Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.18 no.34 Canoas Jan./Jun. 2012
SCIENTIFIC ARTICLE
Change of Incisive Papilla Height Due to Orthodontic Movement: An Evaluation in Study Models and Three-Dimensional Images
Alteração da altura Papilar Interincisiva Devido a Movimentação Ortodôntica: Avaliação em Modelos de Estudo e Imagens Tridimensionais
Luma Oliveira Castro1; Germana Jayme Borges2; Iury Oliveira Castro3; Olavo Cesar Lyra Porto4; Carlos Estrela5
1Post-graduate periodontics at the institution in ABO-GO.
2Master and Specialist in Periodontics, PhD student in Health Sciences Professor of Periodontology at the ABO-GO.
3Master in Clinical Dentistry, Faculty of Dentistry, Federal University of Goiás, Goiania, Goiás, Brazil.
4Master of Health Sciences, Faculty of Medicine, Federal University of Goiás, Goiania, Goiás, Brazil.
5Associate Professor, Professor of Endodontics, Faculty of Dentistry, Federal University of Goiás.
ABSTRACT
The presence of gingival papillae in the anterior maxilla is essential to the aesthetics of the smile. The aim of this study was to evaluate alterations in the height of the upper central incisive papilla, before and after orthodontic movement, using study casts and cone beam computed tomography (CBCT). Sixteen patients between the ages of 13 and 18 years underwent orthodontic treatment. The height of the papillae was calculated in both initial and final study casts by drawing a horizontal line tangent to the zenith of the central incisors and inscribing a vertical line perpendicular to the horizontal line. Papilla height was defi ned as the distance from the tip of the papilla to the point of intersection between the two lines. Initial and final (after orthodontic treatment) CBCT images were analyzed, and the height of interproximal papillae was calculated by measuring the distance from the tip of the papilla to the alveolar bone crest. This measurement was performed in both sagittal and coronal plane views. Data were statistically analyzed using the Student t test. The level of significance was 5%. Initial mean papilla height was 4.6 ± 0.8 mm, and the final value in study casts was 4.3 ± 1.2 mm; there was not a statistically significant difference between initial and final values (p = 0.309). In the CBCT coronal sections, initial mean papilla height was 3.5 ± 1.2 mm vs. 3.1 ± 0.7 mm after treatment (p = 0.094); again, no statistically significant differences were observed. In the sagittal plane, there was a significant difference (p = 0.05) between initial (3.7 ± 1.1 mm) and final (3.1 ± 0.6 mm) mean papilla height. According to our findings, and to the different measuring techniques employed, the height of the papilla changed little as a result of orthodontic therapy.
Keywords: gingival papilla, cone beam computed tomography, orthodontic treatment.
RESUMO
A presença de papila gengival na região anterior da maxila é essencial para a estética do sorriso. O objetivo deste estudo foi avaliar as alterações na altura papilar dos incisivos centrais superiores, antes e após movimentação ortodôntica, utilizando modelos de estudo e tomografia computadorizada de feixe cônico (TCFC). Dezesseis pacientes, com idades entre 13 e 18 anos, foram submetidos a tratamento ortodôntico. A altura da papila foi calculada nos modelos de estudo iniciais e finais. Para isso, uma linha horizontal foi traçada tangente ao zênite dos incisivos centrais e uma linha vertical foi inscrita perpendicularmente à linha horizontal. A altura papilar foi definida como a distância entre a ponta da papila até o ponto de intersecção entre as duas linhas . Nas imagens TCFC inicial e final de cada paciente, a altura da papila foi caldulada com base na distância do ponto de contato interproximal até a crista do osso alveolar. Esta medida foi realizada em cortes sagitais e coronais. Os dados foram analisados estatisticamente utilizando teste t de Student. O nível de significância foi de 5%. A altura média inicial papilar foi de 4,6± 0,8 mm, e a final, de 4,3 ± 1,2 mm; não houve diferença estatisticamente significativa entre as medidas (p = 0,309). No corte coronal da TCFC, a altura média inicial papilar foi de 3,5 ± 1,2 mm, e a final, de 3,1 ± 0,7 mm final (p = 0,094); novamente, não houve diferença estatisticamente significativa. No corte sagital, houve uma diferença significativa (p = 0,05) entre as alturas inicial (3,7 ± 1,1 mm) e final (3,1 ± 0,6 mm) média papilar. De acordo com nossos resultados e com os diferentes métodos de medição empregados, a altura da papila sofreu pouca alteração após terapia ortodôntica.
Palavras-chave: papila gengival, tomografia computadorizada de feixe cônico, tratamento ortodôntico.
INTRODUCTION
Interdental space, or the space located between two adjacent teeth, has a pyramidal shape that is determined by tooth morphology and delimited by the ridge crest and the point of contact between them. The space is filled with the interdental gingival papilla, formed of dense tissue covered by oral epithelium. Forming the papilla are: the relationship between the contact of the teeth, interdental spaces, and the proximal surfaces of the cementoenamel junction1,2.
The presence or absence of the interproximal papilla depends on the distance between the point of contact between teeth and the interdental bone crest. When the vertical distance from the point of contact to the bone crest is 5 mm or less, the papilla is usually present. When this distance is 6 mm or more, the papilla is generally absent2-6.
Several conditions can change the interdental space and, as a consequence, affect the morphology of the interdental papilla. For instance, dental anomalies (irregular contours of crowns, prosthetic restorations, trauma, and periodontal disease) can cause loss of interdental papillae3-6. Orthodontic movement can cause changes in the alveolar bone crest, as a result of dental intrusion and extrusion or vertical movement This change can be observed clinically, by measuring papilla height, as well as by means of three-dimensional images7-11.
Cone-beam computed tomography (CBCT) allows three-dimensional visualization of dental structures and supporting tissues. Because of the image resolution obtained, and because of the possibility of rebuilding the structure in axial, sagittal, and coronal planes, CBCT has attracted increasing attention in various areas of dentistry8-11. Vasconcelos et al.12 compared periapical radiographs with CBCT images in the detection and location of alveolar bone loss. CBCT was the only method that allowed surface analysis of buccal and palatal/lingual aspects, thereby providing a better visualization of the morphology of the bone defect.
The aim of this study was to evaluate, using both study casts and CBCT imagery, changes in papilla height resulting from orthodontic treatment.
METHODOLOGY
Selection of Patients
Sixteen patients between the ages of 13 and 18 years seeking orthodontic treatment were selected for the study. Patients were informed about the aims of both the treatment and the research project, as well as of the terms contained in the informed consent approved by the local research ethics committee (Federal University of Goiás, Brazil, protocol no. 235/2010).
Subjects were included in the study if they presented with Angle Class I malocclusion, full eruption of maxillary central incisors, and an absence of caries, periodontitis, or crowding in the area.
Data Collection
Before and after orthodontic treatment, standardized photographs were taken of the patients’ anterior maxillary region, and molds were created to obtain study casts of their upper jaws. CBCT images were also obtained before and after treatment for the purpose of diagnosis and treatment planning. These images were taken at a private radiology clinic (the Center for Integrated Dental Radiology - CIRO, Goiânia, Brazil) using an i-CAT device (Imaging Sciences International, Hatfield, USA). Volumes were reconstructed using an isometric voxel of 0.25 mm, a tube voltage of 120 kVp, and a tube current of 3.8 mA. Exposure time was 40 seconds (scan size of 13 cm), and images were generated in gray scale (14 bits), with a focal length of 0.5 mm and one single 360° image rotation.
Analysis of Papilla Height
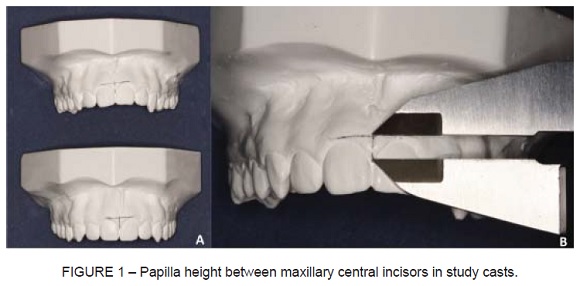
Study casts were used and were obtained before and after orthodontic treatment to measure the papillae height between maxillary central incisors. Upon each study cast, two lines were drawn, one horizontal tangent to the zenith of the central incisor, and a vertical line perpendicular to the horizontal one, through the tip of the papilla (Figure 1A). Papilla height was defined as the distance from the tip of the papilla to the intersecting point between the two lines. With the aid of a 0.01 mm digital caliper, the distance between these points was measured (Figure 1B). A single operator performed all measurements.
Initial and final CBCT images of each patient were analyzed, and the height of interproximal papillae was calculated by measuring the distance from the tip of the papilla to the alveolar bone crest. This measurement was performed in both sagittal and coronal images (Figure 2).

Statistical Analysis
Student’s t test for paired samples was used to analyze data. All statistical analyses were performed on the Statistical Package for the Social Sciences (SPSS Inc., Chicago, USA). Significance was set at p < 0.05.
RESULTS
Initial mean papilla height measured in the study casts was 4.6 ± 0.8 mm, and the final mean was 4.3 ± 1.2 mm. There was no statistically significant difference between the two values (p = 0.309). In coronal CBCT images, the initial mean papilla height was 3.5 ± 1.2 mm, and the fi nal, 3.1 ± 0.7 mm. Again, no statistically significant difference was observed (p = 0.094). In sagittal views, there was a significant difference (p < 0.05) between initial (3.7 ± 1.1 mm) and final (3.1 ± 0.6 mm) mean papilla height. The height of the papillae changed little as a result of orthodontic treatment; this change did not interfere with either the aesthetics of the smile or the mechanics of speech (Table 1).

DISCUSSION
The papilla incisiva highlights the human smile underscoring the importance of analyzing any risk factors that might cause changes to its anatomy.
The papilla is considered healthy and present in periodontal terms when it occupies all the space between the contact point and the alveolar bone crest. Thus, the distance between the bone crest and the contact point should be approximately 5 mm6,14,15,17. In the present study, papilla height measurements, made both clinically (study casts) and on three-dimensional images, were lower than 5 mm, with no significant presence of “black space,” which would compromise the smile aesthetics.
When the absence of the papilla occurs due to morphological or positioning reasons2,14, it is possible to restore the aesthetics of the papillae through orthodontic movement, use of prosthetic crowns, or by adapting the shape of the teeth. An alternative option suggested by Becker et al.19 involves the use of hyaluronic acid in cases of small papillary recessions, and is thought to be safe, effective, and minimally invasive. Other studies suggest surgical techniques for the correction of papillary defects resulting from of an excessive loss of bone tissue3,4,13,16,17.
Cardaropoli et al.4 have determined the optimal mean distance from the point of contact between adjacent teeth to the alveolar bone crest in patients undergoing periodontal surgery for papillary reconstruction after orthodontic treatment. The authors suggest a distance of 6.46 mm, which is above the highest mean obtained in this study (4.6 ± 0.8 mm). Carnio16 described the case of a patient with unfavorable smile aesthetics and the presence of “black spaces” (initially verified through periapical radiographs) at a distance of 9.5 mm between the contact point and the alveolar bone crest, and between the central and lateral incisors. In the face of clinical measurements, a distance of 5.5 mm was observed from the point of contact to the tip of the papilla. Using periapical radiography, the distance from the point of contact to the bone crest was seen to remain the same after reconstructive surgery (papillary and prosthetic restorative treatment), although the final distance from the point of contact to the tip of the papilla was 0. The final aesthetic result of this case report was satisfactory, especially regarding the elimination of “black space.” Chang2, evaluating the distance from the ridge crest to the point of contact in periapical radiographs, observed 6.19 mm ± 0.91 mm and 5.24 mm ± 0.95 mm in the group with and without papillary recession, respectively. The differences between the groups were statistically significant. The measurements found in this study were lower than those reported by Chang2. However, this discrepancy may have occurred because the evaluative method used in this study was CBCT rather than periapical radiography.
When compared with periapical radiographs, CBCT images provide better image quality and more precise measurements because of the three-dimensional representation of structures. In addition, a specific software tool allows the scanner to generate measures in fractions of millimeters. This calibrating tool was used for all assessments thereby resulting in precise linear measurements between the bone crest and contact points in coronal and sagittal planes.
Chun et al.18 used a radiopaque material in the tip height of the bone crest to determine the position of this structure in the occlusal plane of the CT scan. The location of the bone crest was transferred to the study casts, and the distance from the bone crest to the tip of the papilla was measured by means of a digital caliper. The mean value found in male patients was 5.12 mm ± 1.24 mm for maxillary papillae and 4.05 mm ± 0.66 mm in mandibular papillae. In female patients, the mean distance from the ridge crest to the tip of the papilla was 4.66 mm ± 0.81 mm and 3.82 mm ± 1.00 in the maxillary and mandibular quadrants, respectively. There was no significant difference between the maxillary and mandibular groups in either gender. Methodological differences between studies justify the difference in the results.
The presence of papillae is fundamental to the aesthetics of the smile, and several factors, including orthodontic movement, may contribute to their alteration. Most studies evaluating papilla height (obtained clinically or by means of two- or three-dimensional images) were found to report results below 5 mm – a positive fact that favors the pleasing aesthetics of the smile. However, differing methods have been presented and described in the literature to measure the height of interdental papillae. Thus, an effort to standardize measuring techniques and study methodologies is required to achieve consistent and significant scientific evidence and results.
CONCLUSION
In our sample of maxillary incisors, papilla height changed little as a result of orthodontic therapy. The results described in this paper suggest that both study models and CBCT adequately allow researchers to evaluate orthodontic treatment-related changes to incisive papilla height, but CBCT yielded more precise measurements when compared with study casts.
REFERENCES
1. Holmes CH. Morphology of the interdental papillae. J Periodontol. 1975;36:455-60. [ Links ]
2. Chang LC. Assessment of parameters affecting the presence of the central papilla using a non-invasive radiographic method. J Periodontol. 2008;79:603-9. [ Links ]
3. Prato GP, Rotundo R, Cortellini P, Tinti C, Azzi R. Interdental papilla management: a review and classification of therapeutic approaches. Int J Periodontics Restorative Dent. 2004;24:246-55. [ Links ]
4. Cardaropoli D, Re S. Interdental papilla augmentation procedure following orthodontic treatment in a periodontal patient. J Periodontol. 2005;76:655-61. [ Links ]
5. Burke S, Burch J, Tetz J. Incidence and size of pretreatment overlap and posttreatment gingival embrasure space between maxillary central incisors. Am J Orthod Dentofacial Orthop. 1994;105:506-11. [ Links ]
6. Tarnow D, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995-6. [ Links ]
7. Inocencio F, Sandhu HS. Interdental papilla reconstruction combining periodontal and orthodontic therapy in adult periodontal patients: a case report. J Can Dent Assoc. 2008;74:531-5. [ Links ]
8. Bueno MR, Estrela C, Azevedo BC, Brugnara JRA, Azevedo JR. Tomografia computadorizada cone beam: revolução na odontologia. Rev Assoc Paul Cir Dent. 2007;61:325-8. [ Links ]
9. Garib DG, Raymundo JRR, Raymundo MV, Raymundo DV, Ferreira SN. Tomografia computadorizada de feixe cônico (cone beam): entendendo este novo método de diagnóstico por imagem com promissora aplicabilidade na ortodontia. R Dental Press Ortodon Ortop Facial. 2007;12:139-56. [ Links ]
10. Nakajima A, Sameshima GT, Arai Y, Homme Y, Shimizu N, Dougherty SH. Two-and three-dimensional orthodontic imaging using limited cone beam-computed tomography. Angle Orthodontist. 2005;75:895-903. [ Links ]
11. Cohen B. Pathology of the interdental tissues. Dent Pract Dent Rec. 1959;9:167. [ Links ]
12. Vasconcelos KF, Evangelista KM, Rodrigues CD, Estrela C, De Sousa TO, Silva MAG. Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol. 2012;41:64-9. [ Links ]
13. Beagle JR. Surgical Reconstruction of the interdental papilla: case report. Int J Period Restor Dent. 1992;12:144-51. [ Links ]
14. Kurth JR, Kokich VG. Open gingival embrasures after orthodontic treatment in adults: prevalence and etiology. Am J Orthod Dentofacial Orthop. 2001;120:116-23. [ Links ]
15. Wu YJ, Tu YK, Huang SM, Chan CP. The influence of the distance from the contact point to the crest of bone on the presence of the interproximal dental papilla. Chang Gung Med J. 2003;26:822-8. [ Links ]
16. Carnio J. Surgical reconstruction of interdental papilla using as interposed subepithelial connective tissue graft: A case report. Int J Period Restor Dent. 2004;24:31-7. [ Links ]
17. Zetu L, Wang HL. Management of inter-dental/inter-implant papilla. J Clin Periodontol. 2005;32:831-9. [ Links ]
18. Chun YS, Lee SK, Wikesjo UM, Lim WH. The interdental gingiva, a visible guide for placement of mini-implants. Orthod Craniofac Res. 2009;12:20-4. [ Links ]
19. Becker W, Gabitov I, Stepanov M, Kois J, Smidt A, Becker BE. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010;12:1-8. [ Links ]
 Corresponding Author:
Corresponding Author:
Prof. Carlos Estrela
Centro de Ensino e Pesquisa Odontológica do Brasil (CEPOBRAS)
Rua C–245, Quadra 546, Lote 9, Jardim América
CEP 74290-200 – Goiânia, GO, Brazil
E-mail:estrela3@terra.com.br













