Stomatos
ISSN 1519-4442
Stomatos vol.22 no.42 Canoas ene./jun. 2016
Evaluation of retentive force of attachment systems for overdentures retained by one or two implants
Avaliação da força de retenção de sistemas de encaixe para overdentures retidas por um ou dois implantes
Paulo Roberto Mattia I; Daniela M. Botega II; Sabrina Rebollo Zani III; Elken G. Rivaldo III; Luis Carlos F. Frasca II
I professor, School of Dentistry, Universidade de Caxias do Sul (UCS), Caxias do Sul, RS, Brazil
II professors, School of Dentistry, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil
III professors, School of Dentistry, Universidade Luterana do Brasil (ULBRA), Canoas, RS, Brazil
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
Objective: Single implant-retained overdentures are an appealing option for rehabilitation, but the retentive force of attachments in this setting has yet to be determined. Methods: Three attachment systems (ERA, O-Ring, and Ball Attachment), using components made from different materials (plastic and metal), were tested under two different support conditions (single-implant or two-implant). Under irrigation, the systems were subjected to a series of simulated insertion-removal cycles. Maximal retention values were obtained before testing and after 3,240 cycles on a universal testing machine (cross-head speed of 0.5 mm/min). Student's t-test for independent samples was used for statistical analysis (P < 0.05). Results: Tensile strength of the O-Ring and Ball Attachment systems did not show significant changes after mechanical cycling (with one or two implants), while the ERA system showed significant reductions at cycles 2,160 and 3,240 (in the single-implant and in the twoimplant specimens) as compared with the other cycles. Conclusion: Single-implant support for mandibular overdentures can be an alternative for the oral rehabilitation of fully edentulous patients, providing greater simplicity, lower costs, and similar retentive strength as compared to two-implant overdentures, improving the user's quality of life. The tested systems meet the retentive needs of removable prosthodontic appliances, regardless of the number of supporting implants.
Keywords: Dental Implants; Complete Denture; Overdenture; Single Implant.
RESUMO
Objetivo: Overdentures retidas por um único implante são uma opção reabilitadora, entretanto a força de retenção dos encaixes nessa condição ainda não foi estabelecida. Métodos: Três sistemas de encaixe (ERA, O-Ring e Ball Attachment), que utilizam diferentes materiais para retenção (plástico e metal), foram testados sob diferentes condições de suporte para uma overdenture (implante único ou dois implantes). Os sistemas de encaixe foram submetidos a um ensaio simulando ciclos de inserção-remoção da prótese. Valores máximos de retenção foram obtidos antes e após a realização de 3.240 ciclos, em uma máquina de ensaios universal, com velocidade de 0,5 mm/min. Os resultados foram submetidos ao teste t de Student para amostras independentes (P < 0.05). Resultados: Os valores de força de retenção dos encaixes O-Ring e Ball Attachment não apresentaram diferença estatística após ciclagem mecânica (com 1 ou 2 implantes), enquanto que o sistema ERA apresentou redução significativa nos ciclos 2.160 e 3.240 (com 1 e 2 dois implantes) quando comparado aos demais ciclos. Conclusões: Overdentures mandibulares retidas por implante único podem ser uma alternativa para a reabilitação de pacientes edêntulos, proporcionando maior simplicidade, menor custo e retenção semelhante às overdentures retidas por 2 implantes, com consequente melhora na qualidade de vida. Os sistemas de encaixe avaliados apresentaram a retenção necessária para overdentures, independentemente do número de implantes.
Palavras-chave: Implantes Dentários; Prótese Total; Sobredentadura; Implante Único.
INTRODUCTION
The use of osseointegrated implants to support dental prostheses has proven efficacy1. Implant-retained mandibular overdentures improve quality of life for edentulous patients, obtained by greater retention of complete dentures2.
Compared to implant-supported fixed complete dentures, overdentures provide advantages that include lower treatment cost, possibility of removal for care and cleaning, and, in specific cases, clearer speaking, in addition to factors that contraindicate placement of a greater number of implants, such as severe bone resorption, mandibular atrophy, and poor bone quality3.
Currently, the standard implant-based treatment recommended for edentulous patients involves placement of two implants into the alveolar bone in the anterior region of the mandible4. Several studies have evaluated the retentive force of these systems, whether isolated or using bar-and-clip systems5, all-plastic attachments6, both plastic and metal components3, and among different attachment systems 7,8, and have demonstrated their efficiency.
With advances in this predictable treatment modality, some authors have suggested that similar outcomes can be obtained using only one implant placed in the anterior region of the mandible9-11. Walton et al.12 conducted a clinical assessment of the performance of mandibular overdentures retained by a single midline implant in terms of patient satisfaction, component costs, and maintenance sessions for 1 year after placement, as compared with conventional treatment. According to the authors, a single-implant solution for overdenture retention and stabilization was as satisfactory as two implants, requiring the same maintenance but with reduced operative time and cost. In another clinical study, Cordioli et al.13 reported improvement in comfort and masticatory function in 21 patients treated with the single-implant approach.
This is an affordable and relatively simple treatment option, with the advantage that implant parallelism is less of a concern14. Therefore, it is a promising restorative treatment modality, and is relevant from a social standpoint for rehabilitation of lowincome patients15,16. It is known that attachments must have a retentive force of at least 5 N to keep prosthetics in place during function17. However, daily use, the oral environment, and parafunctional activities may affect the retentive capacity of attachments.
Within this context, the present in vitro study sought to compare the resistive force and fatigue resistance of three attachment systems in single-implant and two-implant conditions. The null hypothesis was that there would be no differences among the three attachment systems in the two simulated conditions.
MATERIAL AND METHODS
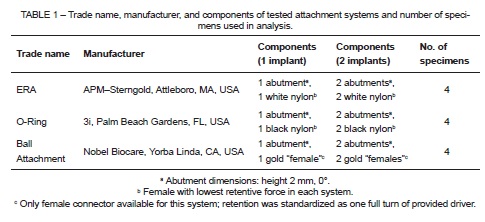
Three types of overdenture attachments were selected: ERA (APM – Sterngold, Attleboro, MA, USA); O-Ring (3i, Palm Beach Gardens, FL, USA); and Ball Attachment (NobelBiocare, Yorba Linda, CA, USA). Four specimens of each system were fabricated, in two conditions (two-implant and single-implant), as shown in Table 1.
Two cylinders (height 20 mm, diameter 35 mm) were made from autopolymer acrylic resin (Orto Clas – Artigos Odontológicos Clássico Ltda., São Paulo, SP, Brazil). Two implants (ICE, 3i, Palm Beach Gardens, FL, USA) were embedded into one cylinder, 22 mm apart (5). A single implant was embedded into the other cylinder (Figure 1).
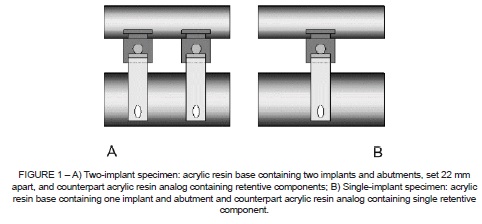
Briefly, the components necessary for single-implant and two-implant retention – a pair of components from each system for two-implant analogs and a single component from each system for the single-implant analogs – were installed onto the resin cylinders and assayed on a universal testing machine.
The least retentive abutment of each system was selected: namely, the white component of the ERA system, the black component of the O-Ring system, and the gold component (the only one available) of the Ball Attachment system. Retention of the gold component of the Ball Attachment was standardized by activation (one full turn) using the tool provided.
The corresponding retention components of each system were embedded in another autopolymer acrylic resin analog (height 2 cm, diameter 3.5 cm), made to simulate the base of a complete denture (Figure 1). During testing, insertion-removal motions were performed along the implant axis in standardized fashion.
The mechanical cycling test was performed on a VERSAT 502M universal testing machine (Panambra Industrial e Técnica S.A., São Paulo, SP, Brazil), with an HBM S40/50kg load cell (HBM Inc., Darmstadt, Germany). The attachment systems were subjected to 3,240 insertion-removal cycles, to simulate 3 years of use (removal three times daily for cleaning). The motor speed was set at 32 rpm and the test performed under constant irrigation with artificial saliva (Salivan, Aspen Farmacêutica S/A, São Paulo, SP, Brazil).
The retentive force of the attachment was measured before the start of mechanical cycling (0 cycles) and after 3,240 cycles (36 months). Maximum force was reached at the time of separation between the abutment and retainer of the attachment system, at a crosshead speed of 0.5 mm/min.
Student's t-test for independent samples was used for statistical analyses. The significance level to reject the null hypothesis was set at P < 0.05. For each attachment system, we compared percent retention loss in the conventional (two-implant) overdenture model and in the single-implant model.
RESULTS
As shown in Table 2, mechanical cycling did not cause significant changes in the tensile strength of the O-Ring and Ball Attachment systems, whether with one or two implants. With the ERA system, significant reductions in tensile strength occurred at cycles 2,160 and 3,240, both in the single-implant and in the two-implant specimens, as compared with the values measured during other cycles.
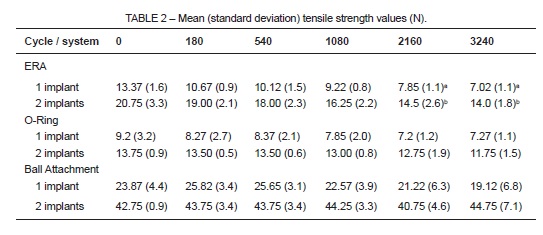
Lowercase letters in rows (ERA system) represent statistically significant differences in relation to other cycles.
Analysis of the results showed that the percent mean reduction of retentive force with the ERA system was 47.4% for single-implant specimens and 31.8% for two-implant specimens. The O-Ring system exhibited reductions of 17.1% and 17.6% respectively under the same conditions. The Ball Attachment system exhibited an 18.2% reduction in single-implant specimens and, unlike the other systems, a 4.5% increase in retentive force in the two-implant specimens.
No component fractures occurred during testing.
DISCUSSION
The null hypothesis that there would be no statistically significant differences among the tested attachment systems under the two study conditions was rejected. The ERA attachment system exhibited significantly lower retentive force after simulation of 3 years' usage. Conversely, the O-Ring and Ball Attachment exhibited no significant differences in retentive force after 3,240 cycles.
In addition to exhibiting a decrease in retentive force after mechanical cycling, the ERA attachment system also showed the highest rate of decline in retention of its components. Similar results were reported by Gamborena et al.18, who found an 85% reduction in the retentive force of the components of this system. According to the authors, this may have occurred due to permanent deformation of the plastic components, as shown under microscopic analysis. In the present study, the greater reduction observed in single-implant specimens may be attributable to greater load.
In all systems, the retentive force values obtained after mechanical cycling exceeded the minimum level required to keep an overdenture in place, which is 5 N17. Bearing this in mind, the ERA system may be deemed appropriate for use (whether supported by one or two implants) as long as the patient does not require particularly strong retention7.
According to several studies, all attachment systems exhibit some wear or deformation after a certain number of cycles and when under functional loading, which may be due to friction between the retaining abutment and its counterpart19. Similar findings were reported by Epstein et al.20.
With the O-Ring system, single-implant and two-implant specimens exhibited the same reduction in retentive force, which was less than that observed with the ERA system, although the difference was not significant. The O-Ring system uses a rubber O-ring, which passes over the largest diameter of the retaining abutment and is then trapped below it, to retain the denture. As this component is highly flexible, it exhibits massive elastic deformation and no plastic deformation, which leads to a lesser decrease in retentive force21.
Finally, in the Ball Attachment group, there was a decrease in retentive force for single-implant specimens and a minor increase in retentive force for two-implant specimens, with no significant difference. The other tested systems had metal abutments and plastic retentive components, whereas the Ball Attachment system has all-metal components. Therefore, during the mechanical cycling test, these components were subjected to repetitive strain, causing permanent deformation. This concept of fatigue may explain the increase in retentive force values (in two-implant specimens) followed by a reduction in these values (in single-implant specimens), with no significant differences3.
Clinical studies have shown that single-implant support for mandibular overdentures can be an alternative for oral rehabilitation of fully edentulous patients, with consequent improvement in user quality of life16. Cordioli et al.22, found insignificant marginal bone loss, improved comfort and oral function, and no treatment failures over a 5-year observation period; treatment was comparable to overdentures supported by two implants.
Krennmair et al.23 found that single-implant anchorage led to significant improvement in subjective patient satisfaction and to a reduction in commonly reported symptoms. Patients with single-implant-retained overdentures found evidence of improved quality of life and masticatory function.
Liddelow & Henry24 studied the use of single implant-supported overdentures for rehabilitation of elderly patients with poor retention and phonetic problems, and found a significant increase in patient satisfaction levels.
The number of cycles used in the present study (3,240) simulated 3 years of usage. Other studies have employed varied cycle counts, including 10,000 cycles19, 5,500 cycles5,18, and 3,000 cycles25.
Prefabricated attachments for implant-supported overdentures exhibit major variation in retentive force values7. Furthermore, the wide range of commercially available brands and models and the broad variability in study methods preclude direct comparison with other investigations. Therefore, further studies are required, as the oral milieu, composition of saliva, temperature, parafunctional habits, and angulation of abutments are all factors that may infl uence outcomes. Evidently, the conditions under which this study was conducted are distinct from clinical practice, which constitutes a limitation. Nevertheless, our results are valid and significant.
CONCLUSION
Within the limitations of the present study, we conclude there were no significant differences in percent wear among the different overdenture groups, whether supported by a single implant or by two implants. All systems met the basic retention needs of overdentures, whether supported by a single implant or by two implants.
REFERENCES
1. Kronstrom M, Davis B, Loney R, Gerrow J, Hollender L. A prospective randomized study on the immediate loading of mandibular overdentures supported by one or two implants: a 12-month follow-up report. Int J Oral Maxillofac Implants. 2010;25:181-8. [ Links ]
2. Fromentin O, Lassauzay C, Abi Nader S, Feine J, de Albuquerque Junior RF. Testing the retention of attachments for implant overdentures – validation of an original force measurement system. J Oral Rehabil. 2010;37:54-62.
3. Pigozzo MN, Mesquita MF, Henriques GE, Vaz LG. The service life of implant-retained overdenture attachment systems. J Prosthet Dent. 2009;102:74-80.
4. Wolf K, Ludwig K, Hartfil H, Kern M. Analysis of retention and wear of ball attachments. Quintessence Int. 2009;40:405-12.
5. Botega DM, Mesquita MF, Henriques GE, Vaz LG. Retention force and fatigue strength of overdenture attachment systems. J Oral Rehabil. 2004;31:884-9.
6. Evtimovska E, Masri R, Driscoll CF, Romberg E. The change in retentive values of locator attachments and hader clips over time. J Prosthodont. 2009;18:479-83.
7. Chung KH, Chung CY, Cagna DR, Cronin RJ Jr. Retention characteristics of attachment systems for implant overdentures. J Prosthodont. 2004;13:221-6.
8. Williams BH, Ochiai KT, Hojo S, Nishimura R, Caputo AA. Retention of maxillary implant overdenture bars of different designs. J Prosthet Dent. 2001;86:603-7.
9. Ismail HA, Mahrous AI, Banasr FH, Soliman TA, Baraka Y. Two years retrospective evaluation of overdenture retained by symphyseal single implant using two types of attachments. J Int Oral Health. 2015;7:4-8.
10. Passia N, Wolfart S, Kern M. Six-year clinical outcome of single implant-retained mandibular overdentures – a pilot study. Clin Oral Impl Res. 2015;26:1191-4.
11. Bryant SR, Walton JN, MacEntee MI. A 5-year ramdomized trial to compare 1 or 2 implants for implant overdentures. J Dent Res. 2015;94:36-43.
12. Walton JN, Glick N, Macentee MI. A randomized clinical trial comparing patient satisfaction and prosthetic outcomes with mandibular overdentures retained by one or two implants. Int J Prosthodont. 2009;22:331-9.
13. Cordioli G, Castagna S, Consolati E. Single-tooth implant rehabilitation: a retrospective study of 67 implants. Int J Prosthodont. 1994;7:525-31.
14. Alsabeeha N, Payne AG, De Silva RK, Swain MV. Mandibular single-implant overdentures: a review with surgical and prosthodontic perspectives of a novel approach. Clin Oral Impl Res. 2009;20:356-65.
15. Grageda E, Rieck B. Metal-reinforced single implant mandibular overdenture retained by an attachment: a clinical report. J Prosthet Dent. 2014;111:16-9.
16. Srinivasan M, Makarov NA, Herrmann FR, Müller F. Implant survival in 1-versus 2-implant mandibular overdentures: a systematic review and meta-analysis. Clin Oral Impl Res. 2016;27:63-72.
17. Lehmann KM, Armin FV. Studies on the retention forces of snap-on attachments. Quintessence Dent Technol. 1978;7:45-8.
18. Gamborena JI, Hazelton LR, NaBadalung D, Brudvik J. Retention of ERA direct overdenture attachments before and after fatigue loading. Int J Prosthodont. 1997;10:123-30.
19. Wichmann MG, Kuntze W. Wear behavior of precision attachments. Int J Prosthodont. 1999;12:409-14.
20. Epstein DD, Epstein PL, Cohen BI, Pagnillo MK. Comparison of the retentive properties of six prefabricated post overdenture attachment systems. J Prosthet Dent. 1999;82:579-84.
21. Bonachela WC, Pedreira AP, Marins L, Pereira T. Comparative evaluation of retention loss in four types of attachments used on overdentures in function of time of use. J Appl Oral Sci. 2003;11:49-54.
22. Cordioli G, Majzoub Z, Castagna S. Mandibular overdentures anchored to single implants: a five-year prospective study. J Prosthet Dent. 1997;78:159-65.
23. Krennmair G, Ulm C. The symphyseal single-tooth implant for anchorage of a mandibular complete denture in geriatric patients: a clinical report. Int J Oral Maxillofac Implants. 2001;16:98-104.
24. Liddelow G, Henry P. The immediately loaded single implant-retained mandibular overdenture: a 36-month prospective study. Int J Prosthodont. 2010;23:13-21.
25. Nagaoka E, Nagayasu Y, Yamashita H, Matsushiro H, Okuno Y. Study of retention in attachments for overdenture. (II) O-ring attachment. J Osaka Univ Dent Sch. 1980;20:215-26.
 Correspondence:
Correspondence:
Daniela Maffei Botega
Rua Ramiro Barcelos, 2492
CEP 90035-003, Porto Alegre
RS, Brazil
E-mail: danimaffei@yahoo.com













