Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.21 no.40 Canoas Jan./Jun. 2015
Intraosseous myofibroma of the jaw: Review of the literature
Miofibroma mandibular intraósseo: revisão de literatura
Roger Corrêa de Barros BertholdI; Thiago Aragon ZanellaII; Liliane Cristina Onofre CasagrandeII; Eduardo Madruga LombardoII; Claiton HeitzIII; Telmo Bandeira BertholdIV
I is doctoral student of Oral and Maxillofacial Surgery, Department of Oral and Maxillofacial Surgery, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil
II are Masters students of Oral and Maxillofacial Surgery, Department of Oral and Maxillofacial Surgery, PUCRS, Porto Alegre, RS, Brazil
III is chairman and professor, Department of Oral and Maxillofacial Surgery, School of Denstistry, PUCRS, Porto Alegre, RS, Brazil
IV is professor, Department of Orthodontics, PUCRS and Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
ABSTRACT
The objective of this study was to perform a review of the pathological features and treatment of intraosseous myofibroma of the jaw. Electronic searches were performed of MEDLINE, via Pubmed (from 1950 to November 2012), EMBASE and Cochrane Wiley, on November 27th, 2012, with no language restrictions. The electronic search yielded 41 hits, of which 27 articles were considered relevant after evaluation of titles and abstracts and underwent eligibility assessment according to the eligibility criteria Of these, 10 did not meet one or more inclusion criteria and were rejected. The 17 articles selected included three retrospective studies, 13 case reports and one case series. These articles reported on a total of 24 cases of solitary myofibroma in the jaw. Intraosseous myofibromas of the jaw are rare lesions and are part of the wide group of spindle-cell neoplasms and are generally observed in the posterior mandible. It is important to establish the appropriate treatment to avoid unnecessary aggressive therapy. Conservative surgery is the preferred option.
Keywords: Myofibroma; Mandibular Neoplasm; Treatment.
RESUMO
O objetivo deste estudo foi realizar uma revisão de literatura sobre miofibroma intraósseo da mandíbula, suas características patológicas e tratamento. Foi realizada uma busca eletrônica nas base de dados MEDLINE via Pubmed (1950 a novembro de 2012), EMBASE e Wiley Cochrane, no dia 27 de novembro de 2012 sem restrição de linguagem. A busca eletrônica resultou em 41 citações, e 27 artigos foram considerados relevantes pela leitura do título e pela avaliação do resumo. Desses 27 artigos, 10 não atenderam um ou mais critérios de inclusão e foram excluídos. Entre os 17 artigos selecionados, havia três estudos retrospectivos, 13 relatos de caso e uma série de casos. Vinte e quatro casos de miofibroma solitário intraósseo da mandíbula foram identificados. Miofibromas intraósseos dos maxilares são lesões raras que fazem parte do grupo de lesões neoplásicas fusiformes e são comumente encontrados na região posterior da mandíbula. É importante estabelecer o tratamento apropriado para evitar terapia agressiva desnecessária. Cirurgia conservadora é a opção desejada.
Palavras-chave: Miofibroma; Neoplasia Mandibular; Tratamento.
INTRODUCTION
A myofibroma is a benign solitary tumor formed of myofibroblasts, that mostly occurs in childhood 1,2. When multiple lesions are present, the condition is called myofibromatosis 2. It was first described by Stout in 1954 3 as congenital generalized myofibromatosis and in 1989, Smith 4 introduced the most widely accepted term, myofibroma, for solitary lesions. Myofibroma is a rare lesion, that is relatively more common in tissues of the head and neck and which can originate from soft tissue and bone 1. Approximately one third of myofibromas involve the jaws 1. Soft tissue myofibroma is the most common presentation and will often affect soft oral tissues such as the tongue, mucosa and gingiva 1-4. Intraosseous myofibromas are rare, especially in adults, but they are occasionally encountered within the mandible 5,6. Since this lesion is rarely seen in the mandible, it can be misdiagnosed as an odontogenic cyst or tumor, and there are previous reports of misdiagnosis preventing appropriate management 7,8. The main objective of this review is to identify the ideal management of intraosseous myofibromas. Their pathological features will also be described.
REVIEW OF THE LITERATURE
A review of the best evidence available in the literature was performed in order to answer the following question "What is the most appropriate treatment for intraosseous myofibroma of the jaw?"
Electronic searches were performed of MEDLINE, via Pubmed (from 1950 to November 2012), EMBASE and Cochrane Wiley, on November 27th, 2012, with no language restrictions. The search strategy employed was as follows: myofibroma of jaw OR jaw myofibroma OR intraosseous myofibroma OR central myofibroma OR myofibroma of mandible OR intraosseous myofibromatosis OR mandibular myofibroma. Two reviewers screened the articles retrieved by these searches. They were blinded to journal titles, in an attempt to avoid selection bias. The full text was retrieved for articles that appeared to be relevant and also for studies for which the titles and abstracts provided insufficient data for a decision. The reference lists of selected articles were also reviewed and once more full texts were retrieved for studies that appeared to be relevant or for which insufficient data were available. The articles selected after review of the full text were then sent for a final eligibility assessment. The criteria used to evaluate the studies were as follows: intraosseous site of lesion; studies that reported histopathologic and immunohistochemical findings; and studies that described treatments. As such, all articles that reported on treatment of intraosseous myofibromas of the jaw, confirmed by histopathological and immunohistochemical analysis, were included.
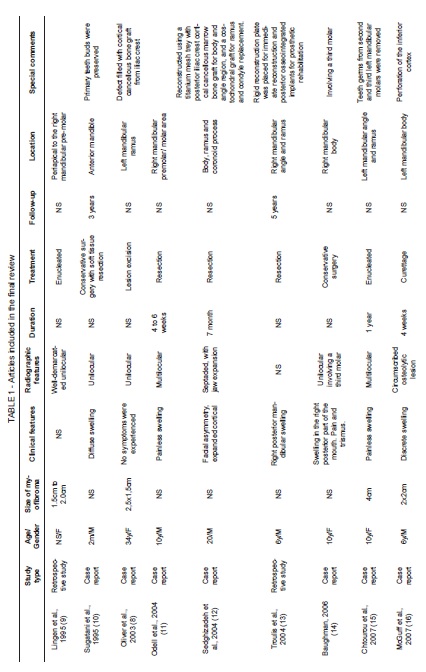
The electronic search yielded 41 hits (37 from Pubmed, 4 from EMBASE and 0 from Cochrane Wiley), of which 27 articles were considered relevant after evaluation of titles and abstracts and underwent eligibility assessment according to the eligibility criteria described above. Ten of these 27 articles did not meet one or more of the inclusion criteria and were therefore rejected. The reasons for exclusion were mostly because lesions were not intraosseous, but one study did not describe treatment and another study was about lesions that were not solitary. The articles included in the final review are listed in Table 1. The 17 articles selected include three retrospective studies, thirteen case reports and one case series. Altogether, these articles report on a total of 24 cases of solitary myofibroma in the jaw.
Age and location
According to the review, solitary intraosseous myofibroma affects patients aged 3 weeks to 43 years (with a mean of 12 years) with no predilection for gender; the studies report on 9 males and 11 females. Most patients were ten years old or younger. The most common location is the posterior mandible, including the body, angle, condyle, coronoid process and ramus, but in 3 patients the site was in the anterior region of the mandible. A retrospective study by Abramowicz et al. 5 described the only two maxillary intraosseous myofibromas in the literature covered in this review. Both were located in the palate, but no computed tomography (CT) images or clinical details were provided 5.
Clinical and radiographic features
Painless swelling of the mandible was the most common symptom reported by patients. Swellings varied from discrete to extensive and led to facial asymmetry in two cases 12,19 and restricted mouth opening in one case 6. Restricted mouth opening was reported by Allon et al. 6, with relation to a patient with a myofibroma in the posterior mandible, involving the coronoid process. The lesion was excised together with a coronoidectomy, but a fracture of the ramus occurred during the procedure and the authors decided to remove the remaining ramus and condyle and preserve the condylar disk. At 6 month follow-up the patient's ability to open the mouth had improved (28 mm) but with deviation to the left. A further 6 myofibromas were asymptomatic and discovered as incidental findings 5,8. For example, in a case reported by Oliver et al. 8, the general dental practitioner discovered the myofibroma during the course of routine conservation treatment and the patient was completely unaware of the lesion, but some bucco-lingual expansion in the lower left third molar was found. Two patients experienced pain. One had a myofibroma associated with a third molar with possible pericoronaritis 14. Partial mental nerve hypoesthesia was reported in one case, in which the myofibroma was discovered incidentally on a panoramic radiograph taken after a facial trauma 17. The author did not state with certainty whether the myofibroma had been the cause of the hypoesthesia, neither whether sensitivity returned after excision of the lesion 17.
The sizes of these lesions were relatively small, ranging from 1 to 4.2 cm in diameter. Within the mandible, myofibromas can cause several complications, such as tooth dislocations and expansion and resorption of bone plates 9-21. Analyzing CT images from the series of 24 lesions, what was possibly the largest intraosseous myofibroma was reported by Sedghizadeh et al. 12. This fully occupied the posterior mandible with expanded cortical. However the authors did not provide the measurements and this study was not included in the size comparison.
The most frequent radiographic finding is of a unilocular radiolucent wellcircumscribed area, reported in 10 cases 6-8,9,10,14,16-18,20, but a unilocular lesion with septation was seen in one case 12, a bilocular lesion in one other case6 and multilocular lesions were seen in 4 cases 6,11,15,19, while indistinct margins may also be observed 11. Cortical expansion was reported frequently and appears to have no relation with the size of lesions, since there are reports of cortical expansion in lesions of small size that can also cause resorption of mandibular bone plates 16,17.
Histology and immunohistochemistry
Histopathologically, intraosseous myofibroma of the jaw and soft tissue myofibroma are indistinguishable 9,11,15. Histological features comprise a well-circumscribed spindle–cell neoplasm with alternating fascicular and cellular areas, characterized by peripheral elongated cells arranged in short fascicles and central round to polygonalshaped cells 12,17. The central cells are usually arranged around thin-walled, irregularly branching blood vessels in a hemangiopericytoma-like vascularity. Immunohistochemical analysis of intraosseous myofibroma of the jaw is also identical to soft tissue myofibroma 16-20. Cells from the lesions stained positive for vimentin and α-SMA, and were negative for desmin, S-100 protein, and cytokeratins 14,16.
Treatment
There are two distinct predominant treatment approaches to intraosseous myofibroma of the jaw: conservative surgery or mandibular segmental resection 9-21. Conservative surgery comprises a number of surgical techniques such as enucleation and curettage and is the most common technique used to treat these lesions, used in 20 of the cases reviewed.
There are 4 reports of mandibular resection as treatment for intraosseous myofibroma, two in adults and two in young boys 11-13,18. Troulis et al. 13 reported a case of a 6-year-old boy with intraosseous myofibroma in the right posterior mandible who was treated with a 4-stage protocol proposed by the same authors for oral rehabilitation of children with jaw tumors. The young boy underwent mandibular resection and a rigid reconstruction plate was used to maintain mandibular continuity and fix the bone segments. Around 12 months after the operation, reconstruction was performed with an iliac bone graft. Ten months after grafting, three implants were used for prosthetic rehabilitation. Another case of resection and reconstruction was reported by Sedghizadeh et al. 12. A 20-year-old male patient underwent hemimandibulectomy with reconstruction 8 weeks after using a titanium mesh tray with posterior iliac crest cortical cancellous marrow bone graft for the body and angle region and a costochondral graft for ramus and condyle replacement.
Since there were no recurrences in the reports evaluated for this review and the lesion is usually described as a well-circumscribed lesion, conservative surgery appears to be the treatment of choice 9-21. Some authors reported that during the operation it was possible to detach the lesion very easily from the mandibular bone 6,10. However, the follow-up period in some cases was very short, and in several cases it was not stated. In 7 cases, the follow-up period reported was greater than 1 year.
Intraosseous myofibromas of the jaw can often dislocate deciduous or permanent tooth buds, since they affect children 15. In 5 cases, dislocation or involvement of tooth buds was reported 6,10,15,21. Extraction of deciduous or permanent tooth buds was performed in 4 cases during excision of the lesions. Sugatani et al. 10 described a 2-month-old boy with intraosseous myofibroma who was treated with conservative surgery with preservation of primary tooth buds that were compressed mesiodistally in the mandible. The authors reported no signs of recurrence 3 years after surgery 10.
FINAL CONSIDERATIONS
Intraosseous myofibroma of the jaw is a rare lesion and is part of the wide group of spindle-cell neoplasms 21. Myofibromas must be differentiated from other pathological entities such as leiomyoma, neurofibroma, fibrosarcoma, leiomyosarcoma, hemangiopericytoma and desmoplastic fibroma 10. Awareness of myofibroma is important for establishment of the correct diagnosis and to avoid morbidity caused by unnecessarily aggressive therapy such as radiotherapy or extensive resections 10. The most commonly observed site is the posterior mandible and clinical and radiographic features are both non-specific, leading to a wide range of differential diagnoses, including odontogenic cysts when unilocular and tumors when multilocular 7,8. Therefore, an incisional biopsy must be performed and histological and immunohistochemical analysis is necessary to arrive at the final diagnosis of myofibroma 1,22. The most appropriate treatment for these lesions is conservative surgery, since they are usually circumscribed lesions that are easily detached from the mandible. However, there are no large series reporting treatment outcomes with appropriate follow-up periods 12,15,17,22.
REFERENCES
1. Foss RD, Ellis GL. Myofibromas and myofibromatosis of the oral region: a clinicpathological analysis of 79 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:57-65. [ Links ]
2. Chung EB, Enzinger FM. Infantile myofibromatosis. Cancer 1981;48:1807-18.
3. Stout AP. Juvenile fibromatosis. Cancer. 1954;7:953-78.
4. Smith KJ, Skelton HG, Barret TL, Lupton GP, Graham JH. Cutaneous myofibroma. Mod Pathol. 1989;2:603-9.
5. Abramowicz S, Simon LE, Kozakewich HP, Perez-Atayde AR, Kaban LB, Padwa BL. Myofibromas of the jaws in children. J Oral Maxillofac Surg. 2011;70:1880-4.
6. Allon I, Vered M, Buchner A, Dayan D. Central (intraosseous) myofibroma of the mandible: clinical, radiologic, and histopathological features of a rare lesion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e45-53.
7. Souza DP, Loureiro CC, Rejas RA, Sousa SO, Raitz R. Intraosseous myofibroma simulating an odontogenic lesion. J Oral Sci. 2009;51:307-11.
8. Oliver RJ, Coulthard P, Carre C, Sloan P. Solitary adult myofibroma of the mandible simulating an odontogenic cyst. Oral Oncol. 2003;39:626-9.
9. Lingen MW, MostofiRS, Solt DB. Myofibromas of the oral cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:297-302.
10. Sugatani T, Inui M, Tagawa T, Seki Y, Mori A, Yoneda J. Myofibroma of the mandible. Clinicopathological study and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:303-9.
11. Odell EW, Aldred M, Carlos R, Curran A, Heikinheimo K, Hille J, et al. Clinicopathological al conference 2002. Ann Acad Med Singapore. 2004;33(4 Suppl):53-8.
12. Sedghizadeh PP, Allen CM, Kalmar JR, Miloro M, Suster S. Solitary central myofibroma presenting in the gnathic region. Ann Diagn Pathol. 2004;8:284-9.
13. Troulis MJ, Williams WB, Kaban LB. Staged protocol for resection, skeletal reconstruction, and oral rehabilitation of children with jaw tumors. J Oral Maxillofac Surg. 2004;62:335-43.
14. Baughman R. Testing your diagnostic skills. Case No. 1: a relatively rare jaw neoplasm called a myofibroma. Todays FDA. 2006;18:22.
15. Chtourou I, Krichen Makni S, Dhouib M, Khabir A, Fakhfakh I, Ayadi L, et al. Pediatric mandibular myofibromatosis. Rev Stomatol Chir Maxillofac. 2007;108:461-4.
16. McGuff HS, Heim-Hall J, Jones AC, Cruz C. Oral and maxillofacial pathology case of the month. Myofibroma. Tex Dent J. 2007;124:1058-9.
17. Shibuya Y, Takeuchi J, Sakaguchi H, Yokoo S, Umeda M, Komori T. Myofibroma of the mandible. Kobe J Med Sci. 2008;54:E169-73.
18. Ramadorai A, Rajsekaran A, Narayanan V. A case report of solitary, intraosseous, adult-onset myofibroma of the mandible. J Maxillofac Oral Surg. 2010;9:280-3.
19. Rokos J, Carlos R, Romanach MJ. Clinical pathological conference case 6: infantile myofibroma. Head Neck Pathol. 2011;5:292-5.
20. Brierley DJ, Khurram SA, Speight PM. Solitary myofibroma of the adult mandible: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;27:012.
21. Haspel AC, Coviello VF, Stevens M, Robinson PG. Myofibroma of the mandible in an infant: case report, review of the literature, and discussion. J Oral Maxillofac Surg. 2012;70:1599-604.
22. Jordan RCK, Regezi JA. Oral spindle cell neoplasms: a review of 307 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:717-24.
 Correspondence:
Correspondence:
Roger Corrêa de Barros Berthold
Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS)
Faculdade de Odontologia, Prédio 6
Av. Ipiranga, 6681, CEP 90616-900
Porto Alegre, RS, Brasil
e-mail: rogerberthold@hotmail.com













