Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.19 no.36 Canoas Jan./Jun. 2013
ORIGINAL ARTICLE / ARTIGO ORIGINAL
Molar incisor hypomineralization: three case reports and discussion of etiology, diagnosis, and management strategies
Hipomineralização de molar e incisivo: três relatos de caso e discussão sobre etiologia, diagnóstico e estratégias de tratamento
Renata Schlesner OliveiraI; Deisi Fátima DaminI; Luciano CasagrandeII; Jonas Almeida RodriguesII
I Graduated in Dentistry at Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil
II Professors of Pediatric Dentistry at Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil
ABSTRACT
The aim of this article including three case reports is to briefly discuss the etiology, diagnosis, and treatment of patients with molar incisor hypomineralization. In all three cases presented, the etiology was related to systemic factors that occurred in the first year of life, especially respiratory deficiency and episodes of high fever. Diagnosis was based on clinical examination of specific characteristics such as changes in color and opacity and loss of tooth structure. Treatment decisions were made according to severity of hypomineralization in each patient, ranging from expectant management/follow-up to esthetic restoration of permanent incisors. Our reports suggest that molar incisor hypomineralization occur predominantly in children with a history of respiratory deficiency and episodes of high fever in the first year of life. Early diagnosis is usually determined by visual examination and treatment decision is dependent on condition severity.
Keywords: Case Reports, Tooth Demineralization, Etiology, Diagnosis.
RESUMO
O objetivo deste artigo, que inclui três relatos de caso, é discutir brevemente a etiologia, o diagnóstico e as estratégias de tratamento de três pacientes com hipomineralização de molares e incisivos. Nos três casos apresentados, a etiologia estava relacionada a fatores sistêmicos que ocorreram durante o primeiro ano de vida, especialmente deficiência do sistema respiratório e episódios de febre alta. O diagnóstico foi realizado com base em exame clínico de características específicas como mudanças na cor e opacidade e perda de estrutura dentária. Decisões de tratamento foram tomadas de acordo com a severidade da hipomineralização em cada paciente, variando desde conduta expectante/acompanhamento até a restauração estética de incisivos permanentes. Nossos relatam indicam que a hipomineralização de molares e incisivos pode ocorrer, predominantemente, em crianças com história de deficiência respiratória e episódios de febre alta durante o primeiro ano de vida. O diagnóstico inicial normalmente é determinado pelo exame visual, e a decisão de tratamento dependerá da severidade da hipomineralização.
Palavras-chave: Relatos de Caso, Desmineralização do Dente, Etiologia, Diagnóstico.
INTRODUCTION
Molar incisor hypomineralization (MIH) is defined as a developmentally derived dental defect that involves hypomineralization of one to four first permanent molars (FPM) and is frequently associated with similarly affected permanent maxillary and mandibular incisors 1,2. Clinically, MIH may present as discrete, opaque lesions, ranging from white to yellow-brown, distinct from the more diffuse linear opacities usually observed in fluorosis. MIH may be associated with post-eruptive enamel loss, making it potentially difficult to distinguish from enamel hypoplasia 3.
Affected teeth can present high sensitivity to temperature variations and tooth brushing, even when the enamel is clinically intact 1. MIH may co-occur with many dental problems, including fast development of carious lesions and repeated need for dental treatment 4-7. The condition has also been referred to as a risk factor for dental caries in populations with a low prevalence of this problem 7.
Different prevalence rates have been reported for MIH in various areas of the world, ranging from 2.5 to 40.2% 7-10. In Brazil, the prevalence of MIH is considered high, varying from 19.8 7 to 40.2% 10. These figures underscore the importance of better investigating this type of defect.
Despite of the multifactorial etiology of hypomineralization, systemic conditions are known to be usually involved 11-13. Several factors have been related to the origin of MIH, e.g., problems during pregnancy, pre-term delivery, cyanosis, diseases in early childhood (e.g., chickenpox, otitis, urinary infections, and tonsillitis), high fever, gastrointestinal disorders (e.g., celiac disease), and the frequent use of antibiotics 4,14-17. The relevance of each event is difficult to establish, as many can happen more than once in early childhood 7. Also, the literature refers to the first years of life as a critical period for crown formation of FPM and incisors, and therefore more likely at risk for MIH 18.
The aim of this article was to report three cases of MIH in patients treated at the Pediatric Dentistry Clinic of Federal University of Rio Grande do Sul, Brazil, and to briefly discuss the etiology, diagnosis and treatment adopted in the three cases.
DESCRIPTION OF CASES
Three young patients and their parents were referred to the University's Pediatric Dentistry Clinic. MIH was diagnosed based on medical history and intraoral clinical examination. Investigation of medical history focused on their first year of life. Clinical examination revealed enamel hypomineralization of the central maxillary incisors (except in case no. 3) and of all first molars. All parents were informed about the diagnosis of MIH in their children, possible etiologies, and the importance of a regular follow-up of affected teeth. Oral hygiene with fluoridated toothpaste was instructed and reinforced to all children and their mothers. The characteristics of each case are described in detail below.
Case nº. 1
A 7-year-old girl whose mother denied any complication during pregnancy had experienced high fever for 3 consecutive days due to asthma at 6 months of age. Two months later, the child had chickenpox. Figure 1 shows hypomineralization affecting the maxillary incisors, mandibular incisors, and first permanent molars. Non-cavitated inactive carious lesions were also observed on occlusal surfaces. For esthetic reasons, resin restoration was indicated to treat the maxillary central incisors, and regular followup was indicated for the molars.

Case nº. 2
A 9-year-old boy whose mother denied any complication during pregnancy had had a flu with high fever for 1 week at 1 year of age. Hypomineralization was observed in the maxillary incisors, mandibular lateral incisors, and first permanent molars (Figure 2). Because the patient did not have any esthetic complaint, no restorative procedure was indicated.

Case nº. 3
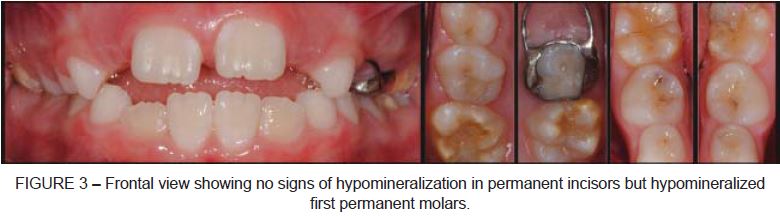
A 7 year-old girl whose mother denied any complication during pregnancy required nebulization due to asthma attacks when she was 3 months old. Subsequently, at 6 months of age, the child was hospitalized with high fever due to intestinal infection. Even though no clinical signs of hypomineralization were present in permanent incisors, visual examination revealed alterations affecting the first permanent molars (Figure 3).
DISCUSSION
The literature suggests several etiological factors for the development of MIH, mostly related to systemic factors 11-13 and also pre-, peri-, and postnatal complications 19. The problems most commonly associated with MIH are cyanosis, childhood diseases (measles, chickenpox, mumps), gastrointestinal disease, respiratory problems (asthma), malnutrition, low birth weight, ear infections, and prematurity 4,14-16. In addition to these factors, there are reports of genetic mechanisms 20,21 involved as causative agents for MIH.
The cases described in this report showed features known to be implicated in the development of MIH. Medical history investigation revealed the occurrence of gastrointestinal disease (case no. 3), respiratory problems (asthma, cases no. 1 and 3), childhood disease (chickenpox, case no. 1), and high fever lasting for at least 3 days (case no. 1). In all patients, these events occurred in the first year of life, which is considered a critical period for the development of MIH 18. These findings suggest that these permanent teeth (incisors and first molars) were probably going through the process of maturation of the organic matrix when the cited systemic events occurred 22. Defects occurring at this stage produce tissues with a large amount of organic matter and a lower mechanical strength when compared with normal enamel 23, favoring the development of quantitative defects or hypomineralization.
MIH diagnosis in the patients here described was made based on verification of clinical characteristics already described in the literature 3, such as opaque yellow-brown discoloration, combined with medical history information reported by the parents.
Different treatment approaches are indicated for MIH depending on severity of hypomineralization or tissue loss 4,5. When no symptoms are reported (as in cases no. 2 and 3), a strict follow-up is enough but extremely important, as enamel defects may facilitate the development of carious lesions 1,5,24. When sensitivity is present, resin or glass ionomer sealants can be placed on occlusal surfaces and topical fluoride can be applied. Finally, when esthetic complaints are present (as in case no. 1), restoration with composite resin should be considered as the first treatment option for permanents incisors.
In patients showing loss of tooth structure, more extensive restorative treatment may be necessary. The use of bonding systems combined with composite resin on occlusal surfaces may be a good option in these cases. However, due to the poor adhesion of restorative material to hypomineralized tissue, glass ionomer cement should be the material of choice. Glass ionomer cements can also be placed on the occlusal surfaces of hypomineralized molars not completely erupted.
More severe cases require more invasive treatments. Semi-permanent restorations using stainless steel crowns or adhesive-retained metal castings are options to be considered. Extraction of affected molars, combined with orthodontic treatment, is another option, especially when a poor long-term prognosis is expected 24.
CONCLUSION
Hypomineralization of molars and incisors occurs predominantly in children with a history of systemic complications in the fi rst year of life, especially respiratory problems and episodes of high fever. Diagnosis is usually determined based on visual examination (opaque and yellow-brown lesions) and previous medical history. Treatment will be dependent on hypomeralization severity. Early, accurate diagnosis and knowledge of treatment options available for MIH are fundamental to minimize sequelae caused by MIH.
REFERENCES
1. Weerheijm KL, Jalevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35(5):390-1. [ Links ]
2. Lygidakis NA, Dimou G, Marinou D. Molar-incisor-hypomineralisation (MIH). A retrospective clinical study in Greek children. II. Possible medical aetiological factors. Eur Arch Paediatr Dent. 2008;9(4):207-17. [ Links ]
3. Crombie FA, Manton DJ, Weerheijm KL, Kilpatrick NM. Molar incisor hypomineralization: a survey of members of the Australian and New Zealand Society of Paediatric Dentistry. Aust Dent J. 2008;53(2):160-6. [ Links ]
4. Jalevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002;12(1):24-32. [ Links ]
5. Leppaniemi A, Lukinmaa PL, Alaluusua S. Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res. 2001;35(1):36-40. [ Links ]
6. Muratbegovic A, Markovic N, Ganibegovic Selimovic M. Molar incisor hypomineralisation in Bosnia and Herzegovina: aetiology and clinical consequences in medium caries activity population. Eur Arch Paediatr Dent. 2007;8(4):189-94. [ Links ]
7. Da Costa-Silva CM, Jeremias F, de Souza JF, Cordeiro Rde C, Santos-Pinto L, Zuanon AC. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010;20(6):426-34. [ Links ]
8. Cho SY, Ki Y, Chu V. Molar incisor hypomineralization in Hong Kong Chinese children. Int J Paediatr Dent. 2008;18(5):348-52. [ Links ]
9. Wogelius P, Haubek D, Poulsen S. Prevalence and distribution of demarcated opacities in permanent 1st molars and incisors in 6 to 8-year-old Danish children. Acta Odontol Scand. 2008;66(1):58-64. [ Links ]
10. Soviero V, Haubek D, Trindade C, Da Matta T, Poulsen S. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol Scand. 2009;67(3):170-5. [ Links ]
11. Weerheijm KL, Groen HJ, Beentjes VE, Poorterman JH. Prevalence of cheese molars in eleven-year-old Dutch children. ASDC J Dent Child. 2001;68(4):259-62, 229. [ Links ]
12. Beentjes VE, Weerheijm KL, Groen HJ. Factors involved in the aetiology of molarincisor hypomineralisation (MIH). Eur J Paediatr Dent. 2002;3(1):9-13. [ Links ]
13. Crombie F, Manton D, Kilpatrick N. Aetiology of molar-incisor hypomineralization: a critical review. Int J Paediatr Dent. 2009;19(2):73-83. [ Links ]
14. Preusser SE, Ferring V, Wleklinski C, Wetzel WE. Prevalence and severity of molar incisor hypomineralization in a region of Germany – a brief communication. J Public Health Dent. 2007;67(3):148-50.
15. Kuscu OO CE, Sandalli N. The prevalence and etiology of molar incisor hypomineralization in a group of children in Istanbul. Eur J Paediatr Dent. 2008;9:139-44. [ Links ]
16. Whatling R, Fearne JM. Molar incisor hypomineralization: a study of aetiological factors in a group of UK children. Int J Paediatr Dent. 2008;18(3):155-62. [ Links ]
17. Laisi S, Ess A, Sahlberg C, Arvio P, Lukinmaa PL, Alaluusua S. Amoxicillin may cause molar incisor hypomineralization. J Dent Res. 2009;88(2):132-6. [ Links ]
18. Jalevik B, Noren JG. Enamel hypomineralization of permanent first molars: a morphological study and survey of possible aetiological factors. Int J Paediatr Dent. 2000;10(4):278-89. [ Links ]
19. William V, Messer LB, Burrow MF. Molar incisor hypomineralization: review and recommendations for clinical management. Pediatr Dent. 2006;28(3):224-32. [ Links ]
20. Brook AH, Smith JM. The aetiology of developmental defects of enamel: a prevalence and family study in East London, U.K. Connect Tissue Res. 1998;39(1-3):151-6; discussion 87-94. [ Links ]
21. Mathu-Muju K, Wright JT. Diagnosis and treatment of molar incisor hypomineralization. Compend Contin Educ Dent. 2006;27(11):604-10; quiz 11. [ Links ]
22. Suga S. Enamel hypomineralization viewed from the pattern of progressive mineralization of human and monkey developing enamel. Adv Dent Res. 1989;3(2):188-98. [ Links ]
23. Porto IM, Merzel J, de Sousa FB, Bachmann L, Cury JA, Line SR, Gerlach RF. Enamel mineralization in the absence of maturation stage ameloblasts. Arch Oral Biol. 2009;54(4):313-21. [ Links ]
24. Weerheijm KL. Molar incisor hypomineralization (MIH): clinical presentation, aetiology and management. Dent Update. 2004;31(1):9-12. [ Links ]
 Corresponding Author:
Corresponding Author:
Jonas Almeida Rodrigues
School of Dentistry (UFRGS)
Rua Ramiro Barcelos, 2492
CEP 90035-003
Porto Alegre, RS, Brazil
E-mail:jorodrigues@ufrgs.br













