Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Stomatos
versão impressa ISSN 1519-4442
Stomatos vol.22 no.43 Canoas Jul./Dez. 2016
Absence of interdental papilla – Systematic review of available therapeutic modalities
Ausência de papila interdental – revisão sistemática sobre as modalidades terapêuticas disponíveis
Maria Augusta Matas Hennig I; Jamile Marconato Mustafa II; Marta Liliana Musskopf III
I Dentist, Master's student in the Graduate Program in Dentistry, ULBRA, Canoas
II Dentist, ULBRA Canoas
IIIDentist, Doctor, Adjunct Professor in the Undergraduate and Graduate Program in Dentistry, ULBRA Canoas
The authors have no conflicts of interest to declare concerning the publication of this manuscript.
ABSTRACT
The objective of the present study was to conduct a systematic review of the treatment alternatives for the absence of interdental papilla (AIP), a clinical situation that can have aesthetic and phonetic impacts. A search for original articles, in humans, reporting more than one case, without language restrictions, dealing with therapeutic alternatives for AIP, was conducted in the databases of MEDLINE and EMBASE. The strategy included [("interdental papilla" OR "black triangles" OR "open gingival embrasure") AND ("treatment" OR "therapy" OR "reconstruction")] up to the year of 2010, resulting in seven studies being included. One study was found upon checking the reference lists and was added, bringing the total to 8 studies. The sample size ranged from two to 19 participants. Six of the eight studies used periodontal surgical techniques and five associated the subepithelial connective tissue graft. Two studies treated AIP with reticulated hyaluronic acid gel. The follow-up time ranged from four to 24 months. The results, in relation to the interdental space area, ranged from 43% to 100% of filling and the reduction of the distance between the contact point and the tip of the papilla ranged from 0.73 to 2.8 mm. Two studies did not describe the results numerically. It was concluded that the therapeutic results presented by the authors were positive. However, it is necessary to take into consideration that the designs of the studies included here have a weak capacity for generating scientific evidence. As studies with a randomized clinical trial design are not conducted to respond to this clinical question, the results of the present study should be used with caution.
Keywords: Systematic review; Interdental papilla; Therapy; Periodontics.
RESUMO
O objetivo deste estudo foi realizar uma revisão sistemática sobre as alternativas de tratamento da ausência da papila interdental (API), situação clínica que pode trazer impactos estéticos e fonéticos. Uma busca por artigos originais, em humanos, apresentando mais de 1 caso, sem restrição de idiomas, que tratassem sobre alternativas terapêuticas para a API foi realizada nas bases de dados Pubmed e Embase. A estratégia incluiu: [("interdental papilla" OR "black triangles" OR "open gingival embrasure") AND ("treatment" OR "therapy" OR "reconstruction")] a partir do ano de 2010, resultando em sete estudos incluídos. Um estudo foi encontrado na verificação das listas de referências e adicionado, totalizando 8 estudos. O tamanho amostral variou de dois a 19 participantes. Seis dos oito estudos utilizaram técnicas cirúrgicas periodontais e cinco associaram o enxerto conjuntivo subepitelial. Dois estudos trataram a API com gel de ácido hialurônico reticulado. O tempo de acompanhamento variou de quatro a 24 meses. Os resultados em relação ao espaço/área interdental variaram de 43 a 100% de preenchimento e a redução da distância entre o ponto de contato e a ponta da papila variou de 0,73 a 2,8 mm. Dois estudos não descreveram numericamente os resultados. Conclui-se que os resultados terapêuticos apresentados pelos autores foram positivos. Entretanto, é preciso levar em consideração que o delineamento dos estudos incluídos tem fraca capacidade de gerar evidência científica. Enquanto estudos com delineamento do tipo ensaio clínico randomizado não sejam realizados para responder essa pergunta clínica, os resultados do presente estudo devem ser utilizados com cautela.
Palavras-chave: Revisão Sistemática; Papila Interdentária; Terapia; Periodontia.
INTRODUCTION
The absence of the interdental papilla, generating black triangles, is a large concern for dentists and for patients. It favors the impaction of food, the occurrence of phonetic problems and can cause great aesthetic damage when it occurs in the anterior region, even when changes of only 2 mm occur1,2. The etiology of the loss of the interdental papilla is multifactorial, and may or may not be associated with effects of periodontal diseases. Many factors may influence the absence of interdental papilla, including aging, loss of alveolar bone height in relation to interproximal contact, angulation of the root, triangular crowns, change to the papilla during orthodontic alignment and traumatic oral hygiene procedures3. Filling the interdental space may require a multidisciplinary approach involving orthodontic, periodontal and restorative treatment. Therapy of the black triangles may be performed using non-surgical, surgical and restorative prosthetic methods3. Regarding the surgical methods, mainly Miller's Class I and II vestibular gingival recessions, the literature supports predictability of the root coverage4. However, in Miller's Class III (which involves the loss of interproximal bone tissue), partial coverage of the recession occurs; while, in cases of Miller's Class IV, there is no predictability of root coverage, although it can occasionally be achieved4.
Apparently, there is no consensus, in the literature, on clinical recommendations as to how to proceed in treating cases of the absence of the interdental papilla. That being the case, the objective of the present study was to gather data from a systematic search of the literature about current treatment alternatives of situations involving the absence of the interdental papilla. This may help the clinician in making therapeutic decisions. The present study is described according to the recommendations of PRISMA5.
METHODS
Eligibility criteria
The scientific articles included dealt with therapeutic alternatives for the absence of the interdental papilla, were original studies, in humans, were not case reports, had no language restrictions, setting the year 2010 as the lower limit for publication.
Among the studies that met the criteria for eligibility, those that were not related to the subject of the present review or that deal with treating the absence of papilla between implants were excluded.
Information sources and search
A systematic search in the databases of MEDLINE and EMBASE was conducted to locate scientific articles that dealt with therapeutic alternatives for the absence of the interdental papilla. The search strategy included [("interdental papilla" OR "black triangles" OR "open gingival embrasure") AND ("treatment" OR "therapy" OR "reconstruction")]. Further, the bibliographic references of the selected studies were evaluated to identify possible studies, not previously located using the steps mentioned above. The database searches were conducted until April 7th, 2016.
Study selection
The selection was conducted in two phases. Phase 1 involved analysis of titles and abstracts of all studies that resulted from the search strategy. Phase 2 involved reading the complete texts of the studies selected in Phase 1. Two readers (MAMH and MLM) participated independently in both phases. Differences between the two were discussed until consensus was reached. It is important to stress that, in the two phases, the readers were blind as to the authorship and origin of the study.
Data items
The following information was collected from all the studies included: author(s), year and country of publication, sample size, classification of the type of defect, treatment (technique used for closing the interdental space), follow-up time and results.
Quality of the reports from the studies
Two reviewers (MAMH and MLM) evaluated all the studies included according to the version of the CARE checklist6.
Summary measures
The results were evaluated in relation to the interdental space area, with the percentage of filling and the reduction of the distance between the contact point and the tip of the papilla in millimeters. The initial evaluation and the final evaluation (greater follow-up time shown in the studies) were compared.
RESULTS
Study selection
The search strategy resulted in a total of 493 articles. Through the analysis of the titles, 452 were excluded. After exclusion by title, the 41 remaining articles were evaluated by the abstract using the same criteria, and 34 were excluded. The 7 remaining articles were read in full text. One study was found by checking the reference list and was included. The fl owchart of the selection of the studies is shown in a Figure 1.
Study characteristics
The eight studies selected were published between the years 2010 and 2015. They were conducted in different countries: one in Brazil7, four in India8-11, one in Argentina12, one in Iran13 and one in Saudi Arabia14. All studies were published in English. The sample sizes of the articles ranged from two7,12 to 199 participants, and from two12 to 399 sites. Six7-12 of the eight studies included presented treatment alternatives for the absence of interdental papilla through surgical techniques. The follow-up time ranged from four7 to 2412 months. All studies report both objective and subjective, positive results. Data from the eight studies included in the systematic review are described in Table 1.
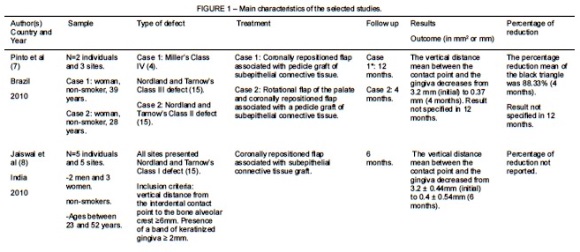
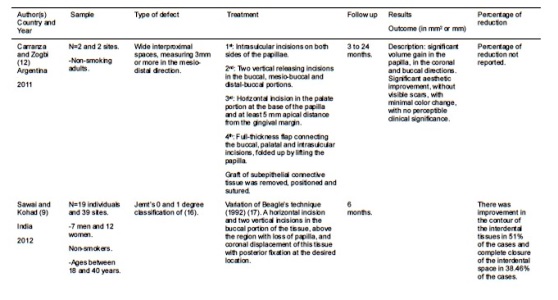
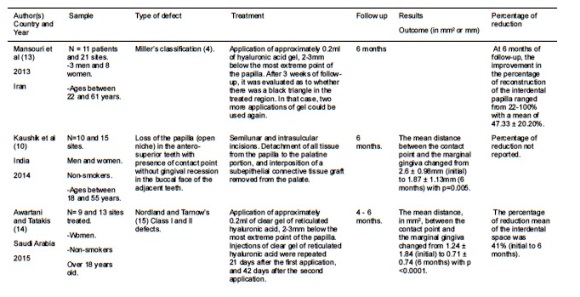
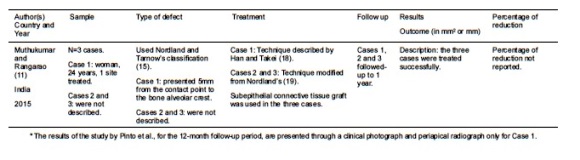
Quality of the reports from the studies
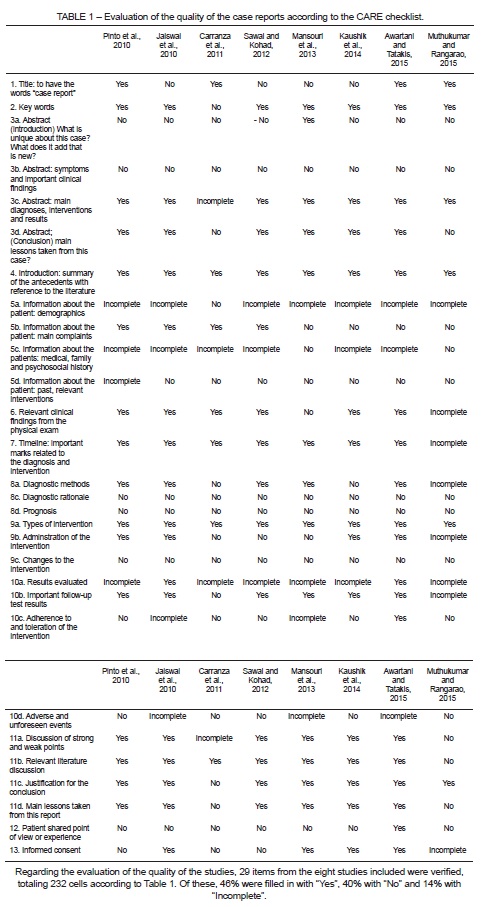
The results of the evaluation of the quality of the reports of the studies included are summarized in Table 1. Only item 8b was excluded, as it was not applicable to the studies selected.
DISCUSSION
Summary of evidence
The present systematic review of the literature sought to gather information regarding therapeutic alternatives for the treatment of interdental papilla loss. The search strategy used returned seven studies7-12,14 on the topic, published in English, from the year 2010 until April of 2016. These studies came from the databases MEDLINE and EMBASE and one study was included after checking the reference lists.
Among the articles selected, six7-9,11,13,14 used classification systems that identify the type of defect. The most used classification (four of five studies) was the description by Nordland and Tarnow15, one study used the Jemt's16 classification and another used Miller's classification4. The other studies10,12 described the types of defects. These data shows that there is no consensus as how to evaluate this type of defect and how to determine which criteria should be taken into consideration at the time of classification.
Regarding the main outcome evaluated, the reduction of interdental space, among the therapeutic modalities, six studies 7-12 used periodontal surgical techniques. Five of them 7,8,10-12 associated the use of subepithelial connective tissue graft to various surgical techniques. Only two studies13,14 treated the interdental papilla loss with the application of hyaluronic acid gel. All studies reported positive results in regard to filling the interdental space. Two studies did not describe the results numerically11,12. From this, it is possible to observe that no study presented a "gold standard" technique for the interdental papilla augmentation.
Although the search strategy was not designed to limit the types of therapeutic modalities, it only showed studies that propose filling the interdental space by increasing the size of the interdental papilla. However, some studies found in the literature, mainly case reports, present multidisciplinary treatment alternatives for this clinical situation20. Restorative dentistry, prostheses and orthodontics may, either exclusively or more commonly, together with the therapeutic modalities found in the studies selected in the present review, be part of the treatment of the absence of interdental papilla20,21.
Limitations
Regarding the protocol of the present systematic review, one limitation may be the data estalished for the return of studies. The choice was made to evaluate more recently published studies, since 2010. In addition to gathering only current studies, the limit of 2010 was set because, in 2009, a systematic review with a meta-analysis had been published on a similar subject22. To our knowledge, this is the first systematic review to approach the issue of the absence of interdental papilla specifically, and not root coverage in general.
The main limitation found, in relation to the studies returned, concerns the design thereof. Among the eight studies included, from the information presented by the authors, two of them7,12 may be classified as case reports and three8,11,14 as case series. The methodologies of the other three studies9,10,13 don't have clear designs and may be considered case series or even uncontrolled clinical studies, according to Fogarty and Wardle23. Therefore, the evidence is weak24. Regarding the evaluation of the quality of the studies, more than half of the items evaluated according to the CARE Checklist were present, even if some of them were incomplete. Nevertheless, conducting the evaluation relevant to the type of design of the studies, one may consider that they are of good quality. 29 items from the eight studies included were verified, totaling the 232 cells in Table 1. Of these, 46% were filled with "Yes", 40% "No" and 14% "Incomplete". The lack of studies with pertinent methodology for the comparison of therapeutic alternatives, of the type of randomized clinical trial, is a concern. For example, without any calculation of the estimate of the sample size, definition of a gold standard therapy, randomization of individuals for different types of treatment and blinding of examiners, the use of the results of the studies returned should be used with caution for making a professional decision.
CONCLUSION
The present systematic review of the literature returned eight studies7-14 on the therapeutic treatment modalities for the absence of the interdental papilla. Of the eight studies selected, six7-12 showed different surgical techniques and, of these, five 7,8,10-12 made use of subepithelial connective tissue graft. Two studies13,14 used hyaluronic acid. The therapeutic results presented by the authors, related to filling the interdental space, were positive. However, it is necessary to consider that the design of the studies included generates weak scientific evidence to support making a clinical decision. While studies with a more appropriate design, such as randomized clinical trials, are not conducted to answer this specific clinical question, the results of the present study should be used with caution.
REFERENCES
1. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol [Internet]. 1992;63(12):995–6. Available from: www.joponline.org doi abs 10.1902 jop.1992.63.12.995\npapers3: publication doi 10.1902 jop.1992.63.12.995
2. Kokich VO, Kiaki HA SP. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;1(6):311–24.
3. Sharma AA, Park JH. Esthetic considerations in interdental papilla: Remediation and regeneration. J Esthet Restor Dent. 2010;22(1):18–28.
4. Miller P. A Classification of Marginal Tissue Recession. Int J Periodontcs Restor Dentislry. 1985;5(2):8–13.
5. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2009;339(august):332–6.
6. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. The CARE guidelines: Consensus-based clinical case report guideline development. J Clin Epidemiol. 2014; 67(1):46–51.
7. Pinto RCNC CB, Ishikiriama SK, Chambrone L, Pustiglioni EF RG. The subepithelial connective tissue pedicle graft combined with the coronally advanced fl ap for restoring missing papilla: a report of two cases. Quintessence Int (Berl) [Internet]. 2010;41(3):213– 20. Available from: www.ncbi.nlm.nih.gov pubmed 20213022
8. Jaiswal P, Bhongade M, Tiwari I, Chavan R, Banode P. Surgical reconstruction of interdental papilla using subepithelial connective tissue graft (SCTG) with a coronally advanced fl ap: A clinical evaluation of five cases. J Contemp Dent Pract. 2010;11(6):49–57.
9. Sawai ML, Kohad RM. An evaluation of a periodontal plastic surgical procedure for the reconstruction of interdental papillae in maxillary anterior region: A clinical study. J Indian Soc Periodontol [Internet]. 2012;16(4):533–8. Available from: www.pubmedcentral. nih.gov articlerender.fcgi?artid=3590722&tool=pmcentrez&rendertype=abstract
10. Kaushik A. Clinical Evaluation of Papilla Reconstruction Using Subepithelial Connective Tissue Graft. J Clin Diagnostic Res [Internet]. 2014;8(9):77–81. Available from: jcdr.net article_fulltext.asp?issn=0973-709x&year=2014&volume=8&issue =9&page=ZC77&issn=0973-709x&id=4881
11. Muthukumar S, Rangarao S. Surgical augmentation of interdental papilla - A case series. Contemp Clin Dent. 2015;6(1):294–9.
12. Carranza N, Zogbi C. Reconstruction of the interdental papilla with an underlying subepithelial connective tissue graft: technical considerations and case reports. Int J Periodontics Restorative Dent [Internet]. 2011;31(5):e45-50. Available from: www. ncbi.nlm.nih.gov pubmed 21845236
13. Mansouri SS, Ghasemi M, Salmani Z, Shams N. Clinical Application of Hyaluronic Acid Gel for Reconstruction of Interdental Papilla at the Esthetic zone. 2013;208–14.
14. Awartani FA, Tatakis DN. Interdental papilla loss: treatment by hyaluronic acid gel injection: a case series. Clin Oral Investig [Internet]. 2015;2–7. Available from: www.ncbi.nlm.nih.gov pubmed 26613740 44.
15. Nordland WP, Tarnow and DP. A Classification System for Loss of Papillary Height. J Periodontol. 1998;69(10):1124–6.
16. Jemt T. Regeneration of gingival papillae after single-implant. Int J Periodontics Restor Dent. 1997;17(4):9497723.
17. JR B. Surgical reconstruction of the interdental papilla: case. Int J Periodontics Restor Dent. 1992;12(2):1521996.
18. Han TJ, Takei HH. Progress in gingival papilla reconstruction. Periodontol 2000 [Internet]. 1996;11:65–8. Available from: www.ncbi.nlm.nih.gov pubmed 9567958
19. Nordland WP, Sandhu HS PC. Microsurgical technique for augmentation of the interdental papilla: three case reports. Int J Periodontics Restor Dent. 2008;28(6):19146049.
20. Follak AC, Ilha BD, Ribeiro DS, Mielke JC, David SCD DL. Reanatomização e fechamento de triângulo negro em dentes ânterossuperiores. Rev Dentística line. 2012;23:26–32.
21. Kovalik AC, Pilatti GL, Academy A. Papila Interdental: Previsibilidade Das Técnicas. Brazil J Periodontol. 2011;21(3):22–32.
22. Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root Coverage Procedures for the Treatment of Localized Recessio-Type Defects: A Cochrane Systematic Review. J Periodontol [Internet]. 2010;81(4):452–78. Available from: www.ncbi.nlm.nih.gov pubmed 20367089
23. Fogarty S, Wardle J. Advances in Integrative Medicine Integrative medicine case series: A clinician's guide to publication. Adv Integr Med [Internet]. 2016;1–5. Available from: dx.doi.org 10.1016 j.aimed.2015.11.001
24. Forrest JL, Miller S a. Enhancing your practice through evidence-based decision making: Finding the best clinical evidence. J Evid Based Dent Pract [Internet]. 2001;1(3):227–36. Available from: www.sciencedirect.com science article B75B8- 4HDXWTM-10 2 40511e0519b3c3b8a88c680436a0769f.
 Correspondence:
Correspondence:
Marta Liliana Musskopf
Avenida Farroupilha número 8001
Canoas/RS
E-mail: martalmusskopf@gmail.com













