Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.19 no.36 Canoas Jan./Jun. 2013
ORIGINAL ARTICLE / ARTIGO ORIGINAL
Soft tissue profile changes in class II patients treated with first bicuspid extraction
Alterações do perfil mole em pacientes portadores de classe II tratados com extrações de primeiros pré-molares
Darlene Ribeiro dos Santos GerzsonI; Danielle Volcato PrettoII; Luciane Quadrado ClossIII; Karina dos Santos MundstockIV
I MS in Orthodontics – ULBRA Canoas/RS
II Orthodontics – Private practice – Porto Alegre/RS
III PhD in Orthodontics – Head of Orthodontic Department – ULBRA Canoas/RS
IV PhD in Orthodontics – Adjunct Professor – UFRGS – Porto Alegre/RS
ABSTRACT
Objective: To assess soft tissue changes in the lip area after orthodontic treatment with first bicuspid extraction in 20 Angle class II patients. Methods: A total of 40 profile cephalograms were digitized and measured: 20 obtained at baseline and 20 after treatment. Eighteen landmarks were marked on the cephalograms and analyzed using the Radiocef software version 4.0 (Radio Memory Ltda.). Linear and angular measurements were used to analyze changes in upper and lower lip position. Statistical analysis included calculation of error. Pre- and post-treatment measurements were compared using the Student t test for paired samples. Results: Upper and lower lips showed a mean retrusion of 2 mm. There was a significant increase in the nasolabial angle, of 5.36°, leading to a decreased facial convexity. The upper lip angle (ULA) retruded -4.74°. Conclusions: Our findings suggest that treatment of class II patients including first bicuspid extraction result in small changes in the patients' facial profile (increased nasolabial angle and decreased upper lip angle).
Keywords: Profile, Face, Tooth Extractions, Lip, Orthodontics.
RESUMO
Objetivo: Avaliar mudanças nos tecidos moles da área labial decorrentes do tratamento ortodôntico com extrações de primeiros pré-molares em 20 indivíduos classe II de Angle. Material e métodos: Foram utilizadas 40 telerradiografias de perfil escaneadas, sendo 20 radiografias iniciais e 20 radiografias pós-tratamento. Dezoito pontos foram digitalizados sobre as telerradiografias e analisados utilizando o programa Radiocef 4.0 (Radio Memory Ltda.). Foram utilizadas medidas lineares e angulares para medir a variação da posição dos lábios dos indivíduos. Foi realizado cálculo de erro do método. Valores pré e pós-tratamento foram comparados entre si utilizando o teste t de Student para dados pareados. Resultados: A retrusão média dos lábios superior e inferior foi de 2 mm. Foi observado um aumento significativo do ângulo nasolabial de 5,36°, o que resultou em uma diminuição da convexidade facial. O ângulo do lábio superior (ULA) diminuiu 4,74°. Conclusão: Pode-se concluir que planejamentos envolvendo extração de primeiros prémolares em pacientes com maloclusão classe II resultam em uma pequena alteração da convexidade do perfil facial (aumento do ângulo nasolabial e diminuição do ângulo do lábio superior).
Palavras-chave: Face, Extração Dentária, Lábio, Ortodontia Corretiva.
INTRODUCTION
One of the primary objectives of orthodontic treatment is to improve facial esthetics through changes in soft tissues 1.Many orthodontists believe that extracting the four premolars to create space for incisor retraction decreases facial convexity. The relationship between retraction of maxillary and mandibular incisors and changes in lip position has been described in several studies, often pointing to a direct relationship between changes in incisor position and lip retrusion 2,3. Notwithstanding, some authors have identified other factors likely to contribute to soft tissue alterations, not necessarily related with changes in the position of anterior teeth 2.
The concept of beauty has changed over time and has been investigated by several authors. Consequently, different methods have been developed to analyze facial profiles and their relationship with the extraction of teeth. In 1998, James 4 compared the facial profile of patients treated with and without tooth extraction and concluded that the group treated with extraction showed a more balanced facial profile after treatment when compared with the group treated without extraction (before treatment, facial balance in the group treated with extraction was also considered poor). Wholley et al., in 2003, emphasized that the decision to extract teeth in orthodontic practice derives from several reasons and does not directly cause changes in lip position 5.
The objective of the present study was to assess soft tissue changes in the lip area after orthodontic treatment with first bicuspid extraction, using cephalometric analysis.
MATERIAL AND METHODS
A total of 20 profile cephalograms obtained before and after orthodontic treatment were analyzed. The following inclusion criteria were taken into consideration: white or black skin color; Angle class II malocclusion (first and second division); mesiobuccal cusp of the permanent maxillary first molar located on top or ahead of the mandibular first molar; no signs or symptoms in the temporomandibular joint; orthodontic treatment plan involving extraction of first bicuspids; patients in permanent dentition. Exclusion criteria were patients not diagnosed with Angle class II malocclusion, patients planning the extraction of other teeth, or not requiring extraction.
Mean age among patients was 23.5 years (range: 9-28 years). Eight patients were male and 12 were female.
The sample comprised patients treated by two specialists in orthodontics and facial orthopedics at their private clinics and patients treated in the Lato Sensu Graduate Program in Orthodontics at Universidade Luterana do Brasil (ULBRA), in Canoas, southern Brazil. Profile cephalograms were obtained before and after treatment with the Frankfurt horizontal plane parallel to the ground. Lip position on the cephalograms was defined as the position of lips at rest. All cephalograms were digitized using the Radiocef software version 4.0 (Radio Memory Ltda.).
A total of 18 landmarks were marked on the cephalograms for subsequent analysis of straight lines and angles on the software. In order to minimize errors, landmarks were marked twice by the same, previously calibrated examiner. The landmarks used in the present study (Figure 1) were based on cephalometric analysis landmarks widely used in the orthodontic literature 6-9:
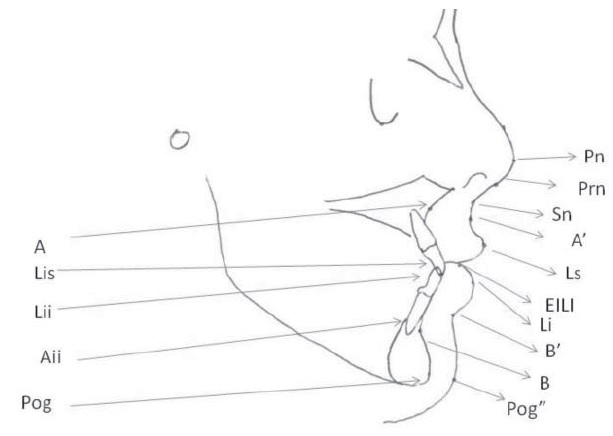
• Po: anatomical porion
• Or: orbitale – most inferior point of the left orbit
• Pog': soft pogonion – most anterior point of the chin contour
• Prn: nasal 's' – midpoint in the nose curvature
• Pn: nasal tip – most anterior point of the nose contour
• A': superior groove – point of greatest concavity between the upper lip and subnasale
• Ls: upper lip – most anterior point on the convexity of the upper lip
• Li: lower lip – most anterior point on the convexity of the lower lip
• B': inferior groove – point of greatest concavity between the lower lip and the soft pogonion
• Sn: subnasale – junction between the columella and the upper lip
• Stm: stomion – junction of the contour of upper and lower lips
• A: point A – point of greatest concavity in the maxilla contour
• B: point B – point of greatest concavity in the mentum contour
• Pog: pogonion – most anterior point of the mentum contour
• Aii: apex of maxillary incisor
• Lis: incisal edge of maxillary incisor
• Lii: incisal edge of mandibular incisor
• EILI : most interior point of the lower lip contour
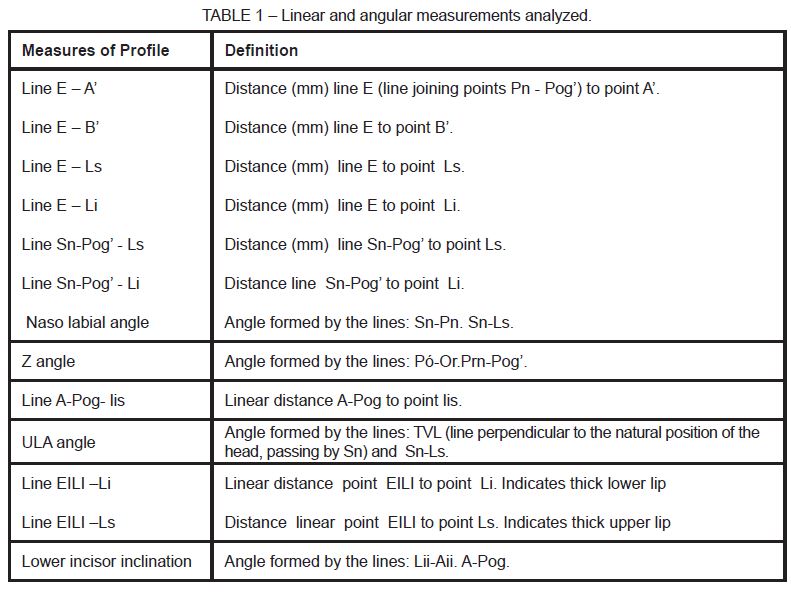
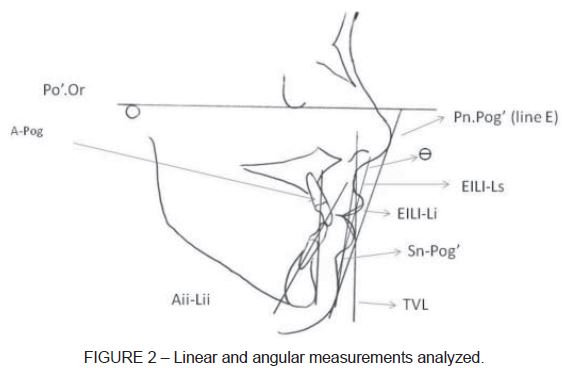
Landmarks were marked using the Radiocef software. Subsequently, previously defined linear and angular measurements were obtained as shown in Table 1 and Figure 2.
RESULTS
Profile cephalograms were marked twice to calibrate the examiner. The mean of the two measurements was used in statistical analysis, and the error between the two measurements was calculated using Student's t test for paired samples (Table 2).
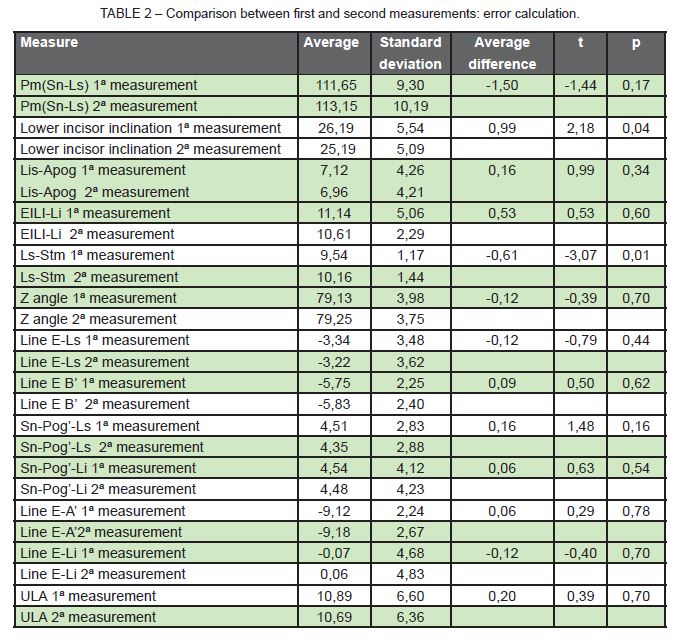
Results revealed that only mandibular incisor inclination and Ls-Stm showed significant differences between the fi st and second measurements. In the analysis of mandibular incisor inclination, the mean difference found between the two measurements was 0.99 mm, whereas for Ls-Stm, the mean difference was 0.61 mm. These two measurements were not included in statistical analysis.
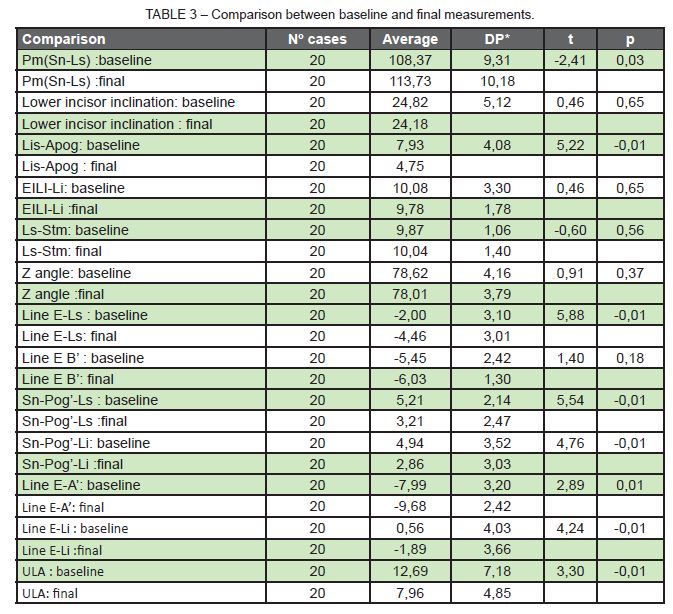
Normality of data was assessed using the Kolmogorov-Smirnov nonparametric test and revealed a normal distribution; as a result, a parametric test was employed. Data were processed and analyzed using the Statistical Package for the Social Sciences (SPSS) version 10.0 (Table 3).
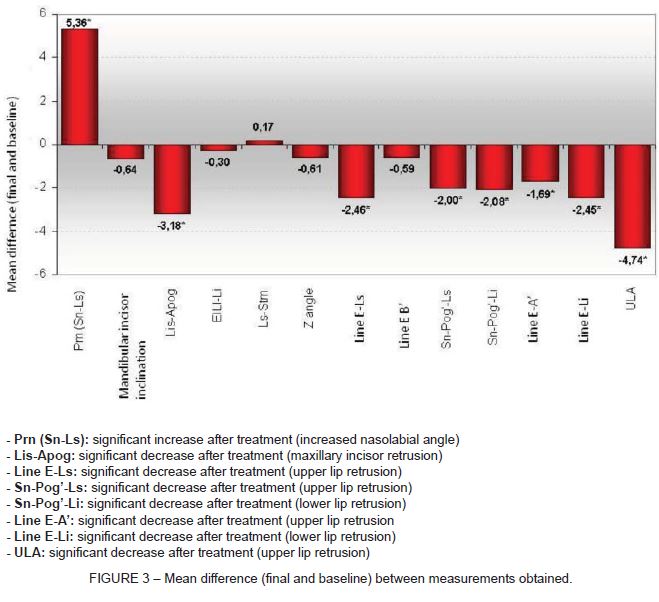
Results of the Student's t test for paired samples (Table 3 and Figure 3) revealed statistically significant differences between baseline and final values for the following measurements:
DISCUSSION
A large number of orthodontists focus their attention primarily on horizontal lip position. Merrifield 7 analyzed facial esthetics in a sample of 120 patients with and without treatment. That author modified Holdaway's H line and created the Z angle, formed by a line extending from the soft pogonion, passing through the most protruded point of the lower lip, and forming an angle with the Frankfurt plane 10. In our sample, this angle was also assessed, but did not show statistically significant changes after treatment.
Caplan, in 1997 2, used different cephalometric measures, including the ones mentioned in the present study, and concluded that mandibular incisor retraction is directly related with retrusion of the lower lip. In other words, we could say that changes in the position of mandibular incisors can predict changes in the lower lip.
The objective of orthodontic treatment is to achieve facial balance through dental stability and esthetics. In the present study, changes in antero-posterior direction were observed in the position of both upper and lower lips. Eight of the 13 measures assessed in the present study showed statistically significant differences when comparing baseline and final values. It was also possible to observe a decrease in facial profile convexity as a result of lower and upper lip retrusion. In addition, a slightly more pronounced linear reduction was observed in the lower lip (-2.44 mm) when compared with the upper lip (-2.23 mm). Another study conducted by Rodrigues et al. 11 found that, for every 1 mm of movement in the maxillary incisor, the upper lip moved 0.81 mm in the same direction, and that, for every 1 mm of movement in the mandibular incisor, the lower lip moved 0.66 mm in the same direction. Final results reported by those authors revealed a slight change in facial profile, which is in line with the findings of the present study 11. Bravo 12 assessed patients treated with first bicuspid extraction and observed that the upper and lower lips retruded 3.4 and 3.8 mm, respectively, in relation to the Ricketts E line. These results are similar to the ones here reported, which also suggested a significant retrusion of upper and lower lips in relation to the same line. A systematic review conducted to assess changes in perioral tissues following extraction of four premolars in adult patients concluded that the upper and lower lips retruded and the nasolabial angle increased after extraction. Upper lip retrusion ranged from 2 to 3.2 mm, and upper lip, from 2 to 4.5 mm in that study. These data corroborate our findings of 2.23 mm of retrusion in the upper lip and 2.26 mm in the lower lip 13.
Tadic and Woods 1 found an increase in the nasolabial angle of 3.65° and concluded that the depth of the curve of the upper lip and the nasolabial angle are more negatively affected in treatments involving bicuspid extraction. In our study, there was an increase of 5.36° in the nasolabial angle, providing clinical evidence of upper lip retrusion. Finnoy et al. 14 assessed changes in the facial profile of 30 patients with class II malocclusion treated with extraction of the four bicuspids and also found changes in the nasolabial angle, even though the result found by those authors was 6.5°, slightly higher than our value.
A mean decrease of 4.74° was observed in the ULA angle, suggesting upper lip retrusion. According to Arnett et al. 8, upper lip retrusion is associated with a decreased ULA angle. This angle changes as the maxillary incisor moves, and it should therefore be seriously taken into consideration in orthodontic treatment planning.
James 4 assessed changes in the profile of patients treated with and without bicuspid extraction. They found a difference of 5.27° in the Z angle between the two groups assessed, with patients not treated with extraction showing a higher angular result than the groups treated with extraction. Conversely, in the present study, changes in the Z angle were not statistically significant. The distance between the lower lip and line E was also assessed by James, who found -2.58 mm in the group treated with extraction, in line with the results here reported (-2.45 mm).
Leonardi et al. 13 recommend the analysis of two other important landmarks related to soft tissue changes, namely, presence of incisor crowding and anchorage loss. These factors can affect facial convexity, as they require a lower degree of retrusion. These two landmarks were not included in the present analysis.
According to Tadic and Woods 1, the complex nature of the musculoskeletal functions of the nose and upper lip contribute to the occurrence of changes in the upper lip area after treatments involving bicuspid extraction. Patients with a convex profile are less prone to presenting changes in lip position after orthodontic treatment involving bicuspid extraction. This probably explains why the results of the present study did not show major changes in the soft tissue profile of patients.
CONCLUSIONS
Our findings allow was to draw the following conclusions:
1 - There was a significant increase in the nasolabial angle, of 5.36°, leading to a decreased facial convexity.
2 - Maxillary incisors retruded -3.18 mm, and upper lips -2.23 mm. The lower lip retracted -2.26 mm.
3 - The upper lip angle (ULA) retruded -4.74°.
It is important to highlight that, in our sample, even though lip retrusion was observed after bicuspid extraction, changes in facial esthetics did not seem to be clinically relevant.
REFERENCES
1. Tadic N, Woods M. Incisal and soft tissue effects of maxillary premolar extraction in class II treatment. Angle Orthod. 2007;77(5):808-15. [ Links ]
2. Caplan M, Shivapuja P. The effect of premolar extractions on the soft-tissue profile in adult African American female. Angle Orthod. 1997;67(2):129-36. [ Links ]
3. Reichenbach RC, Takahashi T, Montero SR. Alterações do lábio inferior decorrentes do tratamento ortodôntico associado a extrações de quatro pré-molares,nos casos de class II divisão 1 de Angle. J. Bras Orthodon Ortop Facial. 2005;10(55):59-68. [ Links ]
4. James R. A comparative study of facial profiles in extraction and nonextraction treatment. Am J Orthod Dentofac Orthop. 1998;114(3):265-76. [ Links ]
5. Wholley C, Woods M. The effects of commonly prescribed premolar extraction sequences on the curvature of the upper and lower lips. Angle Orthod. 2003;73(4):386-94. [ Links ]
6. Downs WB. Analysis of the dentofacial profile. Angle Orthod. 1956;26(4):191-212. [ Links ]
7. Merrifield L. The profile line in the critically evaluating facial esthetics. Angle Orthod. 1981;51:115-50. [ Links ]
8. Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr, et al. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofac Orthop. 1999;116(3):239-52. [ Links ]
9. Erbay E, Caniklioglu C, Erbay S. Soft tissue profile in Anatolian Turkish adults: part I. Evaluation of horizontal lip position using different soft tissue analyses. Am J Orthod Dentofac Orthop. 2002;121(1):57-63. [ Links ]
10. Loi H, Nakata S, Nakasima A, Counts A. Effect of facial convexity on antero- posterior lip positions of the most favored Japanese facial profiles. Angle Orthod. 2005;75(3):326-32. [ Links ]
11. Rodrigues M, Vilella O, Mucha J. Alterações dos tecidos moles decorrentes do tratamento ortodôntico. Ortod Gaucha. 1999;3(1):24-32. [ Links ]
12. Bravo L. Soft tissue facial profile changes after orthodontic treatment with four premolars extracted. Angle Orthod. 1994;64(1):31-42. [ Links ]
13. Leonardi R, Annunziata A, Licciardello V, Barbato E. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion: a systematic review. Angle Orthod. 2010;80:211-6. [ Links ]
14. Finnoy J, Wisth P, Boe O. Changes in soft tissue profile during and after orthodontic treatment. Eur J Orthod. 1987;9:68-78. [ Links ]
 Corresponding Author:
Corresponding Author:
Darlene Ribeiro dos Santos Gerzson
Rua Dona Laura, 87/506
CEP 90430-091, Porto Alegre, RS
Brazil
E-mail:Dra.darleneribeiro@hotmail.com













