Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.20 no.38 Canoas Jan./Jun. 2014
External cervical resorption: clinical case report
Reabsorção externa cervical: relato de caso clínico
Daniela Hansel I; Luis Eduardo Duarte Irala II
I Dental surgeon and a graduate student at the Lato Sensu Graduate Program in Endodontics of São Leopoldo Mandic, Porto Alegre, RS, Brazil
II Dental surgeon with Lato Sensu degrees in Restorative Dentistry and Endodontics and a MSc degree in Endodontics; he is a professor of Endodontics at Universidade Luterana do Brasil (ULBRA), Canoas, RS, Brazil; and head of the Lato Sensu Graduate Program in Endodontics at São Leopoldo Mandic, Porto Alegre, RS, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
External cervical resorption (ECR) is an invasive type of resorption that begins below the gingival epithelium and affects mineralized tissues, e.g., cementum and dentin. Most authors refer to dental trauma, whitening agents, and orthodontic treatment as etiologic factors of ECR; clinical diagnosis is performed via inspection of the gingival groove and margin. In this scenario, cone beam computed tomography has become a highly valuable ancillary method, as it allows to assess the proximity between the resorption and the pulp cavity, and thus, plan treatment. This article describes, in the form of a clinical case report, the diagnosis and treatment of a case of ECR affecting tooth no. 11, classified as Class III according to Heitersay’s classification. Surgical approach, restoration and clinical follow-up over 2-years of follow-up are described. In view of the clinical and radiographic findings observed during follow-up, it can be concluded that treatment was successful in healing periodontal tissues, suggesting a good prognosis.
Keywords: Tomography, Tooth Resorption, Diagnosis.
RESUMO
Reabsorções cervicais externas são reabsorções invasivas que iniciam abaixo da junção epitelial, atacando os tecidos mineralizados, como cemento e dentina. A maioria dos autores coloca como etiologia dessas lesões os traumatismos, agentes clareadores ou ortodontia, sendo seu diagnóstico clínico realizado através da inspeção da margem ou do sulco gengival. Nesse sentido, um dos recursos semiotécnicos auxiliares de grande validade constitui-se na tomografia cone beam, onde se consegue verificar a proximidade da reabsorção com a cavidade pulpar e, assim, planejar o tratamento. Este artigo relata, através de um caso clínico, o diagnóstico e tratamento de uma reabsorção externa cervical do dente nº 11, classificada de acordo com Heitersay como classe III, desde sua abordagem cirúrgica, restauração da cavidade e resolução clínica com um acompanhamento pelo período de 2 anos. Levando em consideração os achados clínicos e radiográficos dentro do período de observação, verificou-se que o tratamento apresentou uma boa resolução dos tecidos periodontais, o que dá indícios de um bom prognóstico para o caso.
Palavras-chave: Tomografia, Reabsorção de Dente, Diagnóstico.
INTRODUCTION AND LITERATURE REVIEW
External cervical resorption (ECR) is a type of dental resorption that begins below the gingival epithelium and which is not caused by etiologic factors related to dental trauma, orthodontic treatment, internal whitening, tooth reimplantation, periodontal treatment, surgical procedures, traction of teeth, tooth fractures or other such factors 1-9.
ECR involves a physiological or pathological event primarily caused by the action of activated clasts, characterized by the progressive or transitory loss of cementum or cementum and dentin 10.
Notwithstanding, to date, this type of external resorption is not yet very well understood 8. Sometimes it is even misdiagnosed, leading to incorrect treatment or unnecessary loss of the tooth. Treatment may include periodontal surgery and dental pulp involvement is possible 11.
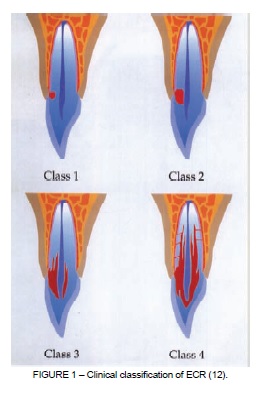
Heithersay 12 has established a clinical classification of ECR (Figure 1). The classification comprises four classes depending on degree of damage to mineralized tissues. Class I is a minor invasion of resorption close to the cervical, in Class II resorption damage is well-defined and close to the pulp chamber, in Class III the resorption damage has reached the cervical third of the root and in Class IV the damage attains the mid third of the root and may even cause it to fracture 3,4,5,8,12,13.
While it is known that one of the functions of the cementum is to protect root dentin from resorption, any damage that is suffered by this tissue can result in exposure of the root dentin to osteoclasts and, therefore, initiate the resorption process 13. Failure of the epithelium sulcular to migrate after removal of the cementum makes it possible for connective tissue to come into contact with dentin, and this is a decisive factor in initiating the osteoclastic resorptive process 2.
Consolaro 2, claims that dentin exposed through small windows at the cementoenamel junction is protected by the extracellular matrix and by the intermediate cementum in the micro-environment formed together with gingival soft tissues and connective and junctional epithelium. The aggression via dentin and gingiva triggers an inflammatory process which disorganizes the region of the cementoenamel junction. ECR is the result of cell mobilization mediated by the immune system to eliminate these proteins incorporated into the dentin during odontogenesis, but are not recognized as belonging. These structural characteristics mean that the cementoenamel junction can be considered the weak point of the tooth, or its Achilles heel.
Histologically, the resorption site is characterized by fibrous tissue fibrous tissue, highly vascularized, with multinucleated osteoclast cells along the surface of the dentin. Since infectious microorganisms are rarely found in these tissues, it is clear that the nature of this process is purely inflammatory 14.
A fine layer of dentin and pre-dentin separate the resorption tissue from the dental pulp, which remains free from inflammation until the end of the process. The resorption tissue is generally free from inflammatory cells, unless the lesion has been invaded by oral microorganisms. These early lesions contain fibrovascular tissue, but appear to develop into fibro-osseous lesions, by deposition of ectopic calcifications, such as bone, both in the interior of the resorption tissue and directly onto the surface of resorbed dentin 15.
Points of resorption are created deep into the dentin and around the root canal, joining more apically with the periodontal ligament. As a result, a delta of channels can form, with the effect of increasing the potential for resorption. Ectopic calcifications, which are deposited in the interior of the resorption tissue and directly onto the surface of dentin, have a canalicular structure with inclusion bodies and looks similar to spongy bone 15.
On radiography, recent damage shows as a nebulous radiolucent area at the root, with ill-defined edges. The canal walls are visible, and show through the radiolucent defect, indicating that the damage is on the external surface of the root; expansion is predominantly lateral, creating large affected areas on the root surface, although shallow, particularly during the initial phases 6.
ECR is generally painless, because the pulp remains protected behind a thin layer of pre-dentin until the end of the process 15.
While this type of resorption may be visible clinically as a pink coronary discoloration, followed by pitting of the enamel, there are often no obvious external signs and the condition is detected radiographically 1.
If the lesion is not detected or is left untreated, the result is cavitation of the enamel covering the resorption tissue 12.
Periapical X-rays are often insufficient to afford a safe and precise analysis of dental resorptions and clinicians will need to employ other sources of data to make the diagnosis more conclusive. In some cases computed tomography may be required, which facilitates analysis of resorption and determination of its extent and location, increasing diagnostic precision 2.
Treatment is based on removal of the soft tissue within the resorption defect and restoration with a permanent filling material 3. Glass ionomer, photopolymerizable composite resin, amalgam and mineral trioxide aggregate (MTA) have all been recommended for restoration of resorption damage 9.
Normally, this type of resorption does not communicate with the root canal and therefore endodontic treatment should not be performed in all cases. However, in clinical practice, when resorption is very close to the pre-dentin, the pulp may be exposed during curettage. In very extensive resorption cases, the decision may be taken to conduct endodontic treatment before completion of treatment for resorption 5.
The success of ECR treatment is dependent on the extent of the resorption process. In cases of Class IV cervical resorption, no alternative treatment is recommended. It is highly desirable that lesions are diagnosed during the initial phases and so patients who are prone to suffer this condition should be monitored radiographically at intervals throughout life 15.
In view of the above, and as shown in the case described below, early diagnosis and correct treatment are key to good prognosis in these cases 11.
CASE REPORT
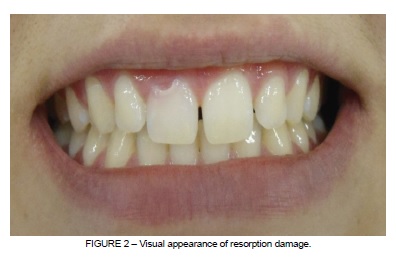
A 16-year-old female patient presented for a consultation at the dental clinic at the Faculdade São Leopoldo Mandic, Porto Alegre, Brazil, complaining of a pink-colored stain in the cervical region of her upper right central incisor. She did not complain of pain in the area, but there was bleeding during brushing (Figure 2).
Clinically, the patient underwent examination of the region using a periodontal probe, finding the cavity rough and observing slight bleeding when displaced from its position. A pulp sensitivity test at -20º was conducted (Aerojet Química Industrial LTDA, Duque de Caxias, RJ, Brazil), indicating vital pulp, and a periapical X-ray was taken to aid in diagnosis (Figure 3).

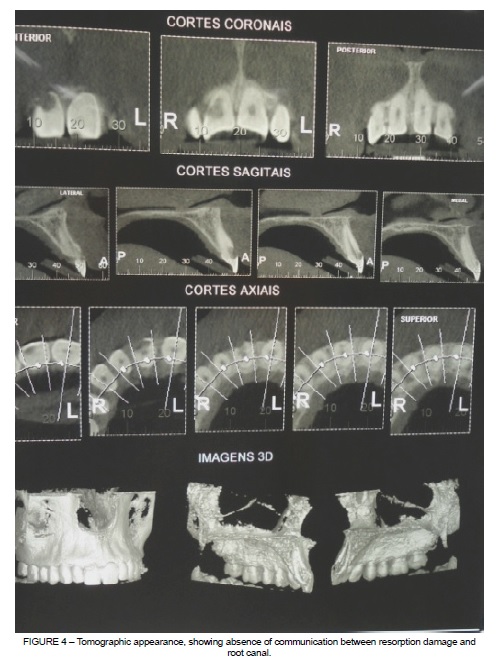
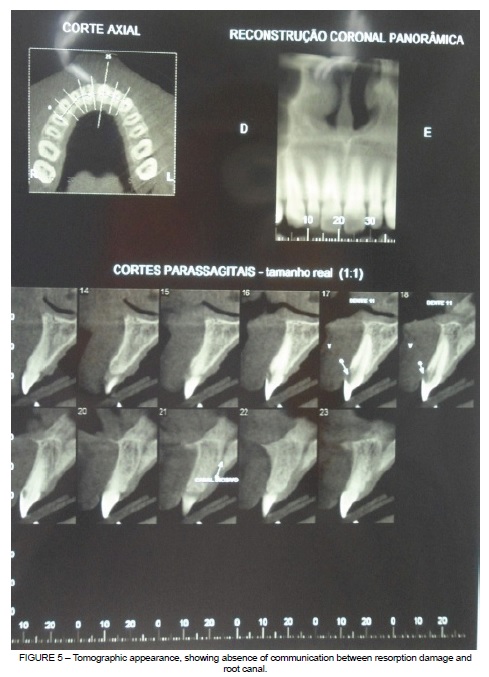
In view of these characteristics, the patient was diagnosed with a Heithersay Class III ECR, positive for sensitivity to cold. A cone beam tomography scan was used to investigate the depth of the damage and its proximity to the pulp chamber (Figures 4 and 5).
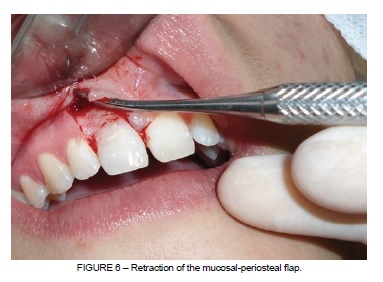
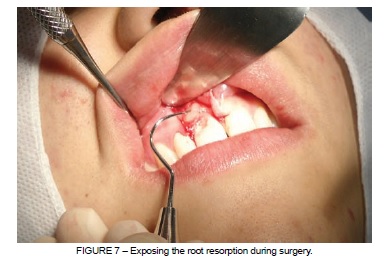
A surgical intervention was conducted in which a mucosal-periosteal flap was created with an intra-sulcular incision and a relaxation at the distal region of element 11, in order to reveal the root resorption damage and facilitate removal of the granulomatous tissue, making it possible to restore the cavity and resorption damage (Figures 6 and 7).
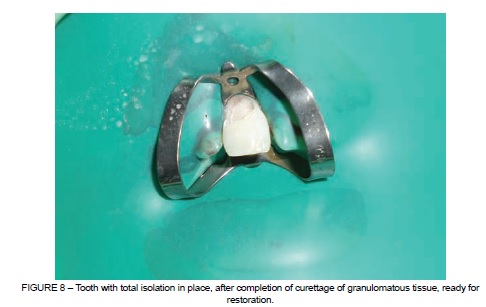
Next, the tooth was prepared with total isolation (Figure 8) and the cavity was restored with glass ionomer (Maxxion R – FGM., Joinville, SC, Brazil), and photopolymerizable composite resin (Charisma Heraeus Kulzer, Wehrheim, Germany). The restoration was finished using silicone tips (Enhance – Dentsply, Petrópolis, RJ, Brazil) (Figure 9).

The flap was repositioned in its original location and sutured using individual stitches in 3.0 silk suture thread (Ethicon – Johnson & Johnson do Brasil, São Paulo, SP, Brazil) (Figure 10).

Instructions for postoperative care covered administration of analgesic (500mg Metamizole Sodium every 6 hours for 3 days) and chemical control of supragingival biofilm with a 0.12% Chlorhexidine Gluconate solution (every 12 hours for 7 days). The patient was also instructed to treat the wound with ice during the first 24 hours, to eat cold or chilled food with a liquid or pasty consistency for 24 hours and to avoid physical exertion for 1 week.
Sutures were removed after 7 days and no intercurrent conditions interfered with healing (Figure 11).

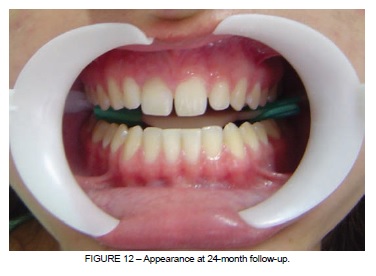
The patient returned for follow-up consultations after 30 days and after 6, 12 and 24 months. Her clinical status was of normal neighboring tissues, absence of symptomology and positive for sensitivity (Figure 12).
DISCUSSION
Treatment of ECR is a clinical challenge for which the literature describes several treatment options and the choice of which to employ is primarily dependent on the extent of the resorption process 13.
External coronary resorption is rarely diagnosed early and is generally an incidental clinical finding, as was the case with this patient who had been diagnosed with gingivitis. Therefore, in order to correctly diagnose ECR, in addition to clinical examination, clinicians will need to use a supplementary examination such as periapical radiography, or even computed tomography or cone beam computed tomography, which was employed in this case in order to assess the extent and position of damage with relation to the pulp chamber 5. Consolaro 16 has pointed out that errors with diagnosis are still common with relation to interpretation of periapical x-rays, with cervical resorption misdiagnosed as cervical caries, resorption by substitution wrongly identified as alveolar-dental ankylosis and external resorption mistaken for internal resorption, etc.
The extent of resorption serves as a guide for clinicians in the selection of the correct treatment material, taking into account aesthetic requirements and patient wishes; which in this case led to the decision to create a glass ionomer lining before restoring the tooth with photopolymerizable resin 14.
After taking the patient’s history and conducting clinical and radiographic examinations, the case described here was classified as Heithersay Class III ECR, with vital pulp. Differential diagnosis to rule out caries of the root consists of introducing an exploratory probe into the cavity and testing for a roughened and hardened surface.
With regard to possible etiology in this case, the patient had undergone orthodontic treatment previously. As Macalossi et al. 5 have pointed out, if excessive force is applied to the cervical region of the tooth during orthodontic treatment, necrosis may set in in adjacent tissues, leading to exposure of dentin and triggering the ECR process.
According to Lopes et al. 10, when damage takes the form of a wide crater, in which a part of the pathological process is intraosseous and the remainder is supraosseous, treatment consists of surgical exposure of the damage, removal of granulation tissue and restoration of the resorbed area.
The treatment chosen for the case presented here was therefore a combination of surgical and restorative treatments. Endodontic treatment was not needed because the tooth had vital pulp and there was no communication between resorption and the pulp chamber or root canal, with no intracanal contamination via the resorption.
During surgery, it was necessary to perform curettage of the granulomatous tissue, thereby interrupting the supply of blood to resorption cells and so reducing the probability of relapse, as suggested by Patel et al. 8.
Clinical and radiographic follow-up is essential to assess the success of treatment for External Resorption Cervical and so, in this case, the patient was seen at 30 days, and at 6, 12 and 24 months for assessment. After just 30 days the appearance was normal, and the patient was asymptomatic, had no periodontal pocket and had healthy gingiva with normal color and texture that exhibited sensitivity to cold 1.
CONCLUSIONS
The restorative surgical treatment conducted in this ECR case effectively resolved the case, to the extent that, over a 2-year period, follow-up assessments found a tooth with normal function and esthetics, healed adjacent tissues and sensitivity to cold, confirming good prognosis in this case.
REFERENCES
1. Camargo SEA, Moraes MEL, Moraes LC, Camargo CHR. Principais características clínicas e radiográficas das reabsorções radiculares internas e externas. Rev Odontol Univers Cidade Sao Paulo. 2008;20(2):195-203. [ Links ]
2. Consolaro A. Reabsorções dentárias nas especialidades clínicas. 2ª ed. Maringá: Dental Press; 2005. 616p.
3. Estevez R, Aranguren J, Escorial A, Gregorio C, Torre F De La, Vera J, Cisneros R. Invasive cervical resorption class III in a maxillary central incisor: diagnosis and followup by means of cone-beam computed tomography. J Endod. 2010;36(12):2012-4.
4. Gulsahi A, Gulsahi K, Ungor M. Invasive cervical resorption: clinical and radiological diagnosis and treatment of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(3):65-72.
5. Macalossi JMS, Back EDEE, Haragushiku GA, Tomazinho FSF, Filho FB. Etiologia, diagnóstico e tratamento da reabsorção cervical externa – revisão de literatura. Odonto. 2012;20(39):71-80.
6. Macieira MM, Justo AM, Só MVR, Santos RB dos, Magro ML, Kuga MC. Diagnóstico radiográfico diferencial das reabsorções radiculares internas e externas entre especialistas em endodontia e clínicos gerais. RFO Passo Fundo. 2011;16(3):273-6.
7. Nascimento GJF, Emiliano GBG, Silva IH de M, Carvalho RA, Galvão HC. Mecanismo, classificação e etiologia das reabsorções radiculares. Rev Fac Odontol Porto Alegre. 2006;47(3):17-22.
8. Patel S, Kanagasingam S, Ford TP. External cervical resorption: a review. J Endod. 2009;35(5):616-25.
9. Ylmaz HG, Kalender A, Cengiz E. Use of mineral trioxide aggregate in the treatment of invasive cervical resorption: a case report. J Endod. 2010;36(1):160-3.
10. Lopes HP, Junior JFS. Endodontia: biologia e técnica. 3ª ed. Rio de Janeiro: Guanabara Koogan; 2011. 951p.
11. Schwartz RS, Robbins W, Rindler E. Management of invasive cervical resorption: observations from three private practices and a report of three cases. J Endod. 2010;36(10):1721-30.
12. Heithersay G S. Invasive cervical resorption following trauma. Austr Endod J. 1999;25(2):79-85.
13. Barnabé W, Souza JB, Lopes L, Ruiz LFN, Freitas PH, Neto TM. Abordagem interdisciplinar no tratamento de reabsorção cervical externa: relato de caso. Rev Odontol Brasil Central. 2011;20(55):359-65.
14. Smidt A, Nuni E, Keinan D. Invasive cervical root resorption: treatment rationale with an interdisciplinary approach. J Endod. 2007;33(11):1383-7.
15. Heithersay GS. Clinical, radiologic and histopathologic features of invasive cervical resorption. Quintessence Int. 1999;30:27-37.
16. Consolaro A. A tomografia computadorizada substitui as radiografias periapicais no diagnóstico das reabsorções dentárias? Rev Clin Ortod Dental Press. 2007;6(5):110-1.
 Correspondence:
Correspondence:
Daniela Hansel
Rua Fernando Abott, 265/401B
CEP 96810-160, Santa Cruz do Sul, RS, Brazil
E-mail: danielahansel@yahoo.com.br













