Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.19 no.37 Canoas Jul./Dez. 2013
Combined orthognathic surgery and prosthetic treatment for class III skeletal malocclusion
Combinação de cirurgia ortognática e tratamento protético para má oclusão esquelética classe III de Angle
Luka Dias Wellar I; Leandro Reinhardt II; Marcos Antonio Torriani II; Tatiana Pereira-Cenci III; Noéli Boscato III
I Dental student at Universidade Federal de Pelotas (UFPel), Pelotas, RS, Brazil
II Professor at the Department of Oral and Maxillofacial Surgery, School of Dentistry, UFPel, Pelotas, RS, Brazil
III Professor at the Graduate Program in Dentistry, School of Dentistry, UFPel, Pelotas, RS, Brazil
ABSTRACT
This clinical report discusses the case of a partially edentulous patient with class III skeletal malocclusion, suffering from poor masticatory function and esthetic appearance caused by severe anteroposterior discrepancy between the dental arches and loss of occlusal vertical dimension. The functional and esthetic rehabilitation was performed with orthognathic surgery followed by prosthetic treatment using an overlay removable partial denture. At the end of the treatment, the patient was successfully rehabilitated, both functionally and esthetically, through reestablishment of the occlusal vertical dimension and correction of the anteroposterior discrepancy between the dental arches. The overlay removable partial denture is a simple and time-efficient alternative in the treatment of partially edentulous patients with class III skeletal malocclusions and small anteroposterior discrepancies between dental arches. Additionally, an esthetic smile and functional rehabilitation of the stomatognathic system was satisfactorily obtained with orthognathic surgery followed by prosthetic treatment.
Keywords: Overlay Removable Partial Denture, Dental Occlusion, Orthognathic Surgery.
RESUMO
Este caso clínico descreve a situação de uma paciente parcialmente desdentada com má oclusão esquelética classe III de Angle que apresentava pobre função mastigatória e desagradável aparência estética, originada pela grave discrepância anteroposterior entre as arcadas dentárias e pela perda de dimensão vertical de oclusão. Sua reabilitação funcional e estética foi realizada através de cirurgia ortognática e tratamento protético mediante a instalação de uma prótese parcial removível tipo overlay. Ao final do tratamento, a paciente foi reabilitada funcionalmente e esteticamente com sucesso através do restabelecimento da dimensão vertical de oclusão e correção da discrepância anteroposterior entre os arcos dentários. A prótese parcial removível tipo overlay é uma alternativa simples e rápida para o tratamento de pacientes parcialmente desdentados com má oclusão esquelética classe III e pequena discrepância anteroposterior entre os arcos dentários. Neste caso clínico, foi obtido de forma satisfatória o restabelecimento estético e funcional do sistema estomatognático através da combinação de cirurgia ortognática e tratamento protético.
Palavras-chave: Prótese Parcial Removível, Oclusão Dentária, Cirurgia Ortognática.
INTRODUCTION
Class III malocclusion is primarily a skeletal condition characterized by the protrusion of the mandible, or the retrusion of the maxilla, or both 1. In patients with class III malocclusion, the mesiobuccal cusps of the maxillary first molars are placed not in the mesiobuccal groove (ideal position of the opposing mandibular first molars), but distal to it 1-3. Ideally, diagnosis of this discrepancy should be made early, during the primary dentition, if possible, in order to increase the possibilities of treatment with good prognosis 4. Late diagnosis of this bone disharmony makes treatment more complex and expensive 5.
In this context, orthodontic treatment alone, or in combination with orthognathic surgery, usually resolves most cases of class III malocclusion. Conversely, oral rehabilitation of totally or partially edentulous patients is challenging and sometimes requires surgical, orthodontic and prosthetic treatments combined 6. The main goals of this multidisciplinary approach are reestablishment of facial and dental harmony, functional occlusion, as well as health and stability of the orofacial structures 7.
The overlay removable partial denture (ORPD) is a therapeutic modality that covers the occlusal surface of one or more abutment teeth, and has shown satisfactory esthetic and functional treatment outcomes. It is primarily indicated in the rehabilitation of patients with reduced occlusal vertical dimension (OVD) or with slight alteration in the anteroposterior occlusal plane 8,9. The aim of this case report is to describe the treatment of a partially edentulous patient with class III skeletal malocclusion through a multidisciplinary approach, including orthognathic surgery and prosthetic treatment with an ORPD.
CASE REPORT
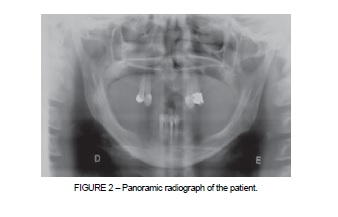
A 50-year-old woman was referred to the Oral and Maxillofacial Surgery Clinic of Universidade Federal de Pelotas (UFPel), southern Brazil. She reported that she was unhappy with her masticatory function and with the esthetic appearance of her smile. Medical evaluation revealed that the patient presented satisfactory general health; upon intraoral examination, very few remaining teeth and severe anteroposterior discrepancy between the dental arches were observed. The maxillary and mandibular arches were classified as Kennedy class I removable partial denture, and the maxillary arch as Kennedy class IV removable partial denture (Figure 1), according to the Kennedy classification; appropriate modifications were applied, according to Applegate's modifications. Clinical and radiographic examination revealed that the periodontal condition of maxillary teeth no. 13, 14, 23 and 24, and mandibular teeth no. 31, 32, 41 and 42, was satisfactory (Figure 2). Intraoral examination also revealed that the right and left maxillary first premolars, no. 14 and 24, respectively, presented with clinically acceptable class II amalgam restorations. On clinical and radiographic examination, loss of OVD was detected (Figure 3).
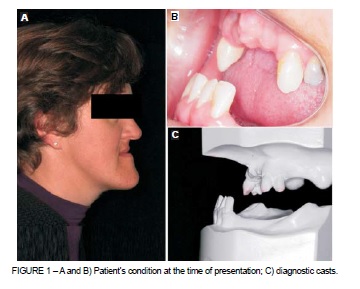
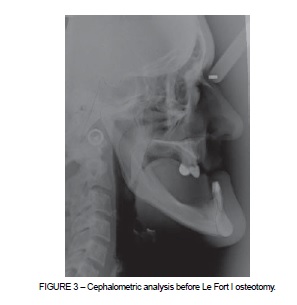
A cephalometric analysis (Figure 3) was performed and diagnostic casts of both arches were obtained (Figure 1C). Occlusion was again analyzed, together with the diagnostic casts mounted on a semi-adjustable articulator. This evaluation confirmed the notable discrepancy between the dental arches.
The ideal treatment objectives, in this case, were to correct the skeletal discrepancies between the maxilla and the mandible, and to establish a satisfactory esthetic appearance by correcting this anteroposterior discrepancy. Other essential objectives included the replacement of missing teeth in both arches, establishment of a stable occlusal relation, and improvement of the patient's facial and dental esthetics.
Considering clinical and radiographic findings, the various treatment options available were discussed with the patient, such as dental implants, fixed partial dentures, conventional removable partial dentures, ORPDs, and orthognathic surgery. Taking into consideration the patient's general health status, the cost and time required for treatment, local risk factors (status of the remaining teeth, as well as their periodontal support) and the anteroposterior discrepancy between the dental arches, the best possible treatment alternative for the patient was chosen. The treatment plan included orthognathic surgery followed by prosthetic rehabilitation. Adequate esthetics, stable occlusion and skeletal discrepancy correction would be possible with this approach. The patient then received detailed information regarding the treatment that was chosen, and signed the informed consent.
Following, the surgical stage was planned with the aid of radiographs and with diagnostic casts mounted on a semi-adjustable articulator. A Le Fort I osteotomy was performed under general anesthesia, in the hospital's operating room. The maxillary alveolar process was completely mobilized and was advanced by 7 mm, as planned by cephalometric analysis. The extent of advancement was confirmed by maxillomandibular fixation, which was carried out using an intermediate acrylic splint. The maxilla was stabilized in the desired position using L-shaped titanium miniplates, with the aid of screws placed bilaterally in the nasomaxillary buttress region. Due to the anatomical limitations, it was not possible to fully correct the severe anteroposterior discrepancy between the dental arches.
Nine months after the orthognathic surgery, a clinical examination again was performed; new diagnostic casts were obtained and mounted on a semi-adjustable articulator. Analysis of the anteroposterior relation between the dental arches and the OVD of occlusion confirmed that the residual discrepancy could be compensated by prosthetic rehabilitation. Due to the socioeconomic status of the patient and the anatomical limitations of the dental arches, maxillary and mandibular removable partial dentures, which represent low-cost alternatives, were chosen for treatment. Thus, the treatment modality selected involved manufacturing a maxillary ORPD covering the remaining teeth and correcting the vertical discrepancy, and manufacturing a conventional mandibular removable partial denture (RPD).
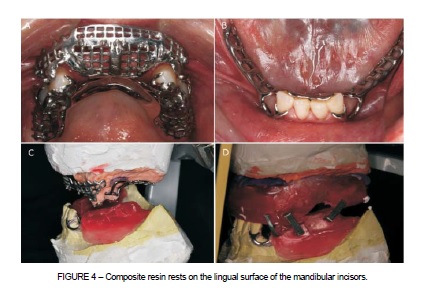
The maxillary canines and first premolars (13, 14, 23 and 24) and the mandibular incisors (31, 32, 41 and 42) were selected to serve as abutment teeth for the maxillary ORPD and the mandibular RPD, respectively. Occlusal rests on all the abutment teeth and rests built in composite resin on the lingual surface of the mandibular incisors were prepared (Figure 4). Next, impressions of both arches were made with irreversible hydrocolloid (Hidrogum, Zhermack, Leicester, UK), and the casts thus obtained were mounted on a semi-adjustable articulator. The casts, along with the designs of the dental prostheses, were sent to the prosthetic laboratory for the fabrication of the metal frameworks for the maxillary ORPD and the mandibular RPD.
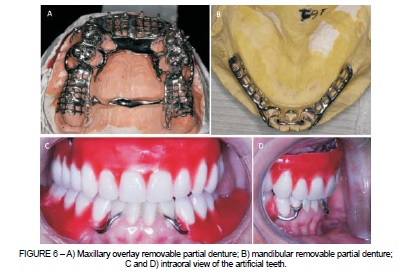
The design of the maxillary ORPD included occlusal support on maxillary canines and premolars, and a double palatal bar (Figures 5A and 6A). The rests of the ORPD were extended in the frontal part of the palatal bar in order to restore the patient's upper lip support, with the addition of acrylic resin. The dental clasps for the mandibular RPD were selected after the analysis of the diagnostic casts. A Roach clasp (Figures 5B and 6B) along with a lingual indirect retainer, supported by rests built in composite resin on the lingual surface of the mandibular incisors, was planned.
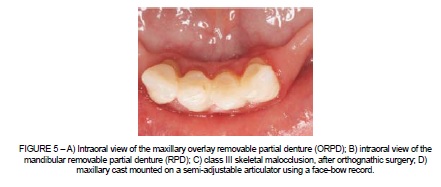
Within fifteen days, the metal frameworks were fabricated using Cobalt-Chromium alloy (Remanium GM 380; Dentaurum, Pforzhein, Germany). Next, try-in of the metallic frameworks was done; they were checked for support, retention and stability. The maxillary and mandibular casts, along with the metal frameworks, were then mounted on a semi-adjustable articulator, using a facebow record (Figures 5C and 5D). The mandibular cast was mounted in centric relation and a clinical determination of the OVD was performed. Esthetic and phonetic methods were used to determine the maxillomandibular relation. The interocclusal space required for reestablishment of the appropriate OVD was recorded as 6 mm. Next, the maxillary and mandibular casts, mounted on the semiadjustable articulator, along with the metal frameworks and the facebow record, were sent to the prosthetic laboratory for assembly of the artificial teeth. Thereafter, the artificial teeth were tried-in, to verify the maxillomandibular relation and to obtain the patient's approval before final processing (Figures 6C and D) using heat-polymerizing acrylic resin (Clássico Artigos Odontológicos, São Paulo, SP, Brazil). The prostheses were then tried-in, and occlusal adjustments were performed. Finally, the prostheses were polished and subsequently inserted into the oral cavity. The prosthetic rehabilitation completed the orthognathic surgery treatments. The intraoral view of the patient before and after treatment (Figures 7A and 4B), shows adequate functional and esthetic relation. Occlusal adjustments were performed at intervals of twenty-four hours, three days, and one week following insertion of the prostheses.
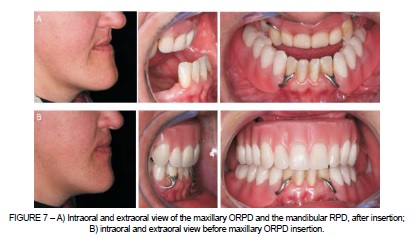
At the end of orthognathic surgery and prosthetic treatment, the patient's facial and dental aspects were improved. The patient had been successfully rehabilitated, both functionally and esthetically, through OVD reestablishment and correction of anteroposterior discrepancy between the dental arches.
DISCUSSION
In this case report, the treatment plan was satisfactory and the treatment objectives were achieved, because a functional and esthetic occlusion was obtained. Functional and esthetic parameters should be the main factors considered by professionals during rehabilitation of a patient with class III skeletal malocclusion 1,10-13. In this case, prosthetic treatment with removable partial dentures was provided for a class III skeletal malocclusion patient, where due to anatomical limitations, previous orthognathic surgery was not sufficient to correct anteroposterior discrepancy between the dental arches. After surgery, the patient still reported dissatisfaction with the esthetic results. In this case, the ORPD could successfully improve the treatment outcomes 7, because it is an effective treatment for providing satisfactory esthetics and function to patients that present unacceptable overjet and overbite and few remaining teeth 5,9,14.
In this context, an important feature of ORPD is the use of remaining teeth as retainers, without causing any dental wear. These teeth, used as retainers, can improve both retention and stability, while simultaneously reducing alveolar bone resorption and maintaining dental proprioception 15. This also allows future restorative treatment to be carried out, such as rehabilitation with implant-supported prostheses. Another advantage of this option of treatment is the lower cost and shorter time span for fabrication of prosthesis, because it does not require additional dental preparation, such as endodontic treatment 6. These factors make the ORPD treatment modality widely popular as an alternative to fixed or implant-supported prostheses, which normally involve higher costs and greater time span for fabrication 7,16.
However, ORPD treatment necessitates observance of an excellent oral care regimen at home, with professional assistance, to prevent failures. Failure to maintain good oral health could lead to failure of the prosthetic rehabilitation once the abutment teeth become susceptible to dental caries. Thus, the patient was instructed to comply with an oral self-care program that included the use of fluoridated toothpaste and a 6-month recall schedule.
Other disadvantages associated with this type of prosthesis are fracture and color instability of the acrylic base resin 13,15, and wear of the artificial teeth 5 Additionally, the lack of planning in the execution of the rehabilitation could lead to serious biomechanical problems, rendering the prosthesis non-functional, and causing biological trauma to the remaining teeth and periodontal tissues, as well as psychological trauma to the patient 7.
Orthodontic treatment was an infeasible alternative in this particular case due to the severe skeletal discrepancies between the maxilla and the mandible. Moreover, orthognathic surgery offered limited outcomes, as predicted during the process of treatment planning, due to the anatomical limitations. Thus, the use of an ORPD following orthognathic surgery was an excellent alternative with satisfactory esthetic and functional results.
In this case, the ORPD compensated for the small anteroposterior bone disharmony satisfactorily, and reestablished function and esthetics. Nevertheless, it is important to emphasize that the favorable results of the presented case should also be attributed to the multidisciplinary approach adopted, including surgical and prosthetic treatment. At follow-up, a clinical evaluation was performed, and the patient's satisfaction was assessed. We were therefore able to verify that the ORDP provides a stable, comfortable and functional solution.
FINAL CONSIDERATION
The ORPD is a simple and time-efficient alternative in the treatment of partially edentulous patients with class III skeletal malocclusions and small anteroposterior discrepancies between dental arches. Additionally, an esthetic smile and functional rehabilitation of the stomatognathic system were satisfactorily obtained with orthognathic surgery followed by prosthetic treatment.
REFERENCES
1. Bataglion C, Hotta TH, Matsumoto W, Ruellas CV. Reestablishment of occlusion through overlay removable partial dentures: a case report. Braz Dent J. 2012;23(2):172-4. [ Links ]
2. Ellis E, Macnamara JA. Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984;42(5):295-305.
3. Rotas N, Sykes JM. Esthetic orthognathic surgery. Facial Plast Surg Clin North Am. 2002;10(3):233-48.
4. Kapust AJ, Sinclair PM, Turley PK. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113(2):204-12.
5. Del Castillo R, Lamar F, Ercoli C. Maxillary and mandibular overlay removable partial dentures for the treatment of posterior open-occlusal relationship: a clinical report. J Prosthet Dent. 2002;87(6):587-92.
6. Pattanaik SB, Wadkar AP. Prosthetic rehabilitation of a patient with congenital oro-nasal defect with an interim prosthesis: a case report. J Indian Prosthodont Soc. 2001;11(2):113-6.
7. Fonseca J, Nicolau P, Daher T. Maxillary overlay removable partial dentures for the restoration of worn teeth. Compend Contin Educ Dent. 2011;32(3):14-20.
8. Hickey AJ, Vergo TJ. Prosthetic treatments for patients with ectodermal dysplasia. J Prosthet Dent. 2001;86(4):364-8.
9. Sakar O, Beyli M, Marsan G. Combined prosthodontic and orthodontic treatment of a patient with a Class III skeletal malocclusion: a clinical report. J Prosthet Dent. 2004;92(3):224-8.
10. Rabie AB, Gu Y. Diagnostic criteria for pseudo-Class III malocclusion. Am J Orthod Dentofacial. 2000;117(1):1-9.
11. Bell R, Kiyak HA, Joondeph DR, Mc Neill RW, Wallen TR. Perceptions of facial profile and their influence on the decision to undergo orthognathic surgery. Am J Orthod. 1985; 88(4):323-32.
12. Berkey DB, Berg RG, Ettinger RL, Mersel A, Mann J. The old-old dental patient: the challenge of clinical decision-making. J Am Dent Assoc. 1996;127(3):321-2.
13. Windchy AM, Morris JC. An alternative treatment with the overlay removable partial denture: a clinical report. J Prosthet Dent. 1998;79(3):249-53.
14. Jayasree K, Bharathi M, Dileep VN, Vinod B. Precision attachment: retained overdenture. J Indian Prosthodont Soc. 2012;12(1):59-62.
15. Schuch C, de Moraes AP, Sarkis-Onofre R, Pereira-Cenci T, Boscato N. An alternative method for the fabrication of a root-supported overdenture: a clinical report. J Prosthet Dent. 2013;109(1):1-4.
16. Nunes DB, da Silva P, Pereira-Cenci T, Garbin CA, Schuh C, Boscato N. Correction of nonparallel implants for an implant-retained overdenture. Gen Dent. 2010;58(4):168-71.
 Correspondence:
Correspondence:
Noéli Boscato
Federal University of Pelotas
Graduate Program in Dentistry
Gonçalves Chaves Street, 457, 2nd floor, Downtown
CEP 96015-560, Pelotas, RS, Brazil
E-mail: noeliboscato@gmail.com













