Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.19 no.37 Canoas Jul./Dez. 2013
Gardner's syndrome suggested by radiographic findings
Síndrome de Gardner sugerida por achados radiográficos
Thiago Oliveira Gamba I; Matheus Lima Oliveira III; Isadora Luana Flores II; Solange Maria Almeida IV; Francisco Haiter-Neto IV; Romero Correia Bradley V; Jaqueline Oliveira Lopes Xavier V; Sérgio Lucio Pereira Castro Lopes VI
I DDS and MSc in Oral Radiology from the Department of Oral Diagnosis, Piracicaba Dental School, Universidade Estadual de Campinas (UNICAMP), Piracicaba, SP, Brazil
II DDS, MSc and PhD in Oral Pathology from the Department of Oral Diagnosis, Piracicaba Dental School, Universidade Estadual de Campinas (UNICAMP), Piracicaba, SP, Brazil
III DDS, MSc, and PhD in Oral Radiology from the Department of Oral Diagnosis and Surgery, Araraquara Dental School, Universidade Estadual Paulista (UNESP), Araraquara, SP, Brazil
IV DDS, MSc, and PhD in Oral Radiology from the Department of Oral Diagnosis, Piracicaba Dental School, UNICAMP, Piracicaba, SP, Brazil
V DDS and private practitioners, Vitória da Conquista, BA, Brazil
VI DDS, MSc, and PhD in Oral Radiology from the Department of Oral Diagnosis and Surgery, São José dos Campos Dental School, Universidade Estadual Paulista (UNESP), São José dos Campos, SP, Brazil
ABSTRACT
Gardner's syndrome (GS) is a hereditary disorder characterized by multiple osteomas, enostosis, epidermoid cysts, subcutaneous desmoid tumors and multiple gastrointestinal polyps. Given the variety of clinical manifestations, the triad of symptoms that better characterizes the GS is composed by polyps of the colon, multiple osteomas and tumors of soft tissue. The osteomas are most common in the frontal bone and mandible. A significant feature of GS is the progression to malignancy of the intestinal polyps in almost 100% of patients. Early detection of GS allows for an excellent prognosis and may be a lifesaving event. Thus, the aim of this case report was to describe the radiographic aspects of GS in the dentomaxillofacial region and to discuss with the current scientific literature.
Keywords: Diagnostic Imaging, Panoramic Radiography, Gardner Syndrome, Osteoma.
RESUMO
A síndrome de Gardner (SG) é uma desordem caracterizada por múltiplos osteomas, enostosis, cistos epidermoides, tumores desmoides subcutâneos e múltiplos pólipos gastrointestinais. Considerando a variedade de manifestações clínicas, a tríade dos sintomas que melhor caracterizam a SG é composta por pólipos do cólon, múltiplos osteomas e tumores de tecido mole. Os osteomas são mais comuns no osso frontal e mandíbula. Uma característica significativa da SG é a progressão maligna dos pólipos intestinais em aproximadamente 100% dos pacientes. A detecção precoce da SG favorece um excelente prognóstico e pode salvar vidas. Então, o objetivo deste relato de caso foi descrever os aspectos radiográficos da SG na região dento-maxilo-facial e discutir com a literatura científica atual.
Palavras-chave: Diagnóstico por Imagem, Radiografia Panorâmica, Síndrome de Gardner, Osteoma.
INTRODUCTION
Gardner's syndrome (GS), also known as familial colorectal polyposis, is an autosomal dominant disorder with equal sex distribution and a prevalence ranging from 1:8,300 to 1:16,000 births 1. Clinical manifestations include multiple osteomas, enostosis, epidermoid cysts, subcutaneous desmoid tumors, and intestinal polyps – mainly colon and rectum. Among other extracolonic manifestations, odontomas, pigmented lesions of the fundus, congenital hypertrophy of the retinal pigment epithelium and dental anomalies, such as supernumerary and impacted teeth, are present. Early detection of GS is very important because of the strong predilection of the intestinal polyps to undergo malignant conversion 2,3.
The variety of clinical manifestations limits the diagnosis of GS. Although some patients present all of the hallmarks of the syndrome, other patients may show 1 or 2 anomalies. Cristofaro et al. described a family in which GS was diagnosed in three generations and observed that clinical sequelae were manly facial eumorphy and occlusion problems of the temporomandibular joint, with no case of malignant transformation 1. Given this limitation in the diagnostic process, the triad of symptoms that better characterizes the GS is composed by polyps of the colon, multiple osteomas and tumors of soft tissue.
Osteomas may affect any part of the skeleton, but they are most commonly present in the jaws and paranasal sinuses4. Because such regions are directly related to the object of study of dental surgeons, it is important to better characterize radiographic findings that suggest the presence of this syndrome. Thus, the aim of this case report was to describe the radiographic aspects of GS in the dentomaxillofacial region, and to discuss with the current scientific literature.
CASE REPORT
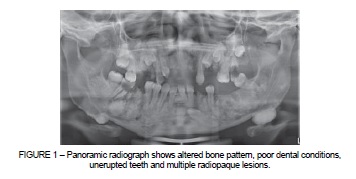
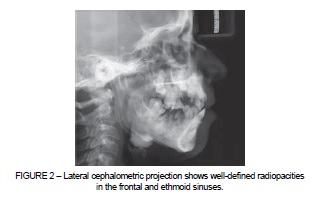
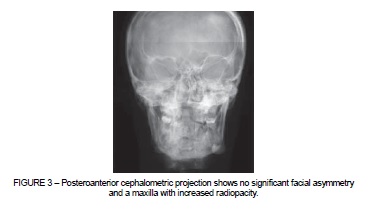
An asymptomatic 32-year-old white female patient was referred to the radiology clinic. Panoramic, lateral and posteroanterior (PA) cephalometric projections were obtained. Panoramic radiograph (Figure 1) revealed significant alteration of the bone pattern throughout both jaws and poor dental conditions. Teeth nos. 11, 12, 16, 21, 22, 36, 37 were missing. Teeth nos. 15, 18, 24, 25, 28, 33, 41 were unerupted. Three supernumerary microdonts were found in the anterior and right maxilla. Multiple small-sized, well-defined and rounded radiopacities were present in the anterior mandible around the lower right canine; the periphery was corticated with an adjacent radiolucent border, which is suggestive of odontoma. Well-defined, rounded, uniform radiopacities were present bilaterally on the inferior mandibular border below the molars, and on the left mandibular notch. Such characteristics are suggestive of periosteal osteomas. Dense bone islands were observed along the mandible and on the posterior maxilla with a defined periphery that, in some regions, blended with the trabeculae of the surrounding bone. The floor of the maxillary sinus was ill defined and apparently lifted. The right temporomandibular joint (TMJ) presented bone cortical thickening of the condyle, articular fossa and tubercle, and the left TMJ was within the normal limits. Lateral projection (Figure 2) showed osteoma-like radiopacities in the frontal and ethmoid sinuses, and normal development of the jaws. PA projection (Figure 3) revealed no significant facial asymmetry and an increased radiopacity of the maxilla. All of these manifestations are highly suggestive of GS. Thus, the patient was referred to the gastroenterologist for further investigation of the presence of intestinal polyps.
DISCUSSION
GS was first described in the early 1950s as having an autosomal dominant pattern of inheritance. It is caused by a mutation in the band q21 on chromosome 5 (5q21) of the adenomatous polyposis coli (APC) gene. The site of mutation of the APC gene determines the manifestations of GS and specific codon mutations are related to specific extracolonic manifestations. Molecular genetic testing of APC is available and is often used in the early diagnosis of at-risk family members. Reported prevalence of all the APC-associated polyposis conditions is 2.29 to 3.2 per 100,000 1,2,4,5.
The majority of the patients with GS do not present all of the expected clinical features for this disease. Skeletal anomalies are observed in about 90% of the cases, and osteoma is the most frequent of them. Osteoma is a benign tumor composed of mature cortical or cancellous bone and the mandible is the most common location 4. Other regions, such as the maxilla, mandibular condyle and frontal, temporal and zygomatic bones have been reported6. A solitary osteoma of the jaw is a common incidental finding on panoramic radiography, however, patients with multiple osteomas must be carefully assessed to exclude the presence of GS. This case presents three suggestive images of periosteal osteomas located on the inferior border of the mandible and mandibular notch. Herford et al. 4 reported two patients who were under treatment of an osteoma and stated that it is preferable to remove the osteomas before they achieve a large size and limit the extent of future surgical procedures. Computed tomography may be employed to better characterize the size, dimensions and relationship with adjacent structures of the osteomas. It is believed that the scientific literature does not provide reliable information about the frequency of osteomas, since they are asymptomatic lesions.
Aletaha and Fateh-Moghadam 7 presented a case of a patient whose first sign of GS was the detection of a palpable mass in the deep superonasal quadrant of the left orbit. Osteomas were detected in the orbital region adjacent to the optic canal, within the ethmoidal air cells, and mandibular angle. The temporomandibular joint was not significantly affected in the present case, but the literature has shown some cases of involvement of the condylar head 1,4,5,8. Additionally, this patient was asymptomatic and the radiographic characteristics of GS were only detected after a routine dental examination.
Several studies have reported unerupted and impacted teeth associated with GS 5,6,8,9, which is in agreement with the present case. Some teeth were clearly misplaced, tilted toward another hard structure while some teeth could just not reach the occlusal plane. Boffano et al. 6 reported a 21-year-old patient with multiple round radiopaque lesions and impacted teeth in the maxilla and mandible detected on a panoramic radiograph. The radiopaque lesions had an osteoma-like appearance, which is strongly indicative of GS.
Polyps of the colon can also be observed on patients affected by GS. A polyp is an abnormal growth of tissue projecting from a mucous membrane, and is not commonly associated with symptoms. The potential for benign colon polyps transforming into malignant colon polyps is cause for concern. Malignant evolution can be avoided by preventive colectomy. Fecal occult blood, sigmoidoscopy/colonoscopy, and upper gastrointestinal endoscopy are required at least every 1-2 years until the patient is 50 years old 2,4,10. Extracolonic manifestations of GS often precede the discovery of colonic polyps, and may facilitate early identification. However, Cankaya et al. 5 reported a rare case of a patient with oral and maxillofacial features of GS and absence of intestinal polyps.
Several manifestations occur in the oral and maxillofacial region and may be discovered during regular dental examination. Developmental dental abnormalities, and odontomas are often discovered on routine radiographs. The patient described in this report showed supernumerary, absent and unerupted teeth, in addition to numerous osteomas, which is highly indicative of GS. Dental panoramic radiography has shown to be a very effective imaging modality to detect multiple osteomas in the jaws. Importantly, although the dental surgeon may be the first healthcare professional to suspect the diagnosis, it would be inappropriate to take panoramic radiographs of all new patients. This should be considered due to possible hazards involved with the use of x rays. Thus, the need of panoramic radiography when screening patients for GS is determined by findings from dental history and clinical examination. Clinical differential diagnosis of GS should include multiple buccal exostoses, idiopathic osteosclerosis, florid osseous dysplasia, multiple odontomas and osteomas 10.
FINAL CONSIDERATIONS
GS presents several oral and maxillofacial manifestations. Osteomas, unerupted teeth and odontomas are frequently observed. Dental surgeons play an important role in the early detection of such disease.













