Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.20 no.38 Canoas Jan./Jun. 2014
Sealing of root perforation with glass ionomer cement: a case report
Selamento de perfuração radicular com cimento de ionômero de vidro: caso clínico
Ronise Ferreira Dotto I; Alcebiades Nunes Barbosa I; Sidney Ricardo Dotto II; Chirley Roberta Hermes III
I PhDs and adjunct professors at the Department of Nursing and Dentistry, School of Dentistry, Universidade de Santa Cruz do Sul (UNISC), Santa Cruz do Sul, RS, Brazil
II PhD and ajunct professor at the School of Dentistry of Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil
III Dental student and Probex scholarship holder at the School of Dentistry, UNISC, Santa Cruz do Sul, RS, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
Despite the development of endodontic therapy, adverse complications can arise during treatment, resulting in a questionable prognosis; root perforation is one such complication. Root perforations located along different thirds of the root canal are associated with practitioner error during the operative stages of endodontic treatment, particularly with failure to observe the anatomic singularities of different tooth types. Various materials have been suggested and used to repair root canal perforations, including calcium hydroxide, silver amalgam, mineral trioxide aggregate (MTA), hydroxyapatite, and glass ionomer cement. This report describes the clinical management of a maxillary second premolar in which periapical radiography showed satisfactory canal obturation, but with a lateral root perforation present at the cervical level. Initial treatment involved curettage and sealing of the perforated area with resin-modified glass ionomer cement, followed by composite-resin reconstruction of the crown. There was favorable clinical and radiographic progression at 1- and 2-year follow-up. We thus conclude that tooth longevity can be prolonged even in the presence of a root perforation.
Keywords: Endodontics, Root Canal, Dental Materials.
RESUMO
Apesar do desenvolvimento da terapia endodôntica, complicações adversas podem surgir durante o tratamento, resultando em prognóstico duvidoso; a perfuração radicular situa-se entre essas complicações. As perfurações radiculares localizadas nos diferentes terços do canal radicular estão relacionadas às negligências nas etapas operatórias do tratamento endodôntico, principalmente a não observância das particularidades anatômicas dos diferentes grupos dentais. Diversos materiais têm sido indicados e utilizados para selar as perfurações endodônticas, entre eles o hidróxido de dentináricálcio, o amálgama de prata, o agregado trióxido mineral (MTA), a hidroxiapatita e o cimento de ionômero de vidro. Este trabalho tem por objetivo descrever a situação clínica de um 2º pré-molar superior no qual se constatou por meio da radiografia periapical que o mesmo possuía obturação de canal satisfatória, porém com a presença de uma perfuração lateral a nível cervical da raiz. Inicialmente o tratamento envolveu a curetagem e selamento da área perfurada com cimento de ionômero de vidro modificado por resina seguido da reconstrução coronal com resina composta. Após avaliações de 1 e 2 anos, observou-se uma evolução clínica e radiográfica favorável, o que permite concluir que é possível aumentar a longevidade do elemento dental em boca não obstante a presença de uma perfuração radicular.
Palavras-chave: Endodontia, Canal Radicular, Materiais Dentários.
INTRODUCTION
Recent developments in endodontic therapy and adhesive restoration techniques have substantially increased the rate of conservation of teeth with endodontic involvement and significant coronal damage.
In some clinical settings, however, complications can hinder treatment and lead to a questionable prognosis. One such complication is root perforation, which is defined as an artificial passage created within a tooth or its root, whether iatrogenic or due to pathological resorption, which produces a communication between the pulp cavity and the periodontal tissues. The most severe complication of root perforation is the potential for secondary periodontal inflammation and loss of bone attachment, ultimately leading to tooth loss 1.
Several procedures performed during endodontic treatment may lead to perforation. The prognosis depends on the extent and location of the perforation, as well as on the time elapsed between perforation and repair 2.
Perforation, whether due to carious decay, iatrogenesis, or degenerative processes (such as internal and external resorption), may occur in the cervical, middle, or apical thirds of the root, as well as in the furcation; it constitutes a clinical challenge in conventional endodontic practice 3. Depending on the location, different treatment techniques are available to address this event 4.
Iatrogenic perforations may be caused by several reasons, including aberrant canal morphology, practitioner error while gaining access to the pulp chamber, failure during chemical and mechanical preparation due to inadequate canal wall wear, calcifications, or preparation for intracanal post placement, and may be driven by practitioner negligence, recklessness, or inexperience. Therefore, several authors have sought to study alternatives that increase the safety of instrumentation so as to minimize rates of iatrogenic perforation 1.
When located in the furcation or cervical third of the root, perforations have a negative impact on the prognosis of endodontic treatment, as they trigger an inflammatory reaction in the periodontal region that may lead to attachment loss and, occasionally, tooth loss as well. Depending on the crestal bone level and the degree of its destruction in the region of the perforation, a periodontal pocket may form. Once the alveolar bone is destroyed, granulation tissue is likely to form and may invaginate into the tooth through the perforation tract 5.
Adequate repair of a perforation requires sealing of the tract. The material used for this purpose will be effective if it provides excellent sealing, is biocompatible and easy to compound, and is able to promote osteogenesis and cementogenesis 4-7.
A wide range of materials has been used to seal endodontic perforations. Differences in outcome show that no optimal material is available; rather, there is a broad selection to choose from depending on the factors involved in each case (size, location, contamination, time elapsed between perforation and repair) and, of course, on which material is available at the time the perforation is detected 4,8.
Materials employed for the treatment of root perforations and reported in the literature include calcium hydroxide 9, silver amalgam 5, mineral trioxide aggregate (MTA) 7,10,11, hydroxyapatite 10, and glass ionomer cement 12,13. Silver amalgam is not advised for this purpose, due to its poor retention and high marginal leakage rate.
Glass ionomer cement, which is commonly used for retrograde obturation, is also an alternative for sealing of perforations, especially those located in the cervical third, where use of adhesive restorative materials has been recommended. Glass ionomer cement is classified as such, and has been used to treat resorption defects and iatrogenic perforations 14.
The properties of glass ionomer cement are adequate for repair of subgingival lesions: it is biocompatible, bonds to dentin and to cementum, releases fluoride, and has a low thermal expansion coefficient 15.
Gomes et al. 16 studied the periodontal response to resin-modified glass ionomer cement (RMGIC) and amalgam placed in surgical windows and left for 124 days in the dog, and found a less pronounced inflammatory response to RMGIC than to amalgam. In some sites restored with RMGIC, the authors found evidence of bone repair and a connective tissue lining.
Developed at Loma Linda University in Loma Linda, California, MTA is a composite material containing tricalcium silicate, tricalcium aluminate, and other mineral oxides that sets into a hard mass within 4 hours of contact with water and has proven sealing ability for retrograde obturation 12.
MTA has been the first-line material of choice for perforation repair due to its compatibility with periapical tissues, its sealing ability, its behavior in the presence of moisture, and its ability to induce cementogenesis 2. Furthermore, it does not affect the healing process 2,17. Studies have shown a favorable tissue response in MTA-treated perforations, providing further evidence of the biological properties of this material 17. MTA is reportedly able to stimulate mineral deposition at the material-dentin interface and within the dentinal tubules 5.
This report describes a clinical case in which a lateral root perforation in the distocervical region of a maxillary premolar was detected at the time of coronal restoration after endodontic treatment. The decision was made to seal the perforation with light-cured glass ionomer cement.
CASE REPORT
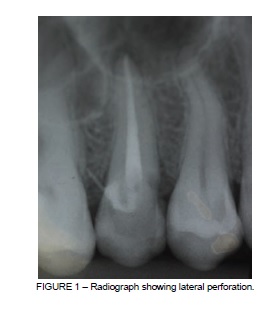
A 21-year-old woman presented for restoration of a right maxillary second premolar after endodontic treatment. Radiographic examination showed satisfactory obturation of the root canal system, but also revealed a root perforation in the distocervical region (Figure 1).
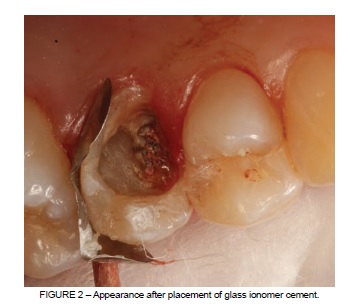
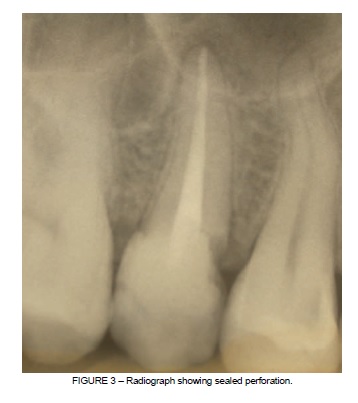
First, the temporary filling material was removed from the occlusal cavity and pulp chamber, which revealed a passage between the distocervical region of the root and the periodontium, approximately 2-3 mm in diameter, as well as granulation tissue invaginating into the pulp chamber with copious bleeding. Under infiltration anesthesia, the granulation tissue was removed with periodontal curettes. A sectional matrix (Unimatrix, TDV) was then placed into the interproximal space between the affected tooth and the adjacent first molar to provide external sealing in the area of the perforation. A wooden wedge was introduced tightly to stabilize the matrix in place and minimize the presence of moisture in the area. With a Centrix syringe (DFL) and using the matrix for isolation, RMGIC (Vitro Fil LC, DFL) was injected into the perforation and into the deepest region of the pulp chamber to seal the perforated area (Figure 2). Radiographic examination showed adequate sealing (Figure 3).



One week later, the patient returned for further restoration. First, a circumferential retainerless matrix device (AutoMatrix, TDV) was placed and the mesial wall of the tooth reconstructed with composite resin to facilitate rubber dam placement and improve the effectiveness of isolation for later stages of the restoration process (Figure 4). A temporary filling was placed (Coltosol, Vigodent S/A Ind. e Com., Bonsucesso, RJ, Brazil) and the patient sent home.
At the next appointment, rubber dam isolation was performed, the temporary filling was taken out, and the obturation material was partially removed with a slightly heated condenser. Using a #3 Largo reamer (Wilcos do Brasil Indústria e Comércio Ltda, Petrópolis, RJ, Brazil), the canal was widened down to approximately half of the root length. A fiberglass intracanal post (Whitepost, FGM) was then placed to reinforce the tooth/restoration complex. The post was test-fitted, cut to size, and cemented into the canal with Rely X ARC resin cement (3M ESPE) and Scotchbond Multi-Purpose dental adhesive (3M ESPE), in accordance with manufacturer instructions (Figure 5).
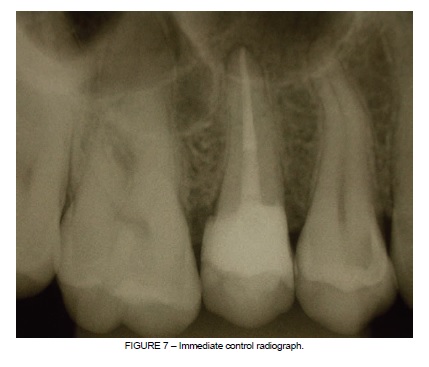
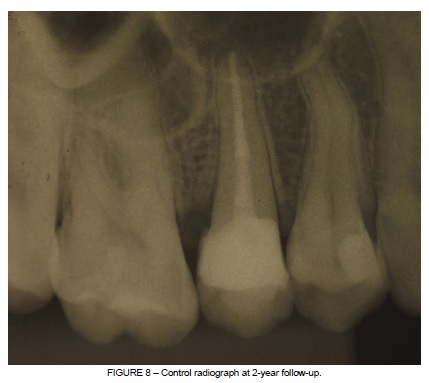
The crown was then restored with composite resin (Charisma, Heraeus Kulzer) and a conventional two-step adhesive system (Single Bond 2, 3M ESPE). Any flash was removed, the occlusion was adjusted, and the patient discharged. One week later, the surface of the restoration was shaped and polished to its final configuration, thus concluding the reconstruction portion of treatment (Figure 6), and a control periapical radiograph was obtained (Figure 7). At 2-year follow-up, the clinical and radiographic outcome was satisfactory (Figure 8).
DISCUSSION
Perforations located in the furcation region or cervical third of the root have a negative impact on the prognosis of endodontic treatment, as they trigger an inflammatory reaction in the periodontal region that may lead to loss of attachment and, occasionally, of the affected tooth. Depending on the crestal bone level and the degree of its destruction in the region of the perforation, a periodontal pocket may form. Once the alveolar bone is destroyed, granulation tissue is likely to form and may invaginate into the tooth through the perforation tract 5.
No single optimal method for perforation repair exists. A wide range of materials and treatment strategies is available to conserve the affected tooth and return it to normal function.
Bernardes et al. 3 suggests that measures be taken to improve the outcomes of perforation repair, such as recognition, correction, assessment of results, and avoidance of file contact with bone and surrounding tissues during instrumentation. A small perforation will cause minor bleeding, while an extensive perforation will cause much heavier bleeding, which can prevent treatment from continuing.
In the present case, periapical radiographs revealed a lateral perforation in the distocervical region of the right maxillary second premolar; the prognosis was deemed favorable in view of the short time since perforation (less than 1 month between the end of endodontic treatment and presenting to our service). The prognosis of a perforation is highly dependent on the sealing ability of the chosen repair material and is related to the size and site of the perforation, the time since perforation, and the presence of microbial agents, as well as on the feasibility of sealing and the accessibility of the main canal 13,18.
Proper sealing of the perforated region is essential, as it prevents contamination and restores the physiological condition of the tooth and its surrounding tissues. Several materials have been used to seal root perforations, including amalgam, gutta-percha, zinc oxide and glass ionomer cements, MTA, resins, and calcium hydroxide 9.
Good success rates can be obtained with MTA for treatment of root perforations, making it the material of choice for such repairs due to its sealing ability and biocompatibility; it is well-tolerated by periapical tissues and does not interfere with the healing process 17,19,20. The biological properties of MTA have also been shown to induce a favorable response from periodontal tissues 17. MTA is known to stimulate mineral deposition at the material-dentin interface and within the dentinal tubules 21. In view of these stimulating properties, its use is justified in intraosseous root perforations.
However, in supraosseous and subgingival perforations, like that described in this report, sealants such as glass ionomer, compomers, and resins are the materials of choice, because they are not susceptible to dissolution and pose no risk of decontamination, unlike MTA. It is important to note that repair of subgingival perforations sometimes requires orthodontic extrusion and periodontal tissue remodeling in addition to restorative procedures 18.
Glass ionomer cement bonds well to dentin, which may be explained by the formation of chemical bonds between the glass ionomer and the calcium ions of dentin. On the other hand, the high fluidity of light-cured glass ionomer cement promotes better flow and, consequently, better filling of the perforation cavity, thus providing improved sealing 16. It is thus a good material for repair of perforations, especially those located in the cervical region, where use of restorative materials is indicated 12.
In the present clinical case, glass ionomer cement was also chosen because it has been widely employed for its physical properties and fluoride release and because it is light-cured, which greatly facilitates its use 3,13. In an in vitro study, Shimabuko 22 found less leakage in furcation perforations repaired with light-cured glass ionomer than in those repaired with amalgam, and placement of a calcium hydroxide barrier further improved the sealing ability of the cement.
Gomes et al. 16 found a reduced periodontal inflammatory response with RMGIC as compared with amalgam; some sites restored with the former even showed evidence of bone repair and connective tissue coating.
It is essential that practitioners adopt preventive management strategies to avoid iatrogenic perforations. Therefore, a thorough analysis of radiographs should always be performed to assess root and pulp chamber volume, root direction and curvature in relation to adjacent teeth, the longitudinal axis of the tooth, etc. On the other hand, knowledge of dental morphology, including both external (surface) and internal anatomy and their relations, can provide important guidance while gaining endodontic access 18. By taking this guidance into account, practitioners can substantially reduce the need for future interventions that might lead to a questionable prognosis.
FINAL CONSIDERATIONS
With good diagnosis, thorough treatment planning, and selection of appropriate procedures and restorative materials, good clinical outcomes can be obtained even in endodontically treated teeth with root perforations and major coronal damage.
Based on the interventions employed and on the outcome at follow-up of the case reported herein, we conclude that root perforation can be overcome, and that a prolonged lifespan can be expected even in teeth affected by this complication.
REFERENCES
1. Alves DF, Gomes FB, Sayão SM, Mourato AP. Tratamento clínico cirúrgico de perfuração do canal radicular com MTA. Int J Dent. 2005;4:34-40. [ Links ]
2. Mente J, Hage N, Pfefferle T, Koch MJ, Geletneky B, Dreyhaupt J, et al. Treatment outcome of mineral trioxide aggregate: repair of root perforations. J Endod. 2010;36:208- 13.
3. Bernardes C, Fava AS, Borges Britto ML. Análise dos materiais de reparo no tratamento das perfurações radiculares. Revisão da literatura. EJER Eletron J Endod Rosario [Internet]. 2005 [cited 2014 Jul 08]; 1(4). Available from: http://rephip.unr.edu. ar/bitstream/handle/2133/1398/29-59-1-PB.pdf?sequence=1
4. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006;13:95-107.
5. Cogo DM, Vanni JR, Reginatto T, Fornari V, Baratto Filho F. Materiais utilizados no tratamento das perfurações endodônticas. Rev Sul-Bras Odontol. 2009;6:195-203.
6. Juarez Broon N, Bramante CM, de Assis GF, Bortoluzzi EA, Bernardineli N, de Moraes IG, et al. Healing of root perforations treated with mineral trioxide aggregate (MTA) and Portland cement. J Appl Oral Sci. 2006;14:305-11.
7. Silva Neto UX, Moraes IG. Capacidade seladora proporcionada por alguns materiais utilizados em perfurações na região de furca de molares humanos extraídos. J Appl Oral Sci. 2003;11:27-33.
8. Ruiz PA. Perfurações endodônticas: revisão de literatura. Rev Bras Patol Oral. 2003;2:45-50.
9. Tanomaru Filho M, Tanomaru JMG, Faleiros FCB. Capacidade seladora e adaptação de materiais utilizados em perfurações de furca. Rev Fac Odontol Lins. 2004;16:19-24.
10. Krupalini KS, Udayakumar, Jayalakshmi KB. A comparative evaluation of medicated calcium sulphate, hydroxylapatite, mineral trioxide aggregate (MTA) as barrier and their effect on the sealing ability of furcation perforation repair material--an in vitro study. Indian J Dent Res. 2003;14:156-61.
11. Menezes R, da Silva Neto UX, Carneiro E, Letra A, Bramante CM, Bernadinelli N. MTA repair of a supracrestal perforation: a case report. J Endod. 2005;31:212-4.
12. Tanomaru Filho M, Faleiros FCB, Tanomaru JMG. Capacidade seladora de materiais utilizados em perfurações endodônticas laterais. Rev Fac Odontol Lins. 2002;14:40-3.
13. Tanomaru Filho M, Mazotti D, Tanomaru JMG. Capacidade seladora de materiais empregados em perfurações radiculares. Rev ABO Nac. 2003;11:230-2.
14. Melo PAV, Travassos RMC, Dourado AT, Ferreira GS. Perfuração radicular cervical: relato de um caso clinico. Rev Odontol Univ Cid São Paulo. 2011;23:266-72.
15. Behnia A, Strassler HE, Campbell R. Repairing iatrogenic root perforation. J Am Dent Assoc. 2000;131:196-201.
16. Gomes SC, Miranda LA, Soares I, Oppermann RV. Clinical and histologic evaluation of the periodontal response to restorative procedures in the dog. Int J Periodontics Restorative Dent. 2005;25:39-47.
17. Camilleri J, Pitt Ford TR. Mineral trioxide aggregate: a review of the constituents and biological properties of the material. Int Endod J. 2006;39:747-54.
18. Silveira LFM, Cavalheiro GT, Heverson LCR, Martos J. Resolução clínica de perfuração radicular através de selamento com agregado de trióxido mineral (MTA). Int J Dent. 2010;9:220-4.
19. de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study--phases 3 and 4: orthograde retreatment. J Endod. 2008;34:131-7.
20. Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review--part II: leakage and biocompatibility investigations. J Endod. 2010;36:190- 202.
21. Dreger LA, Felippe WT, Reyes-Carmona JF, Felippe GS, Bortoluzzi EA, Felippe MC. Mineral trioxide aggregate and Portland cement promote biomineralization in vivo. J Endod. 2012;38:324-9.
22. Shimabuko DM. Avaliação in vitro do selamento marginal obtido quando do uso de associações de materiais no tratamento de perfurações de furca em molares humanos. Ecler Endod [Internet]. 2000 [cited 2014 07 Jun]. Available from: http://ecler.bvs.br/scielo. php?script=sci_arttext&pid=S1516-40552000000100002&lng=en&nrm=iso&tlng=pt.
 Correspondence:
Correspondence:
Ronise Ferreira Dotto
Rua Fernando Abott 391/404
CEP 96810-072, Santa Cruz do Sul, RS, Brazil
E-mail: ronisef@unisc.br













