Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.20 no.39 Canoas Jul./Dez. 2014
Treatment of actinic cheilitis by surgical vermilionectomy
Tratamento da queilite actínica através da técnica cirúrgica da vermelhectomia
Sergio Augusto Quevedo Miguens Jr. I; Humberto Thomazi Gassen II; Milene Castilhos de Oliveira III; José Luiz Fontoura Junior IV; Aurelício Novaes Silva Jr. V; Pedro Antonio González Hernández VI
I PhD in Oral Medicine and an adjunct professor at the School of Dentistry at Universidade Luterana do Brasil (ULBRA), Canoas, RS, Brazil
II MSc in Oral and Maxillofacial Surgery and Traumatology and anadjunct professor at the School of Dentistry at ULBRA, Canoas, RS, Brazil
III Dental surgeon, Graduate Program in Dentistry, School of Dentistry, Universidade Luterana do Brasil, Campus Canoas (ULBRA), Canoas, RS, Brazil
IV Dental student at ULBRA, Canoas, RS, Brazil
V PhD in Oral and Maxillofacial Surgery and Traumatology and an adjunct professor at the School of Dentistry at ULBRA, Canoas, RS, Brazil
VI PhD in Esthetic Dentistry and an adjunct professor at the School of Dentistry at ULBRA, Canoas, RS, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
Actinic cheilitis is a potentially premalignant condition that is primarily found on the lower lip. Etiology is related to chronic exposure to ultraviolet light and the condition exhibits a strong predilection for people whose work involves intense exposure to the sun. Clinically observable signs include white or reddened areas of maculation or whitish plaques caused by hyperkeratinization of the lip epithelium, which can progress to a point at which the demarcation between the skin, vermillion border of the lip and the mucosa is lost. These lesions are generally asymptomatic but may progress to form areas of erosion and/or ulceration. There are a number of treatments available, one of which, vermilionectomy, is a surgical procedure in which the vermillion border of the lip is partially or totally removed and which, in addition to being inexpensive, offers the advantage of providing material for pathological analysis. The objective of this study is to describe the vermilionectomy technique as used to treat a patient diagnosed with actinic cheilitis.
Keywords: Cheilitis, Precancerous Conditions, Photosensitivity Disorders.
RESUMO
A queilite actínica é uma lesão cancerizável que acomete principalmente o lábio inferior, cujo fator etiológico está relacionado à exposição crônica aos raios ultravioletas. Possui uma predileção aumentada por indivíduos que apresentam atividade laboral com intensa exposição ao sol. Clinicamente, observam-se áreas maculares brancas ou avermelhadas ou lesões em forma de placas esbranquiçadas resultantes da hiperceratinização do epitélio do lábio, a qual pode progredir para a perda do limite entre a pele, vermelhão do lábio e a mucosa. Essas lesões são geralmente assintomáticas e podem progredir para áreas erosivas e/ou ulceradas. Dentre as diversas formas de tratamento, há a vermelhectomia, que consiste num procedimento cirúrgico para a remoção parcial ou total do vermelhão do lábio, apresentando baixo custo e permitindo a disponibilidade de material para exame anatomopatológico. O objetivo desse trabalho é relatar a técnica de vermelhectomia no tratamento de um paciente com diagnóstico de queilite actínica.
Palavras-chave: Queilite, Transtornos de Fotossensibilidade, Lesões Pré-Cancerosas.
INTRODUCTION
Actinic cheilitis (AC) is a potentially premalignant condition involving the vermillion border of the lips, which is also known as exfoliative cheilitis, solar cheilitis, solar keratosis and actinic keratosis 1-3. The principal etiologic factor is ultraviolet B radiation (UVB), which triggers changes to proteins and DNA that initiate and promote dysplastic changes to the epidermis 4,5.
AC is most common among white-skinned people, males, individuals over the age of 50 and those who engage in outdoor activities and/or have a history of chronic exposure to the sun 3,5, since the lower lip is the structure that is most vulnerable to solar radiation damage 6,7.
Clinically, AC manifests as discoloration and loss of mucosal elasticity, erosions, atrophy, erythema and ulceration, in addition to a blurring of the demarcation between the vermillion border of the lip and the skin 1,2,7. The lesion also most often presents as red or white areas or areas of white interspersed with red 4. Investigation of the histological features of AC has shown that in around 100% some type of abnormality, such as solar elastosis or dysplasia, is observable 7.
Although AC is one of a number of lesions that are easily detected during clinical examination, late diagnosis can be attributed to certain factors, such as lack of awareness, lack of symptomology and because the initial clinical presentation appears inoffensive 1,6. There is an acknowledgement among clinicians that lip squamous cell carcinoma is often reported alone with no coincident diagnosis of AC 7.
While AC can be avoided or monitored by wearing hats, caps and lip sunscreens, a biopsy should be conducted and the lesion treated if the signs persist or worsen 8,9. Patients who are continuously exposed to sunlight should undergo regular screening and should receive more careful treatment 4.
The prognosis of AC is variable and depends on histological diagnosis and on adoption of lifestyle changes and self-care on the part of the patient 4.
The most widely used treatments are all intended to eliminate or destroy the abnormal epithelium and include vermilionectomy, topical administration of 5-fl uorouracil (5-FU), cryotherapy, electrocauterization, carbon dioxide laser ablation, and photodynamic therapy, among others 1,3,10,11.
Vermilionectomy is a surgical procedure that consists of partial or total removal of the vermillion border from the lips. The surgical technique involves removal of the damaged tissues of the vermillion border of the lip above the plane of the orbicularis oris muscle, covering the wound by advancing healthy internal labial mucosa 2,9. The technique was described for the first time by Von Esmarch & Kiwalzik 12 and is indicated for treatment of precancerous lesions such as AC or in situ squamous cell carcinoma. It has been widely accepted as a method for removing diffuse dysplastic lesions from the lips and also provides material for pathological analysis to aid in determination of the extent of the disease process 3,9.
The technique involves the possibility of postoperative complications such as formation of hematoma, dehiscence of the wound, formation of infl exible scar tissue, loss of the profile of the lips and development of paresthesias 3. On the other hand, it is a rapid method with a short postoperative recovery period and low rates of complications and is an effective method of prophylaxis against squamous cell carcinoma of the lips 13,14, in addition to being conducted with local anesthesia, in outpatients settings, and offering very satisfactory esthetic results 9.
The objective of this study is to describe the vermilionectomy technique as used to treat a white-skinned, 69-year-old patient diagnosed with AC.
CASE REPORT
A white-skinned, 69-year-old male patient, who was a retired driver presented at the Stomatology Service at the University Hospital at the Universidade Luterana do Brasil (ULBRA Canoas) after referral for investigation of white areas on his lower lip.
During history taking, the patient reported being a smoker for 30 years with a frequency of three cigarettes a day and a type II diabetic with hypertension, taking 5mg of glibenclamide once a day, 25 mg of Hydrochlorothiazide once a day, 100mg of AAS once a day, 20mg of simvastatin once a day and 20mg of enalapril twice a day.
Physical examination revealed whitish plaques involving the vermillion border of the lower lip (Figure 1A) that had been present for 1 year, were not removed by scraping, and had sessile bases, imprecise borders and rough surface with palpable, painless and moveable submandibular glands on the left side.
In view of these clinical findings, a diagnostic hypothesis of AC was established and the initial treatment chosen was total excision of the whitened areas in conjunction with the vermillion border of the lip. Since the area affected by the lesions was considerable, the excision surgery was planned as two distinct procedures.
The initial steps consisted of extra-buccal antisepsis with 2% chlorhexidine digluconate followed by intra-buccal antisepsis with 0.12% chlorhexidine digluconate. The mental nerves were blocked by local anesthesia with 2% mepivacaine with adrenaline 1:100.000 in a volume of approximately 1.8 ml plus local supplementary doses with the objective of maintaining hemostasis, to a volume of approximately 0.6 ml. A linear incision was made using a nº15 scalpel blade, following the path of the vermillion border and leaving a 2 millimeter margin of apparently healthy tissue, to a depth of 2 millimeters, sufficient to remove the vermillion border of the lip and expose the muscle tissue as far as the medial line (Figure 1B).
After partial removal of the lesion, the tissue fragment (Figure 1C) was immediately stored in a quantity of 10% buffered formalin 20 times the volume of the specimen and sent for pathological analysis.
The edges of the surgical wound were drawn together using single-stitch sutures in 4-0 nylon monofilament (Figure 1D), bringing the healthy internal labial mucosa to the edge of the incision in the skin.
Postoperative medications prescribed were 500mg Amoxycillin every 8h for 7 days, 1g Dipyrone every 6h for 3 days, wound hygiene with 0.9% saline solution and application of Bepantol Derma® to the wound at night, in addition to the routine care provided to surgical outpatients.
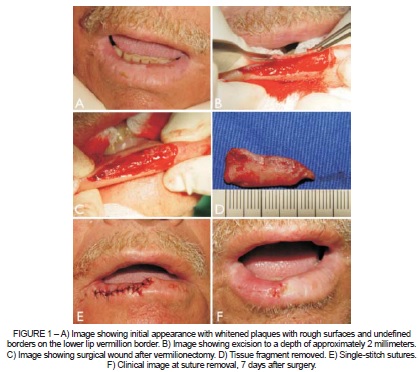
Sutures were removed 7 days after surgery and the patient was instructed to apply Bepantol Derma® at night and sunscreen with a protection factor of 30 during the day.
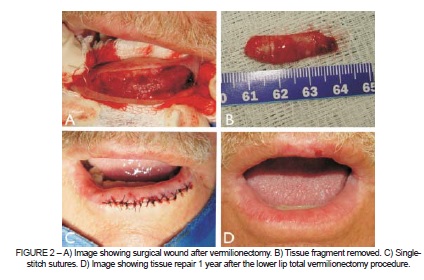
Twenty-eight days later, vermilionectomy was performed for the left side, using the same surgical technique and criteria as in the first procedure (Figure 2A-C).
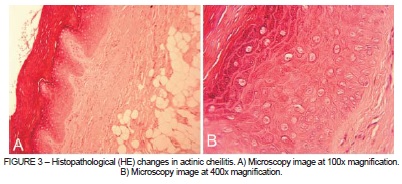
Microscopy analysis with Hematoxylin and Eosin (HE) staining showed stratified squamous epithelial tissue with areas of atrophy and hyperkeratosis (Figure 3A). The epithelial tissue exhibited duplication of the basal layer, atypical mitoses, acanthosis and abnormal stratification (Figure 3B). Microscopic diagnosis was mild epithelial dysplasia.
The patient is currently attending three-monthly clinical follow-up consultations at which, in addition to providing guidance with relation to protection from the sun, physical examinations are carried out to screen for changes in color, consistency and surface of the lips.
FINAL COMMENTS
Although there are a number of treatments for AC, recurrence is common. Each treatment offers advantages and disadvantages and all can be conducted successfully in outpatient settings.
Vermilionectomy is the treatment of choice because it enables pathological analysis of all of the tissues that are removed. Notwithstanding, irrespective of which treatment is chosen, no treatment will be effective if the patient is not aware of the importance of post-diagnosis care and of regular consultations with a health professional to screen for possible recurrence of the disease, in addition to consolidating habits relating to continuous protection from the sun.
As such, the dental surgeon's task with relation to these patients is to educate, to prevent, to diagnose, to treat and to follow-up, since this is a lesion that is both premalignant and easily treated.
REFERENCES
1. Nico MMS, Rivitti EA, Lourenço SV. Actinic cheilitis: histologic study of the entire vermilion and comparison with previous biopsy. J Cutan Pathol. 2007;34:309-14. [ Links ]
2. Barry RB, McKenzie J, Berg D, Langtry JA. Direct primary closure without undermining in the repair of vermilionectomy defects of the lower lip. Br J Dermatol. 2012;167:1092-7.
3. Shah AY, Doherty SD, Rosen T. Actinic cheilitis: a treatment review. Int J Dermatol. 2010;49:1225-34.
4. de Santana Sarmento DJ, da Costa Miguel MC, Queiroz LM, Godoy GP, da Silveira EJ. Actinic cheilitis: clinicopathologic profile and association with degree of dysplasia. Int J Dermatol. 2014;53:466-72. Epub 2013 Dec 10.
5. Kaugars GE, Pillion T, Svirsky JA, Page DG, Burns JC, Abbey LM. Actinic cheilitis: a review of 152 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:181-6.
6. Vieira RA, Minicucci EM, Marques ME, Marques SA. Actinic cheilitis and squamous cell carcinoma of the lip: clinical, histopathological and immunogenetic aspects. An Bras Dermatol. 2012;87:105-14.
7. Savage NW, McKay C, Faulkner C. Actinic cheilitis in dental practice. Austr Dent J. 2010;55:78-84.
8. Instituto Nacional de Câncer [Internet]. 2013 Nov cited 2013 Nov 26]. Available from: http://www2.inca.gov.br/wps/wcm/connect/ tiposdecancer/site/home/boca
9. Kurul S, Uzunismail A, Kizir A. Total vermilionectomy: indications and technique. Eur J Surg Oncol. 1995;21:201-3.
10. Hauschild A, Lischner S, Lange-Asschenfeldt B, Egberts F. Treatment of actinic cheilitis using photodynamic therapy with methyl aminolevulinate: report of three cases. Dermatol Surg. 2005;31:1344-7, discussion 1348.
11. Ribeiro CF, Souza FH, Jordão JM, Haendchen LC, Mesquita L, Schmitt JV, et al. Photodynamic therapy in actinic cheilitis: clinical and anatomopathological evaluation of 19 patients. An Bras Dermatol. 2012;87:418-23.
12. Von Terheyden H, Fleiner B, Koch G. Contour of the lower lip after von Esmarch reconstruction of lower lip vermilion. Mund Kiefer Gesichtschir. 1997;1(Suppl 1):S113-6.
13. Picascia DD, Robinson JK. Actinic cheilitis: a review of the etiology, differential diagnosis, and treatment. J Am Acad Dermatol. 1987;17:255-63.
14. Johnson TM, Sebastien TS, Lowe L, Nelson BR. Carbon dioxide LASER treatment of actinic cheilitis. J Am Acad Dermatol. 1992;27:737-40.
 Correspondence:
Correspondence:
Sergio Augusto Miguens Jr
ULBRA, Curso de Odontologia, Departamento Diagnóstico Bucal
Rua Farroupilha, 8001, Prédio 59, Bairro São José, CEP 92425-900
Canoas, RS, Brasil
E-mail: samiguens@gmail.com













