Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.21 no.41 Canoas Jul./Dez. 2015
Clinical management of crown-root fracture due to occlusal interference
Dentes natais e neonatais: relato de três casos
André Azevedo dos Santos I; Ana Paula Perroni II; Josué Martos III; Noéli Boscato IV
I DDS (private practice), Pelotas, RS, Brazil
II MSc candidate at the Graduate Program in Dentistry (Prosthodontics), School of Dentistry, Universidade Federal de Pelotas (UFPel), Pelotas, RS, Brazil
III DDS, MSc, and PhD; and is associate professor at the School of Dentistry, UFPel, Pelotas, RS, Brazil
IV DDS, MSc, and PhD; and is adjunct professor at the Graduate Program in Dentistry, School of Dentistry (Prosthodontics), UFPel, Pelotas, RS, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript
ABSTRACT
This clinical report describes a crown-root fracture of the upper right central incisor associated with compromised anterior dental aesthetics. Occlusal adjustment and aesthetic rehabilitation were achieved by using single-tooth restorations with IPS e.max Press®. The precepts of occlusion were observed to establish an optimal occlusion in terms of static and dynamic mandibular movement. Five-year follow-up demonstrated that the clinical protocol used was successful, providing periodontal tissues with no signs of disease. Satisfactory function has been observed associated with excellent aesthetic outcomes. Reestablishing the occlusal pattern provided longevity to the aesthetic treatment, as well as health to the stomatognathic system.
Keywords: Dental Occlusion; Dental Prosthesis; Tooth Fractures.
RESUMO
Este relato de caso descreve uma fratura coronorradicular do incisivo central superior direito associado com insatisfatória aparência estética anterior. Foram feitos ajustes oclusais e reabilitação estética com restaurações unitárias usando o sistema IPS e.max Press®. Os preceitos da oclusão foram observados a fim de estabelecer uma oclusão ideal nos movimentos mandibulares estáticos e dinâmicos. Cinco anos de acompanhamento demonstraram que o protocolo clínico usado foi bem-sucedido, favorecendo a manutenção da saúde dos tecidos periodontais. Observou-se satisfatória função associada com excelente estética. O restabelecimento do padrão oclusal favoreceu a longevidade do tratamento estético e a saúde do sistema estomatognático.
Palavras-chave: Oclusão Dentária; Prótese Dentária; Fraturas dos Dentes.
INTRODUCTION
Several procedures must be understood and mastered in order to achieve effective aesthetic and prosthetic rehabilitation. Among them, a thorough knowledge of occlusion, its interference, and maneuvers for adjustment are crucial. Clinical manifestations, as periodontal ligament thickening, mobility, wear facets, fremitus, pain, and tooth darkening and fracture characterize specific clinical signs of occlusal trauma due to premature contacts during mandibular movement 1. Eliminating the adverse influence of proprioceptive inputs from occlusal interference and/or trauma is mandatory 2.
Functional aspects play a significant role regarding oral rehabilitation, thus problems can result in structural and biological damage 3. Adequate anterior guidance is essential, because it provides optimal management of load transfer and low threshold of periodontal afferents around the canine and incisor teeth 4,5. However, aesthetic aspects do play a major role in patient satisfaction. For producing highly aesthetic procedures, several ceramic materials are available 6,7. Among them, the ceramic system based on lithium disilicate provides suitable aesthetic outcomes and resistance 8.
This clinical report describes the treatment of a patient showing unsatisfactory maxillary anterior aesthetics, with darkening and complicated crown-root fracture in the maxillary right central incisor derived from occlusal trauma in protrusive and lateral movement.
CASE REPORT
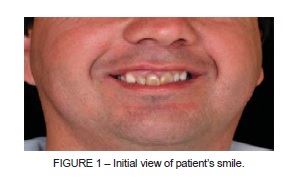
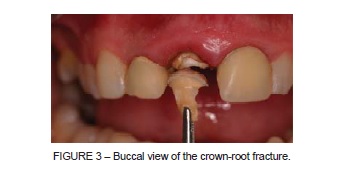
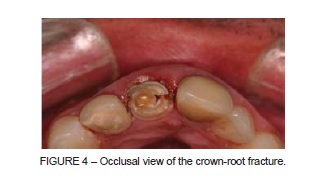
A 37-year-old male patient sought dental care complaining he was unhappy about the aesthetics of his smile (Figure 1). Intraoral clinical examination revealed unsatisfactory maxillary anterior aesthetics due to darkening of the maxillary right and left central incisors and lateral right incisor. Periodontal examination in the right maxillary central incisor evidenced gingival inflammation and occlusal interference (Figure 2), in addition to a crown-root fracture (Figures 3 and 4), stemming from ineffective protrusive movement. Radiographic examination of maxillary anterior teeth revealed satisfactory endodontic treatment, although right and left central incisors showed inappropriate posts, characteristically short in length and diameter. Considering the local and systemic factors, such as the patient's general health status, local risk factors, status of the remaining teeth, as well as their periodontal support and bone health, the treatment plan included periodontal treatment associated with prosthetic treatment by using tooth-single metal-free crowns and suitable occlusal adjustment.

Occlusion was analyzed again, along with diagnostic casts mounted on a semiadjustable articulator. This evaluation confirmed the notable discrepancy between dental arches. Maxillary and mandibular casts were obtained, mounted on a semiadjustable articulator, and occlusion was assessed again, preoperatively. Analysis of the anteroposterior relation between dental arches confirmed notable posterior occlusal disharmony and orthodontic treatment needs. However, such a treatment was an infeasible alternative in this particular case, due to aspects related to patient's work. Then, an appropriate occlusal pattern by diagnostic wax-up was initially established, which constitutes a valuable tool for any smile makeover, because it provides information for occlusion contacts, optimal crown form and template for temporary restorations 9. In this process, the desired amount of tooth structure is removed from the preoperative model and the adequate anterior and lateral guidance are waxed on the original teeth of casts. The diagnostic wax-up also produced a mock-up for preparing the definitive prosthetic crowns.
According to the treatment plan, metallic posts were removed from the maxillary right and left central incisors and maxillary right lateral incisor, and they subsequently received a glass-fiber post (White post DC®; FGM, São Paulo, SP, Brazil), 1.5 mm in diameter and luted with self-adhesive resin cement (RelyXU100®; 3MESPE, St. Paul, MN, USA). The core restorations were made of microhybrid composite resin (Filtek Supreme®; 3M ESPE, St. Paul, MN, USA). Following, teeth were prepared with diamond burs (KG Sorensen®, Barueri, SP, Brazil) and chamfer finish line was performed. Maxillary right lateral incisor received higher reduction in the buccal dental surface, due to its inadequate tooth position. Cervical preparation was extended until the cementumenamel junction and smooth margins were created to prevent stress concentration zones. Prefabricated artificial acrylic resin teeth (Trilux®; RuthiBras, São Paulo, SP, Brazil) and self-cured acrylic resin were used to confection of temporary restorations, according to the criteria of form, function, and aesthetics. Full-arch impressions of maxillary abutment teeth were made, by using regular-body polysulfide (Permlastic®; Kerr, Orange, CA, USA). An opposing arch impression was also performed, by using irreversible hydrocolloid impression material (Jeltrate Plus®; Dentsply, York, PA, USA). Both impressions were poured in type III dentalstone (Microstone®; Whip Mix Corp, Louisville, KY, USA) and stone casts were mounted on a semi-adjustable articulator (A7Fix®; Bioart, São Carlos, SP, Brazil) at maximum intercuspation position, and they were sent to laboratory for manufacturing of the ceramic substructures. On the maxillary cast, metal-free ceramic substructures were waxed-up and obtained by using lithium disilicate-reinforced glass ceramic material (IPS e.max press®; Ivoclar Vivadent, Schaan, Liechtenstein). After verifying the adaptation of copings, veneer porcelain (IPS e.max Ceram®; Ivoclar Vivadent) was applied and fired to achieve the definitive dental shape. Then, phonetic aesthetic and functional evaluation were carefully carried out. Ceramic was glazed and the crowns luted by using dual-cured self-adhesive resin cement (RelyXU100®; 3MESPE, St. Paul, MN, USA), following manufacturer's instructions. Excess luting cement was removed and the marginal area was properly finished, then polished with abrasive discs and strips. Occlusion analysis of static and dynamic movement was carefully performed, to avoid any occlusal interference (Figure 5). Satisfactory occlusal pattern and absence of any occlusal interference were observed at each patient's recall appointments. After a 5-year follow-up, the patient was satisfied with his rehabilitation at the aesthetic and functional levels (Figure 6).


DISCUSSION
Occlusal interference has been defined in the literature over the years as interference with closure, habitual and/or terminal hinge, and excursive interference with non-working or working sides 10,11. These kinds of interference in protrusive and canine guidance lead to induction of abnormal activity in masticatory muscles, mandibular displacement, and occlusal overload 10-14. Therefore, multidisciplinary knowledge and occlusal adjustment are required to provide longevity to the rehabilitation treatment 10,15. It is noteworthy that severity of dental and periodontal diseases is determined through intensity and duration of the action exerted by occlusal trauma or by their continuing interference 9,13.
Functional analysis must be the starting point to perform any restorative treatment 3 and it may be clinically useful for evaluation and diagnosis of periodontal and dental diseases 9. Non-working side interference must be always removed, because it leads to the most detrimental effects, although occlusal interference in maximum intercuspation has also a deleterious effect on periodontal and pulpal tissues of the affected tooth 9. Static occlusion must be observed to examine the existence of any deflective contact between the cusps of opposing teeth. Dynamic occlusion must be performed to assess interference on mandibular movements 9. Indeed, the relationship between periodontal attachment, bone loss, and occlusal trauma may also provide significant information regarding the origin of occlusal trauma, periodontal diseases, and tooth fracture 16.
This clinical report described the treatment of a patient with both aesthetic and functional dental concerns. Considering the anteroposterior relation between dental arches, other options available were discussed with the patient, including orthodontic treatment; he chose to address only anterior aesthetic and functional problems. The aesthetic problem was completely overcome through the lithium disilicate glass-ceramic system, which has shown to be capable of restoring dental form and function with great color match and high accuracy of adjustment, translucency, and opacity 8. The occlusal trauma was removed and adequate anterior and lateral guidance were resumed by providing the patient with functional satisfaction after a 5-year follow-up.
FINAL REMARKS
It may be claimed that reestablishing the occlusal pattern provided longevity to the aesthetic treatment, as well as health to the stomatognathic system.
REFERENCES
1. Popescu MR, Deva V, Dragomir LP, Searpe M, Vatu M, Stefarta A, et al. Study on the histopathological modifications of the dental pulp in occlusal trauma. Rom J Morphol Embryol. 2011;52:425-30. [ Links ]
2. Reis A, Loguercio AD. Tooth fragment reattachment: current treatment concepts. Pract Proced Aesthet Dent. 2004;16:739-40.
3. Nagarsekar A, Aras M. Role of anterior guidance in esthetic and functional rehabilitation. J Indian Prosthodont Soc. 2008;8:225-7.
4. Sapkota B, Gupta A. Pattern of occlusal contacts in lateral excursions (canine protection or group function). Kathmandu Univ Med J. 2014;12:43-7.
5. Klineberg IJ, Trulsson M, Murray GM. Occlusion on implants – is there a problem? J Oral Rehabil. 2012;39:522-37.
6. Bynum JH. Clinical case report: Testing occlusal management, previewing anterior esthetics, and staging rehabilitation with direct composite and Kois deprogrammer. Compend Contin Educ Dent. 2010;31:298-302.
7. Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glassceramic crowns: a retrospective study. Quintessence Int. 2002;33:503-10.
8. Vivadent I. IPS e.max® Press – Instructions for use. Schaan/Liechtenstein: Ivoclar Vivadent AG; 2009.
9. Davies SJ, Gray RM, Whitehead SA. Good occlusal practice in advanced restorative dentistry. Br Dent J. 2001;191:421-4.
10. Clark GT, Tsukiyama Y, Baba K, Watanabe T. Sixty-eight years of experimental occlusal interference studies: what have we learned? J Prosthet Dent. 1999;82:704-13.
11. Kawakami M, Okamoto K, Fujii R, Kirita T. Orthodontic rehabilitation for anterior teeth lost due to trauma with crowding malocclusion. Dent Traumatol. 2010;26:357-9.
12. Burgett FG. Trauma from occlusion – periodontal concerns. Dent Clin North Am. 1995;39:301-11.
13. Alani A, Patel M. Clinical issues in occlusion – Part I. Singapore Dent J. 2014;35C:31-8.
14. De Boever JA, Carlsson GE, Klineberg IJ. Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part II: Tooth loss and prosthodontic treatment. J Oral Rehabil. 2000;27:647-59.
15. da Cunha LF, Pedroche LO, Gonzaga CC, Furuse AY. Esthetic, occlusal, and periodontal rehabilitation of anterior teeth with minimum thickness porcelain laminate veneers. J Prosthet Dent. 2014;112:1315-8.
16. Ishigaki S, Kurozumi T, Morishige E, Yatani H. Occlusal interference during mastication can cause pathological tooth mobility. J Periodontal Res. 2006;41:189-92.
 Correspondence:
Correspondence:
Noéli Boscato
Graduate Program in Dentistry
School of Dentistry, UFPel
Rua Gonçalves Chaves, 457, 2º andar
CEP 96015-560, Pelotas, RS, Brazil
e-mail: noeliboscato@gmail.com













