Services on Demand
Article
Related links
Share
Brazilian Journal of Oral Sciences
On-line version ISSN 1677-3225
Braz. J. Oral Sci. vol.10 n.2 Piracicaba Apr./Jun. 2011
ORIGINAL ARTICLE
Antimicrobial activity of chlorhexidine in patients with fixed orthodontic appliances
Nakas EnitaI; Vildana DzemidzicI; Alisa TiroI; Enes PasicII; Sanja HadzicII
I DDS, Msc, Senior research assistant, Department of Orthodontics, School of Dentistry, University of Sarajevo, Sarajevo, Bosnia and Herzegovina
II DDS, Msc, Senior research assistant, Department of Oral medicine and Periodontology, School of Dentistry, University of Sarajevo, Sarajevo, Bosnia and Herzegovina
ABSTRACT
Aim: Oral environment of orthodontic patients undergoes changes, such as pH reduction, larger number of sites available for Streptococcus mutans collection, and increased accumulation of food particles, which may lead to an increased number of S. mutans colony-forming units (CFU) in saliva. Chlorhexidine gluconate (CHX) is the most potent documented antimicrobial agent against Mutans streptococci and dental caries. The aim of this work was to assess efficiency of CHX-based mouthwashes in patient with fixed orthodontic appliances. Methods: Twenty patients with fixed appliances were selected for this study. They were undergoing full-bonded non extraction treatment with metal brackets (Roth 0.22, Discovery Dentaurum) on their teeth and bands on their molars. Each patient was provided with a toothbrush and toothpaste. The mouthwashes were used by patients according to the manufacturers' directions 15 min after toothbrushing: 5 mL of 0.2% CHX (Corsodyl, GlaxoSmithKline) was applied for 60 s in the morning and before bedtime for 2 weeks. Results: The data were analyzed according to the nonparametric Wilcoxon signed rank test (SPSS software). Statistical significance level was set at p<0.05. Conclusions: The use of CHX-based mouthwashes in patients with fixed orthodontic appliances led to reduction in the level of S. mutans.
Keywords: chlorhexidine, Streptococcus mutans, orthodontic treatment.
Introduction
Bonded orthodontic appliances increase the number of plaque retention sites, reduce the possibility self-cleaning on vestibular areas and impede oral hygiene. As of result of this, the oral cavity of orthodontic patients undergoes changes, such as pH reduction, larger number of sites available for Streptococcus mutans collection, and increased accumulation of food particles, which may lead to an increased number of S. mutans colony-forming units (CFU) in saliva1.
Dental plaque is a multi-species biofilm consisting of more than 700 species of oral bacteria on tooth surfaces, and mutans streptococci (MS) are the major group of early primary colonizers2. MS are microorganisms that primarily colonize dental surfaces. At concentrations of 104-105 CFU/mL in saliva, S. mutans is able to colonize clean, smooth surfaces of teeth. The presence of MS on tooth surfaces increases the possibility of caries development3. Due to some of their vital characteristics, MS are regarded potentially highly cariogenic4. Therefore, preventive efforts in these risk groups have concentrated on direct suppression of the cariogenic microflora by chemotherapeutics as an adjunct to improved oral hygiene.
Chlorhexidine gluconate (CHX) is the most potent documented antimicrobial agent against MS and dental caries5. Mouth rinsing with a chemical agent could be a useful clinical adjunct for reducing the bacterial plaque accumulation during the active phase of orthodontic treatment. Chemical agents also help orthodontic patients who have difficulties in maintaining plaque control by mechanical means alone. The aim of this work was to assess efficiency of CHX-based mouthwashes in patients with fixed orthodontic appliances.
Material and methods
Twenty patients with fixed appliances were selected for this study. The following criteria were used for selecting patients who were undergoing full-banded non extraction treatment with metal brackets (Roth 0.22, Dentaurum GmbH & Co., Ispringen, Germany) on their teeth and bands on their molars who: were at least 13 and no more than 18 years old with complete permanent dentition including second molars; had no evidence of decalcification on their teeth; had no active caries lesion; had no known medical problem or current antibiotic therapy; had anterior composite fillings; had no known hypersensitivity to CHX.
Each patient was provided with a toothbrush, a toothpaste and a leaflet with brushing instructions; All patients were instructed to brush for a minimum of 3 min.
The same protocol was followed for each patient. First, the gingiva of individual teeth was examined and scoring was performed, according to the following scoring system: 0: Normal gingiva; 1: Slight inflammation - a minor change in color, consistency (no bleeding on probing); 2: Average inflammation - redness, swelling (bleeding on probing); 3: Severe inflammation - strong redness and swelling (spontaneous bleeding). Final score was obtained when the total score was divided by the number of examined teeth.
After collection of stimulated saliva sample for the purpose of establishing the quantities of S. mutans and Lactobacillus spp. . Saliva samples were collected at two timelines for each patient: 1. Before use of CHX (at least 1 month after bonding); 2. After 2 weeks of use of CHX. For such purpose, colony counting test kit (CRT Bacteria, Ivoclar Vivadent, Liechtenstein) was used, according to manufacturer's instruction. Patients were given a piece of (factory-made) wax, which they chewed for 5 min in order to collect enough stimulated saliva. While chewing, they collected saliva into disposable sterile plastic cups.
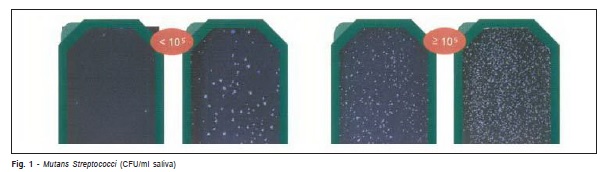
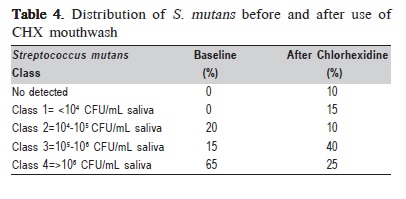
After 5 min, disposable pipettes were used to take saliva and seed it on slides for Streptococci mutans and Lactobacilli spp. The protective coat from sterile slides was removed, 5 drops were neatly dripped on the slide (until its entire surface was covered in saliva), which was held under a slight angle, taking special care not to damage the surface of the slide with the sharp edge of pipette. Once the procedure was over, a tablet of NaHCO3 was put in slide boxes, and then the boxes were closed and placed into an incubator at 37°C. Forty-eight hours later, the results were read as indicated in the manufacturer's scheme, according to the following scale: Class 1= <104 CFU/mL saliva; Class 2=104-105 CFU/mL saliva; Class 3=105-106 CFU/mL saliva; Class 4=>106 CFU/mL saliva (Figure 1.)
The mouthwashes were used by patients according to the manufacturer's directions 15 min after toothbrushing: 5 mL of 0.2% CHX (Corsodyl, GlaxoSmithKline) was applied for 60 s in the morning and at bedtime for 2 weeks. The patients were instructed not to consume any liquid or food or at least 30 min after using the prescribed mouthwash. All patients are asked to bring the mouthwash bottle, so we could determine patient compliance based on how much liquid was left.
The data were analyzed using the nonparametric Wilcoxon signed rank test (SPSS software, SPSS Inc., Chicago, IL, USA). Statistical significance level was set at p <0.05
Results
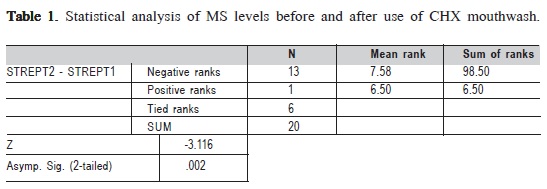
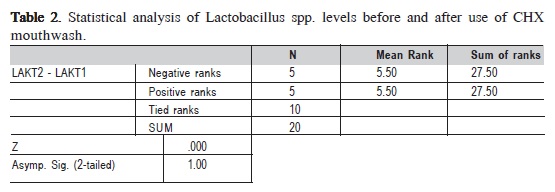
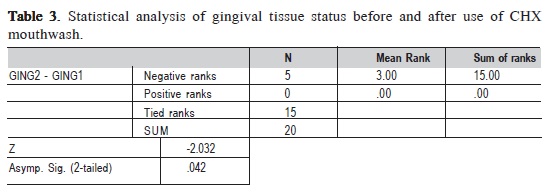
The results of the statistical analysis of MS levels, Lactobacillus spp. levels and gingival tissue status before and after use of CHX mouthwash are presented in Tables 1, 2 and 3. The distribution of S. mutans before and after use of CHX mouthwash is given in Table 4.
The findings of the present study indicate that the use of CHX mouthwashes reduced S. mutans levels (p = 0.002) in patients with fixed orthodontic appliances. Thirteen patients presented lower S. mutans while in 6 patients S. mutans counts remained the same regardless of use of the antimicrobial agent.
CHX-based mouthwash had no significant impact on Lactobacillus spp. levels, as 5 patients presented higher counts, 5 presented lower counts while in 10 patients Lactobacillus spp. counts remained the same regardless of use of the antimicrobial agent.
Discussion
The findings of the present study regarding the effect of the CHX mouthwash on the microbial counts are in accordance with those of other authors. Oltramari-Navaro et al. (2009)6 suggested that the use of dentifrices with lower CHX concentration can reduce the risk of tooth staining without compromising its effectiveness in controlling gingivitis and bleeding in orthodontic patients. Masek et al. (2008)7 found that Cervitec® caused a reduction of S. mutans and Lactobacillus spp. saliva counts in patients with previously identified high level of these bacteria. Sari (2007)8 reported that 0.2% CHX mouthwash decreased S. mutans levels, but had no effect on lactobacilli levels. Olympio et al. (2006)9 observed that the use of dentifrices containing CHX seems to be effective for the treatment of gingivitis in orthodontic patients. Beyth (2003)10 found a significant reduction of S. mutans CFU in 10 patients after use of CHX oral rinse10. According to Eldridge (1998)11, the use of CHX mouthwash reduces the levels of S. mutans, gingival index and gingival bleeding. Anderson (1997)12 found that the use of CHX oral rinse contributes to improving oral hygiene in patients with fixed orthodontic appliances12.
In the present study, 6 patients reported discoloration of teeth as a result of the treatment, which is a possible side effect o CHX. Eldridge (1998)11 described the appearance of brown color tongue that spontaneously resolved after cessation of the use of CHX, which, however, was not observed in the present study. Anderson (1997)12 observed discoloration of teeth and increase in dental calculus formation, but they did not determine the significance of these phenomena.
Our results corroborate previous findings about the influence of CHX on S. Mutans levels, oral hygiene and gingival condition13-14. In the present study, the use of CHX-based mouthwashes reduced S. mutans counts and improved the gingival index, but had no significant impact on Lactobacillus counts.
References
1. Mota SM, Enoki C, Ito IY, Elias AM, Matsumoto MA. Streptococcus mutans counts in plaque adjacent to orthodontic brackets bonded with resin-modified glass ionomer cement or resin-based composite. Braz Oral Res. 2008; 22: 55-60. [ Links ]
2. Yanti, Rukayadi Y, Lee KH, Hwang JK. Activity of panduratin A isolated from Kaempferia pandurata Roxb. against multi-species oral biofilms in vitro. J Oral Sci. 2009; 51: 87-95.
3. Nakas E, Zukanovic A.The prevalence of cariogenic salivary microorganisms in children of various ages. Bosn J Basic Med Sci. 2007; 7: 166-70.
4. Gibbons RJ, Cohen L, Hay DI. Strains of Streptococcus mutans and Streptococcus sobrinus attach to different pellicle receptors. Infect Immun. 1986; 52: 555-61.
5. Attin R, Ilse A, Werner C, Wiegand A, Attin T. Antimicrobial effectiveness of a highly concentrated chlorhexidine varnish treatment in teenagers with fixed orthodontic appliances. Angle Orthod. 2006; 76: 1022-7.
6. Oltramari-Navarro PV, Titarelli JM, Marsicano JA, Henriques JF, Janson G, Lauris JR et al. Effectiveness of 0.50% and 0.75% chlorhexidine dentifrices in orthodontic patients: a double-blind and randomized controlled trial.. Am J Orthod Dentofacial Orthop. 2009; 136: 651-6.
7. I. Mašek, D. Matoševic, H.Juric, S.Meštrovic Antimicrobial effects of chlorhexidine in orthodontic patients ascro. Acta Stomatol Croat. 2008; 42: 41-8.
8. Sari E, Birinci I. Microbiological evaluation of 0.2% chlorhexidine gluconate mouth rinse in orthodontic patients. Angle Orthod. 2007; 77: 881-4.
9. Olympio KP, Bardal PA, de M Bastos JR, Buzalaf MA Effectiveness of a chlorhexidine dentifrice in orthodontic patients: a randomized-controlled trial. J Clin Periodontol. 2006; 33: 421-6.
10. Beyth N, Redlich M, Harari D, Friedman M, Steinberg D. Effect of sustained-release chlorhexidin digluconate varnish on Streptococcus mutans and Actinomyces viscosus in orthodontic patients.; Am J Orthod Dentofacial Orthop. 2003; 123: 345-8.
11. Eldridge KR, Finnie SF, Stephens JA, Mauad AM, Munoz CA, Kettering JD. Efficacy of an alcohol-free chlorhexidin digluconate mouthrinse as an antimicrobial agent. J Prosthet Dent. 1998; 80: 685-90.
12. Anderson GB, Bowden J, Morrison EC, Caffesse RG.: Clinical effects of chlorhexidin digluconate mouthwashes on patients undergoing orthodontic treatment.; Am J Orthod Dentofacial Orthop. 1997;111: 606-12.
13. Schaeken MJ, van der Hoeven JS, Hendriks JC. Effects of varnishes containing chlorhexidine on the human dental plaque ûora. J Dent Res. 1989; 68: 1786-9.
14. Lundstrom F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients: the effect of chlorhexidine treatments. Eur J Orthod. 1987; 9:109-16.
 Correspondence:
Correspondence:
Nakas Enita
Department of Orthodontics,
School of Dentistry, University of Sarajevo
Bolnièka 4a , 71 000 Sarajevo,
Bosnia and Herzegovina
E-mail: enitta@gmail.com
Received for publication: January 01, 2011
Accepted: April 19, 2011