Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.19 no.36 Canoas Jan./Jun. 2013
CASE REPORT / RELATO DE CASO
Endodontic material diffusion in the pathogenesis of maxillary sinus aspergillosis
Patogênese da aspergilose do seio maxilar associada à difusão de material endodôntico
Stéfano FlorenzanoI; Larissa Santana Arantes EliasII; Angélica Ferreira Oton LeiteII; Clóvis SilvaIII; Carlos EstrelaIV; Elismauro Francisco MendonçaV
I Department of Stomatology, Dental School, Federal University of Goiás (UFGO), Goiânia, GO, Brazil
II Graduate students at the Dental School of UFGO, Goiânia, GO, Brazil
III DDS, works at the Cancer Hospital, Goiânia, GO, Brazil
IV DDS, MSc, PhD, Chairman and Professor of Endodontics at UFGO, Goiânia, GO, Brazil
V DDS, MSc, PhD, Chairman and Professor of Oral Pathology at UFGO, Goiânia, GO, Brazil
ABSTRACT
One undesirable sequela of root canal treatment is the overextension of endodontic material into the maxillary sinus, which may represent a risk factor for maxillary sinus aspergillosis (MSA). Diverse clinical presentations of aspergillosis have been reported and they vary depending on the immune status of the host. The noninvasive form called Aspergillus mycetoma occurs mostly in healthy people. This report describes a case of MSA associated with root canal overfilling in a 27-year-old healthy man. The patient had been asymptomatic for 6 years after root canal treatment. Radiography revealed a diffuse radiopaque mass inside the left maxillary sinus, with radiolucent areas near the cortical bone of the maxillary sinus. Computed tomography (CT) showed the presence of material with a density similar to that of soft tissue. Imaging findings suggested that the calcification filled the left maxillary antrum, without expansion or bone destruction. The lesion was removed, and microscopic examination of the specimen revealed an inflammatory process with numerous dichotomized fungal structures (compatible with Aspergillus sp.). Histopathological features were compatible with aspergillosis. Treatment consisted of surgery and adjunctive anti-fungal therapy with itraconazole. Clinical and radiographic follow-up revealed no recurrence of the lesion.
Keywords: Aspergillosis, Endodontic Treatment, Material Diffusion, Maxillary Sinus.
RESUMO
Uma sequela indesejável do tratamento endodôntico é a extrusão do material obturador no seio maxilar, o que pode representar um fator de risco para desenvolvimento da aspergilose do seio maxilar (ASM). Diversas apresentações clínicas da ASM têm sido relatadas e variam de acordo com estado imunológico do hospedeiro. A forma não invasiva Aspergillus mycetomaocorre principalmente em pessoas saudáveis. Este estudo descreve um caso clínico de ASM associada à sobreextensão do tratamento endodôntico em paciente do gênero masculino, 27 anos. O paciente estava assintomático durante 6 anos após concluído o tratamento endodôntico. A radiografia revelou uma massa radiopaca difusa no interior do seio maxilar esquerdo, com áreas radiolúcidas perto do osso cortical do seio maxilar. A tomografia computadorizada (TC) evidenciou material com uma densidade semelhante à do tecido mole. Os achados radiográficos sugerem calcificação preenchendo o antro maxilar esquerdo, sem expansão ou destruição óssea. A lesão foi removida e a análise microscópica revelou processo inflamatório com numerosas hifas dicotomizadas compatível com o Aspergillus sp. O tratamento consistiu em cirurgia e terapia antifúngica adjuvante com itraconazol. O acompanhamento clínico e radiográfico não revelou recorrência da lesão.
Palavras-chave: aspergilose, tratamento endodôntico, difusão de material, seio maxilar.
INTRODUCTION
One possible unpleasant occurrence after root canal treatment is the overextension of endodontic materials (sealer, gutta-percha) into the maxillary sinus, a factor that may cause maxillary sinus aspergillosis (MSA) 1-5.
Several clinical presentations of aspergillosis have been reported, and they vary depending on the immune status of the host. The noninvasive form called Aspergillus mycetoma (aspergilloma) or fungus ball occurs mostly in healthy individuals. It has been suggested that the extrusion of root canal obturation materials into the maxillary sinus may predispose a patient to noninvasive aspergillosis 2. Endodontic materials containing zinc oxide are considered to cause growth of Aspergillus fumigatus and may allow for its proliferation and metabolism 2,4-9. Foreign materials embedded in vital tissues produce an inflammatory reaction which persists until their elimination 8.
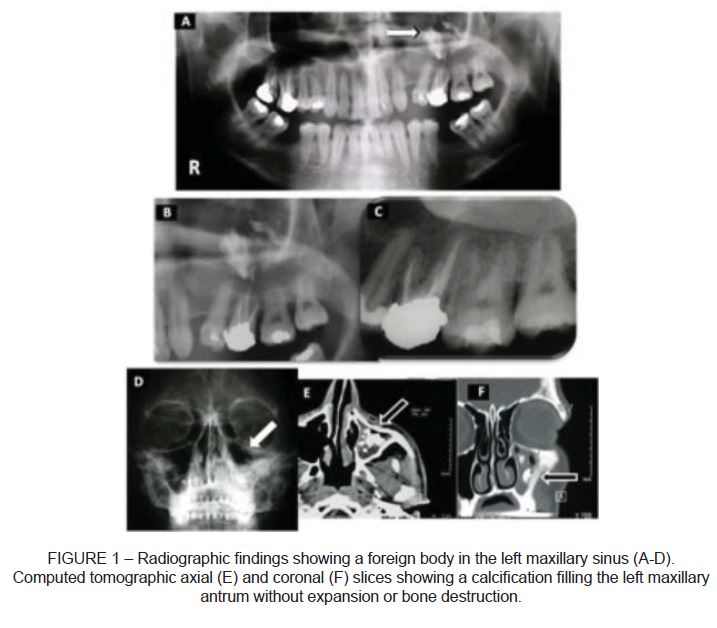
Radiographically, the isolated finding of a dense opaque foreign-body reaction in the maxillary sinus is considered a characteristic finding of MSA 4. Panoramic radiographs usually show a radiopaque mass in the maxillary sinus involved. The characteristic presentation in computed tomography (CT) scans includes a calcified mass, with heterogeneous opacities typically associated with radiopacity of metallic appearance involving the maxillary sinus 10,11.
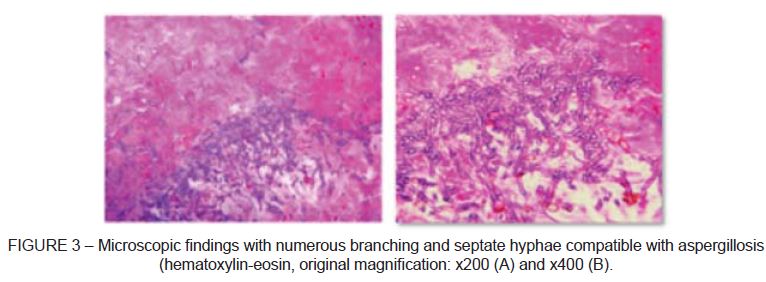
Microscopic findings of MSA show varying numbers of septate hyphae that branch at a characteristic 45° angle and conidiophores typical of Aspergillus. These hyphae show a tendency to invade adjacent small blood vessels, the occlusion of which often results in a pattern characteristic of necrosis. An intense inflammatory response is also present, with lymphocytes, plasma cells, epithelioid cells, and giant cells 12.
This study discusses the features of MSA in a young healthy male patient caused by overfilling of root canal material.
CASE REPORT
A 27-year-old healthy man with no medical history of systemic disease or allergic phenomena, who presented an unusual finding in the left maxillary sinus on a routine radiograph, was referred to the Department of Oral Surgery at the Cancer Hospital, Goiânia, Brazil. The patient had been asymptomatic for 6 years after root canal treatment and had had no history of traumatic dental injury. Extraoral and intraoral examinations showed no pathosis.
Panoramic radiograph revealed a diffuse radiopaque mass inside the left maxillary sinus, with radiolucent areas near the cortical plate of the maxillary sinus (Figure 1). A CT scan with multiplanar reconstruction based on axial, coronal, and sagittal slices was requested to obtain further details. The scan showed the presence of a material with a density similar to that of soft tissue. It also suggested a calcification filling the left maxillary antrum, without expansion or bone destruction (Figure 1). Even though there was no evidence of root canal overfilling on the periapical radiograph in the present case, previous endodontic treatment was the only event referred by the patient in association with the clinical findings.
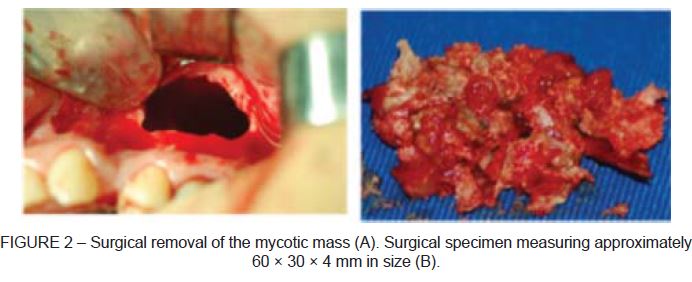
Based on radiographic findings, the diagnostic hypothesis of maxillary sinus disease of fungal etiology was raised. The patient was referred to the Cancer Hospital for surgical removal of the lesion. The surgical specimen measured approximately 60 x 30 x 4 mm in size (Figure 2) and was sent for histopathological examination. Microscopic examination revealed an inflammatory process with numerous dichotomized fungal structures, suggestive of Aspergillus sp. (Figure 3).
Treatment consisted of surgery and adjunctive anti-fungal therapy with itraconazole (100 mg) for 60 days. Clinical and radiographic follow-up revealed no recurrence of the lesion over 2 years. Concomitant to the anti-fungal treatment, the patient was advised to seek assistance for retreatment of the first maxillary molar.
DISCUSSION
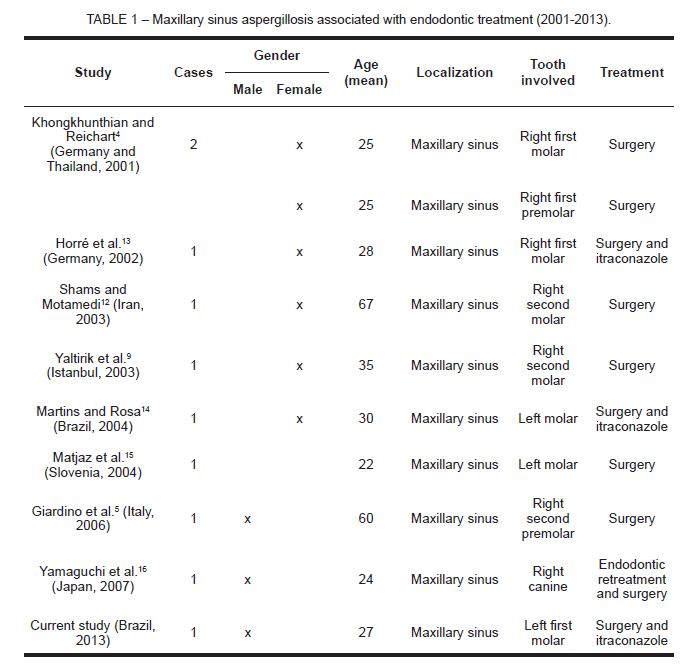
MSA is an uncommon condition, but an increase in aspergillosis associated with iatrogenic errors in endodontics has been reported over the past 10 years (Table 1). Root canal treatment with overextension of root canal sealer into the sinus has been suggested as the main etiological factor for MSA in healthy patients 2. Conversely, in immunosuppressed patients, aspergillosis is common and is present as multiorgan disease 17.
According to Khongkhunthian & Reichart 4, in non-immunocompromised patients, aspergillosis of the paranasal sinuses is a relatively rare opportunistic infection. Clinically, it can be divided into non-invasive, invasive, and allergic variants. The noninvasive form called Aspergillus mycetoma, or aspergilloma, or fungus ball, occurs mostly in healthy people. Usually only one sinus, especially the maxillary antrum, is affected, either symptomatically or asymptomatically. A typical, characteristic radiographic feature is the single finding of a densely opaque foreign-body reaction in the maxillary sinus 18. These foreign-bodies, concrements, or antroliths are usually in the center or near the orifice of the maxillary sinus. The invasive form of Aspergillus infection in immunocompromised patients occurs in the lung tissue via blood vessels and causes necrotic bronchopneumonia. Finally, the allergic form was first described by Katzenstein et al. 19. Symptoms are the same as those of allergic bronchitis.
Allergic bronchopulmonary aspergillosis usually affects young adults with a history of asthma and intranasal polyps. Clinical outcomes include sinus obstruction and chronic parasinusitis (as also observed in the noninvasive form). The allergic form does not respond to conventional medical management 4.
Particles of endodontic cement in the sinus may cause interactions resulting in inflammation and blocking of ciliary movement, creating favorable conditions for Aspergillus growth 20. Extrusion does not always cause MSA, as systemic and local conditions differ across patients 16. In our particular case, diffusion of the endodontic sealer was believed to be the main etiological factor in the development of the fungal infection lesion. The patient did not have any systemic conditions, e.g., diabetes, was not under long-term treatments (antibiotic or cortisone usage), radio or chemotherapy, immunosuppressive treatments, and did not have any immunodeficient disease that might favor fungal infections 7.
According to our patient, symptoms started with mild nasal obstruction after endodontic treatment. Indeed, mycotic sinusitis may develop many years after endodontic treatment in a chronic, non-painful form, making early detection practically impossible 20. Diagnosis is often made (in asymptomatic forms) after a routine panoramic radiograph obtained during dental treatment 2, based on the single, characteristic finding of a densely opaque foreign-body in the maxillary sinus 4.
Some authors consider MSA associated with highly radiodense material to be a consequence of overfilling of teeth endodontically treated with materials containing zinc oxide 2,6,7. Root canal cements can facilitate Aspergillus infection, and studies have shown that zinc oxide considerably accelerates the growth of different species of this fungus 7,14,21-23. Thus, it is essential to know the anatomical relationship between the maxillary sinus floor and the root tips of maxillary posterior teeth in the preoperative treatment planning of maxillary posterior teeth 23. Kopp et al. 22 reported that more than 50% of cases of MSA were associated with the extrusion of endodontic obturation materials. Ross 21 showed that Aspergillus fumigatus required materials such as zinc for its proliferation and metabolism.
Studies have suggested that overextension of root canal cements containing zinc oxide should be avoided 14,23. Given the probable correlation between zinc oxide and mycetoma, cases showing close proximity between the floor of the maxillary sinus and maxillary teeth should be carefully managed 20. The teeth in closest contact with the sinus wall (antral teeth) are the first and second molars and the second premolar 13,15,24,25. Many studies have demonstrated involvement of the first maxillary molar 4,9,12,13, and Yamaguchi et al. 16 has described a case of MSA involving the right canine. A female predominance was found in the studies 4,9,12,25, differently from the present case report, where a male patient was diagnosed with MSA. Conversely, our case is in accordance with the literature with respect to the typical age of patients diagnosed with aspergillosis.
With regard to the treatment of MSA, surgical removal of the mycotic mass is the approach most commonly recommended in the literature. Systemic anti-fungal therapy is also used and often recommended to complement the surgical procedure 26,27. Aspergillosis shows no tendency to recur after successful removal 2,25.
CONCLUSION
Extrusion of root canal sealer containing zinc oxide may be considered a risk factor for MSA and may have the effect of promoting the pathogenesis of this condition.
REFERENCES
1. Grigorin D, Bambule J, Delacretaz J. La sinusite maxilaire fungique. Dermatologica. 1979;159:180. [ Links ]
2. Beck-Mannagetta J, Necek D, Grasserbauer M. Solitary aspergillosis of maxillary sinus, a complication of dental treatment. Lancet. 1983;2:1260. [ Links ]
3. Loidolt D, Mangge H, Wilders-Truschnig M, Beaufort F, Schauenstein K. In vivo and in vitro suppression of lymphocytes function in Aspergillus sinusitis. Arch Otorhinolaryngol. 1989;246:321-3. [ Links ]
4. Khongkhunthian P, Reichart PA. Aspergillosis of the maxillary sinus as a complication of overfilling root canal material into the sinus: report of two cases. J Endod. 2001;27:476-8. [ Links ]
5. Giardino L, Pontieri F, Savoldi E, Tallarigo F. Aspergillus mycetoma of the maxillary sinus secondary to overfilling of a root canal. J Endod. 2006;32:692-4. [ Links ]
6. Legent F, Billet J, Beauvillain C, Bonnet J, Miegeville M. The role of dental canal fillings in the development of Aspergillus sinusitis. Arch Otorhinolaryngol. 1989;246:318-20. [ Links ]
7. De Foer C, Fossion E, Vaillant JM. Sinus aspergillosis. J Cranio-Maxillofac Surg. 1990;18:33-40. [ Links ]
8. Hauman CHJ, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002;35:127-41. [ Links ]
9. Yaltirik M, Koçak Berberoglu H, Koray M, Dulger O, Yildirim S, Aydil BA. Orbital pain and headache secondary to overfilling of a root canal. J Endod. 2003;29:771-2. [ Links ]
10. Dhong HJ, Ung JY, Park JH. Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol. 2000;14:227-31. [ Links ]
11. Fergunson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin N Am. 2000;33:389-98. [ Links ]
12. Shams MG, Motamedi MH. Aspergilloma of the maxillary sinus complicating an oralantral fistula. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2003;96:3-5. [ Links ]
13. Horré R, Schumacher G, Marklein G, Krömer B, Wardelmann E, Gilges S, De Hoog GS, Wahl G, Schaal KP. Case report: maxillary sinus infection due to Emericella nidulans. Mycoses. 2002;45:402-5. [ Links ]
14. Martins WD, Rosa EAR. Aspergillosis of the maxillary sinus: review and case report. Scand J Infect Dis. 2004;36:758-61. [ Links ]
15. Matjaz R, Jernej P, Mirela KR. Sinus maxillaris mycetoma of odontogenic origin: case report. Braz Dent J. 2004;15:248-50. [ Links ]
16. Yamaguchi K, Matsunaga T, Hayashi Y. Gross extrusion of endodontic obturation materials into the maxillary sinus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;104:131-4. [ Links ]
17. Burnham R, Bridle C. Aspergillosis of the maxillary sinus secondary to a foreign body (amalgam) in the maxillary antrum. J Oral Maxillofac Surg. 2009;47:313-5. [ Links ]
18. Costa F, Polini F, Zerman N, Robiony M, Toro C, Politi M. Surgical treatment of Aspergillus mycetomas of the maxillary sinus: review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;103:23-9. [ Links ]
19. Katzenstein A, Sale S, Greenberger P. Allergic aspergillosis sinusitis: a newly recognized form of sinusitis. J Allergy Clin Immunol. 1983;72:89-93. [ Links ]
20. Mensi M, Salgarello S, Pinsi G, Piccioni M. Mycetoma of the maxillary sinus: endodontic and microbiological correlations. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2004;98:119-23. [ Links ]
21. Ross IS. Some effects of heavy metals on fungal cells. Trans Br Mycol Soc. 1975;64:175. [ Links ]
22. Kopp W, Fotter R, Steiner H, Beaufort F, Stammberger H. Aspergillosis of the paranasal sinuses. Radiology. 1985;156:715-6. [ Links ]
23. Kilic C, Kamburoglu K, lcen Pehlivan Yuksel IP, Ozen T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 2010;4:462-7. [ Links ]
24. Fligny I, Lamas G, Rouhani F, Soudant J. Chronic maxillary sinusitis of dental origin and nasosinusal aspergillosis. How to manage intrasinusal foreign bodies? Ann Otolaryngol Chir Cervicofac. 1991;108:465-8. [ Links ]
25. Batur YB, Ersev H. Five-year follow-up of a root canal filling material in the maxillary sinus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2008;106:e54-6. [ Links ]
26. Bahadur S, Kacker K, D'Souza B, Chopra P. Paranasal sinus aspergillosis. J Laryngol Otol. 1983;97:863-7. [ Links ]
27. Stammberger H. Special problems. In: Stammberger H, ed. Functional endoscopic sinus surgery. Philadelphia: B.C. Decker; 1991. p. 400-24. [ Links ]
 Corresponding Author:
Corresponding Author:
Prof. Dr. Elismauro Francisco Mendonça
Department of Oral Sciences, Federal University of Goiás
Praça Universitária s/nº, Setor Universitário
CEP 74605-020, Goiânia, GO, Brazil
E-mail:elismaur@odonto.ufg.br













