPa) laser irradiation did not differ statistically. The lowest μTBS values were obtained for RelyX Unicem, and the group without laser irradiation showed statistically higher values (14.50 MPa) than those found with laser irradiation (7.53 MPa) (Table 2).
Mixed failure occurred in all groups. There was a 100% rate of mixed failure for RelyX Unicem with and without laser irradiation. Adhesive failure occurred in specimens treated with Adper Single Bond 2 and Clearfil SE Bond with and without laser irradiation. There was no cohesive failure in composite resin or dentin (Table 3).
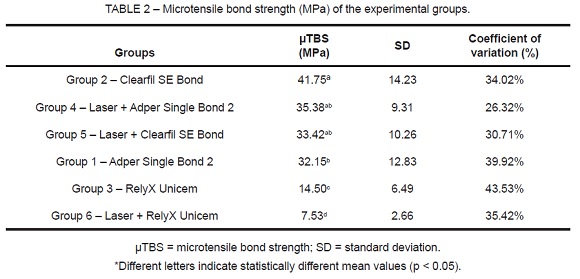
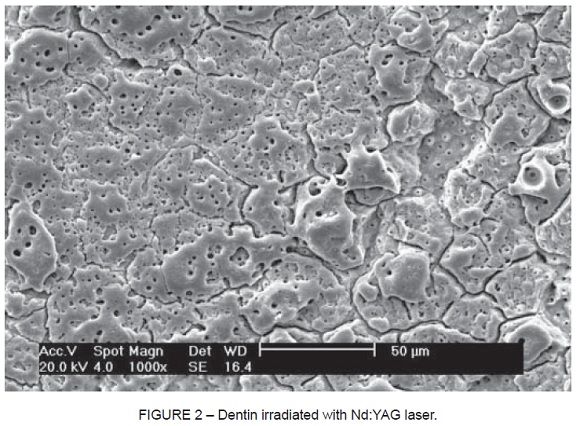
Figure 1 shows the dentin surface after polishing with silicon carbide abrasive paper, with the presence of smear layer. Figure 2 shows the dentin surface after Nd:YAG laser irradiation. Laser irradiation caused surface melting and small scattered areas with some open dentinal tubules.
DISCUSSION
Adhesive materials have evolved rapidly in recent years with the purpose of improving clinical performance, allowing greater durability of restorations and application of simplified techniques. Clinical studies evaluating the performance of these materials are of paramount importance to the applicability of the techniques.
However, because clinical trials are very complex and expensive experiments, laboratory studies have been used as an option, such as those aiming to test bond strength to tooth structures. These laboratory tests allow a comparison between materials in terms of bonding to different substrates10.
Three different adhesive materials were tested in the present study. Adper Single Bond 2 adhesive system involves etching with 37% phosphoric acid as the first clinical procedure, and the simultaneous application of the primer and adhesive at a second stage. Clearfil SE Bond adhesive system is characterized by the application of a self-etching primer, followed by an adhesive. RelyX Unicem is a self-adhesive resin luting cement that does not need application of an adhesive prior to cement application, according to the manufacturer’s instruction.
Based on the results of this study, our hypothesis cannot be fully confirmed, because a significant decrease in bond strength was observed for RelyX Unicem.
Schaller et al.7 showed that laser irradiation may produce an acid-resistant layer on the surface of dentin, as etching with phosphoric acid was not able to remove the recrystallized areas. However, in this study, laser irradiation induced significant topographic alterations in dentin surfaces (Figure 2). Surface melting was observed, followed by recrystallization, and dentin assumed a vitrified appearance, exhibiting an irregular surface resembling dimples, with a spongy appearance. The region between the areas with this appearance showed normal dentin, with some open dentinal tubules. Other studies have also observed these surface alterations11-13, which may favor micromechanical retention14-15. Therefore, concerning Adper Single Bond 2 and Clearfil SE Bond adhesive systems, it is believed that the difficulty in etching may have been counterbalanced by a micromechanical retention caused by topographic alterations in dentin surface when Nd:YAG laser was irradiated.
In addition, studies have shown that Nd:YAG laser can cause changes in the chemical composition of dentin16. Kobayashi et al.17 evaluated bond strength of luting glass ionomer cement to a dentin surface irradiated with Nd:YAG laser and showed that Nd:YAG laser irradiation increased the calcium and phosphorous content of dentin and reduced the amount of oxygen. For those authors, these changes may have contributed to the increase in the molecular binding of carboxyl groups of the polyalkenoic acid present in the glass ionomer cement with the calcium of the dentin, favoring the increase in bond strength observed in the study. Based on that, we can speculate that, in this study, the laser energy delivered increased the calcium concentration, thus preventing a significant reduction in bond strength of Adper Single Bond 2 and Clearfil SE Bond adhesive systems. This would provide greater chemical bonding of the polyalkenoic acid copolymer component of Adper Single Bond 2, as well as of the functional monomer 10-MDP present in Clearfil SE Bond, with the calcium of the dentin18. Matos et al.4, testing a self-etching adhesive with MDP on dentin irradiated with Nd:YAG laser, also found that bond strength was not compromised.
The self-adhesive resin luting cement, RelyX Unicem, had the lowest mean μTBS values compared to the other two adhesive materials. This probably occurred because this resin cement interacts more superficially with the dentin, without the need for previous acid etching as when using Adper Single Bond 2 (phosphoric acid) and Clearfil SE Bond (selfetching primer). RelyX Unicem consists of alkaline fillers and multifunctional phosphoric acid methacrylates, which are responsible for its self-etching properties19. Studies have shown that this self-adhesive cement was unable to demineralize or dissolve the smear layer completely, and no decalcification and infiltration of dentin occurred and no hybrid layer or resin tags were observed20-22. Some reasons have been proposed for the limited capacity of self-adhesive resin cements to diffuse and decalcify the underlying dentin effectively: 1) high viscosity, which may rapidly increase as an acid-base reaction; 2) a neutralization effect may occur during setting, because these chemical reactions involve water release and alkaline filler that may raise the pH level23. According to De Munck et al.21 and Gerth et al.24, RelyX Unicem presents a chemical chelation reaction between phosphoric acid monomers and calcium ions derived from hydroxyapatite in tooth tissues.
The low bond strength values found in the groups luted with self-adhesive resin cement may also be related to the lack of pressure exerted on the cement. Pressure is important during cement application to avoid bubbles and open spaces on the interface, which might compromise the longevity of adhesive bonds and achieve a close fit with the cavity walls due to the thixotropic properties of this cement21.When RelyX Unicem was applied to the irradiated dentin, there was a significant decrease in μTBS. One factor that possibly contributed to this finding is that this resin cement is more viscous than the adhesives and, therefore, did not have the same wettability to penetrate the irradiated dentin in an appropriate way in the micromechanical retention caused by the laser on the dentin.
RelyX Unicem has two setting reactions: redox reaction for polymerization of the resinous phase and an acid-base reaction resulting in the formation of calcium phosphate. Bonding to dentin is established by ionization of the methacrylate phosphoric acid during the mixture of monomers. Ionization uses water from the dentin as well as water produced during the neutralization reaction of phosphate monomers with the basic particles19. Because the presence of water is important for the ionization reaction to occur, the dentin surface was left slightly wet before applying the self-adhesive resin luting cement, as recommended by the manufacturer.
Failure mode analysis was used because it allows us to verify whether the methodology is able to provide bond strength values corresponding to the adhesive-dentin interface. In addition, it allows us to determine which is the weakest region and most susceptible to failure25. Adper Single Bond 2 and Clearfil SE Bond showed a greater tendency to adhesive failure after laser irradiation. This suggests that the adhesive-dentin interface was weakened by Nd:YAG irradiation compared to groups in which laser was not applied. As for RelyX Unicem, regardless of the application of laser, there was a 100% rate of mixed failure, occurring always at the bonding interface level, and the resin cement remained in place on a part of the dentin surface.
Self-adhesive resin luting cements, such as RelyX Unicem, are indicated for the fixation of inlays, onlays, overlays, and complete crowns. Extrapolation of these results to clinical practice may suggest the use of this resin cement for restorations, in which retention principles and mechanical stability of the preparation are respected. In the case of preparations without friction retention, in which bonding to the tooth will depend more on the adhesive material, the use of adhesive systems associated with resin cements would be recommended.
CONCLUSION
The application of Nd:YAG laser to the dentin did not significantly compromise bond strength of Adper Single Bond 2 and Clearfil SE Bond adhesive systems, with a significant decrease only in bond strength of RelyX Unicem.
REFERENCES
1. Swift EJr, Perdigão J, Heymann HO. Bonding to enamel and dentin: a brief history and state of the art. Quintessence Int. 1995;26(2):95-110. [ Links ]
2. Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NR, Pashley DH. Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentin. J Dent. 2004;32(1):55-65. [ Links ]
3. Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumans M. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23(1):71-81. [ Links ]
4. Matos AB, Oliveira DC, Navarro RS, de Eduardo CP, Matson E. Nd:YAG laser influence on tensile bond strength of self-etching adhesive systems. J Clin Laser Med Surg. 2000;18(5):253-7. [ Links ]
5. Klinke T, Klimm W, Gutknecht N. Antibacterial effects of Nd:YAG laser irradiation within root canal dentin. J Clin Laser Med Surg. 1997;15(1):29-31. [ Links ]
6. Anić I, Segović S, Katanec D, Prskalo K, Najzar-Fleger D. Scanning electron microscopic study of dentin lased with Argon, CO2 and Nd:YAG laser. J Endod. 1998;24(2):77-81. [ Links ]
7. Schaller HG, Weihing T, Strub JR. Permeability of dentine after Nd:YAG laser treatment: an in vitro study. J Oral Rehabil. 1997;24(4):274-81. [ Links ]
8. Moritz A, Schoop U, Goharkhay K, Szakacs S, Sperr W, Schweidler E, Wernisch J, Gutknecht N. Procedures for enamel and dentin conditioning: a comparison of conventional and innovative methods. J Esthet Dent. 1998;10(2):84-93. [ Links ]
9. Matos AB, Oliveira DC, Kuramoto M Jr, Eduardo CP, Matson E. Nd-YAG Laser influence on sound dentin bond strength. J Clin Laser Med Surg. 1999;17(4):165-9. [ Links ]
10. Wilson NH. The evaluation of materials: relationships between laboratory investigations and clinical studies. Oper Dent. 1990;15(4):149-55. [ Links ]
11. Cernavin I. A comparison of the effects of Nd:YAG and Ho:YAG laser irradiation on dentin and enamel. Aust Dent J. 1995;40(2):79-84. [ Links ]
12. Kinney JH, Haupt DL, Balooch M, White JM, Bell WL, Marshall SJ, Marshall GW Jr. The threshold effects of Nd and Ho:YAG laser- induced surface modification on demineralization of dentin surfaces. J Dent Res. 1996;75(6):1388-95. [ Links ]
13. Sazak H, Türkmen C, Günday M. Effects of Nd:YAG laser, air- abrasion and acidetching on human enamel and dentin. Oper Dent. 2001;26(5):476-81. [ Links ]
14. Ariyaratnam MT, Wilson MA, Blinkhorn AS. An analysis of surface roughness, surface morphology and composite/dentin bond strength of human dentin following the application of the Nd:YAG laser. Dent Mater. 1999;15(4):22-8. [ Links ]
15. Rolla JN, Mota EG, Oshima HM, Burnett Jr LH, Spohr AM. Nd:YAG laser influence on microtensile bond strength of different adhesive systems to human dentin. Photomed Laser Surg. 2006;24(6):730-4. [ Links ]
16. Paranhos MPG, Spohr AM, Marcondes M, Oshima Hm, Mota EG, Burnett Jr LH. Influence of Nd:YAG laser irradiation on microtensile bond strength of adhesive systems to sound or carious dentin. Quintessence Int. 2009;40(2):145-53. [ Links ]
17. Kobayashi CA, Fujishima A, Miyazaki T, Kimura Y, Matsumoto K, Osada T, Fukunaga H, Kawawa T. Effect of Nd:YAG laser irradiation on shear bond strength of glass-ionomer
luting cement to dentin surface. Int J Prosthodont. 2003;16(5):493-8.
18. Yoshida Y, Nagakane K, Fukuda R, Nakayama Y, Okazaki M, Shintani H, Inoue S, Tagawa Y, Suzuki K, De Munck J, Van Meerbeek B. Comparative study on adhesive performance of functional monomers. J Dent Res. 2004;83(6):454-8. [ Links ]
19. Technical data sheet (2007) Expertise; RelyX Unicem. 3M ESPE Dental Products, Seefeld, Germany; Retrieved online July 10, 2008 from: http://multimedia.mmm.com/mws/mediawebserver.dyn?666666Zjc61Vs666iFPCOrrrrQ- [ Links ]
20. Yang B, Ludwig K, Adelung R, Kern M. Micro-tensile bond strength of three luting resins to human regional dentin. Dent Mater. 2006;22(1):45–56.
21. De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004;20(10):963-71. [ Links ]
22. Goracci C, Cury AH, Cantoro A, Papacchini F, Tay FR, Ferrari M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J Adhes Dent. 2006;8(5):327–35.
23. Monticelli F, Osorio R, Mazzitelli C, Ferrari M, Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J Dent Res. 2008;87(10):974–9.
24. Gerth HU, Dammaschke T, Züchner H, Schäfer E. Chemical analysis and bonding reaction of RelyX Unicem and Bifi x composites- A comparative study. Dent Mater. 2006;22(10):934-41. [ Links ]
25. Armstrong SR, Keller JC, Boyer DB. Mode of failure in the dentin-adhesive resinresin composite bonded joint as determined by strength-based (μTBS) and fracture-based (CNSB) mechanical testing. Dent Mater. 2001;17(3):201-10.
 Corresponding Author:
Corresponding Author:
Ana Maria Spohr
School of Dentistry
Pontifical Catholic University of Rio Grande do Sul (PUCRS)
Av. Ipiranga, 6681 – Block 6
CEP 90616–900 – Goiânia, GO, Brazil
Phone: xx51–9995-0465, Fax: xx51–3342-8569
E-mail:anaspohr@terra.com.br













