Brazilian Journal of Oral Sciences
ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.1 Piracicaba ene./mar. 2012
ORIGINAL ARTICLE
Social and demographic profile of Unified Health System users in a medium-sized city of southern Brazil
Simone Gomes Dias de OliveiraI; Pedro Henrique Azambuja CarvalhoII; Rafael Guerra LundIII
IDDS, MSc student in Prosthodontics, School of Dentistry, Federal University of Pelotas, Brazil
IIUndergraduate student, School of Dentistry, Federal University of Pelotas, Brazil
IIIDDS, MSc, PhD in Dentistry, School of Dentistry, Federal University of Pelotas, Brazil
ABSTRACT
AIM: The use of health services is a complex behavior and results from a series of determinants that includes the users' social and demographic characteristics. The current survey interprets the social and demographic profile of Unified Health System (UHS; SUS in Portuguese) users from Pelotas RS Brazil, which was conducted by interviews with 333 users from five Health Basic Units (HBUs).
METHODS: The social and demographic characterization was deployed by the variables sex, age, occupation, city/town or district of origin, number of family members, use of continuous medication, diseases and family income.
RESULTS: HBU users were mostly women (82.4%), within the 30-40-year-old age range (21.4%), housewives (36.3%) from Pelotas (96.2%) and from the district of Fragata (26.1%). Families of users comprise mostly two to four members (66.6%), with an income of one to two minimum wages (66.2%). Fifty-one percent of the interviewees do not use continuous medication, while hypertension was the most cited disease (51.8%).
CONCLUSIONS: An understanding of HBU users' characteristics and their associated social and demographic context may contribute towards a better reception and may confirm the UHS contribution towards universality and equality of public health care.
Keywords: Unified Health System, health profile, social conditions, Brazil.
Introduction
Wealth distribution in Brazil is still highly uneven not only among the federal states, but also among the population. The Unified Health System (UHS - SUS in Portuguese) represents a health program of the Brazilian government notorious for its general principles of organization which covers medical expenses of about 80% of the Brazilian population1. The UHS guarantees access to any health service to all the population and warrants citizen participation through their representative entities in the process of health public polices and their execution2. Moreover, the health services should have a macroeconomic (cost control) and microeconomic (maximization of services, with maximum satisfaction at minimum costs) efficiency3.
Users' satisfaction and the use of health services are a complex behavior resulting from a set of determinants, which include the users' socio-demographic characteristics. In fact, health practices do not have merely a technical dimension;they are, at the same time, complex social practices permeated by culture, economy, politics and ideological dimensions². These multiple aspects interact mutually, compete for a set of actions and services availability, as well as compete for emergence of issues to gain access to activities and services4.
The health service organization in Brazil comprises the Unified Health System (UHS), which is public and governmental, featuring a universal and equitable orientation, and a complementary system, which is private, made up of health insurance and care through payment. According to data by the World Health Search and National Research by Domiciliary Sample5, the private system in Brazil covers about 34.5% of the population, whereas the public health system covers 100% of the Brazilian population. Moreover, UHS differs from the health systems of other countries in that it is comprises all citizens in Brazil and promotes equal and equitable orientation6.
The Brazilian public health system warrants to all citizens the same rights and promotes total universal access to all free offered services. Further, the equity principle guarantees more access to the most needy and thus health democratization is provided7.
Since its implementation, UHS administrators have been adapting its institutional model through social participation guidelines and through decentralization triggered by the activities of the Brazilian state in deploying in-depth modifications in the social field6. However, changes have not reduced inequality and inequities in the Brazilian public health system are still disparate8.
Health care humanization should be analyzed by focusing on professionals and users. The more integrated the UHS assistance, the greater guarantee of a quality and equitable health services. However, this process depends on a critical view by users and professionals9.
So that a constant dialogue with the movements may be kept and permanent and sustainable ways of articulation established, the system's vulnerability must be reduced and the population's life quality increased. Such relationship multiplies the possibilities of solving health problems, which enhance UHS activities10.
According to Buss and Pellegrini Filho (2008)8, the determining factor in a country's general health situation is not total wealth but its distribution. In Brazil, besides notoriously serious inequities, large sectors of the population live in poor conditions which, in the main, impair their access to minimum health conditions.
Population surveys on life and health conditions have been undertaken periodically in a large number of countries to organize public policies and their attributions. Colombia, for instance, is conducting several population surveys aimed at building a database for monitoring and assessing public health policies under implementation11.
The current survey interprets the socio-demographic profile of the UHS users from the city of Pelotas-RS, at the southern region of Brazil.
Material and methods
The study was approved by the Ethics Committee of the School of Dentistry of the Federal University of Pelotas (RS, Brazil) (No. 083/2009).
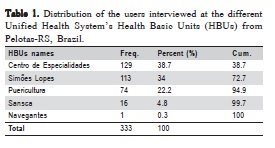
This descriptive cross-sectional survey of a convenience sample comprised 333 users of five Health Basic Units (HBUs) from the city of Pelotas, southern Brazil (Table 1). Semistructured interviews with open and closed questions were carried out for the survey. The socio-demographic profile of UHS users was determined by data collection during a 1- year period and all users selected for the study freely accepted to participate in the interviews.
Pelotas is a medium-sized city (323,034 inhabitants, with 22,082 residents in rural areas) in a relatively affluent area in southern Brazil. Its economy is based on services and food industries (Department of Economic Development, 2002). The HBUs were chosen according to their importance, care diversity and location in the city in such a way that a more diversified population could be covered and the study range expanded.
The interviews were carried out by two students from the School of Dentistry of the Federal University of Pelotas, who were properly instructed within a pilot study. The only requirement for the users to be included in the sample was being treated at the HBUs. If they accepted the invitation, the participants were interviewed randomly while waiting for treatment, after signing an informed consent form.
All eligible UHS users agreed to participate in the survey. After the interviews, data collected were tabulated in software SPSS 10.0 and analyzed by STATA SE 10. So that the socio-demographic characterization of the sample population could be analyzed the following variables were taken: sex, age, occupation, city/town or district of origin, number of family members, continuous medication use, diseases with extended treatment, and family income per capita.
Results
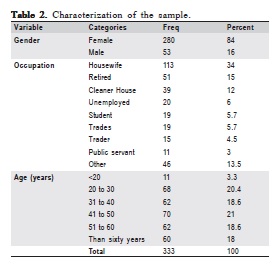
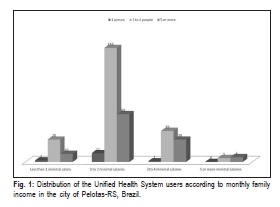
The results for gender, age and occupation of users are shown in Table 2. The professional profile characterized most users as housewives (33.93%) and pensioners (15.3%) with monthly 1-2 minimum wages (64.26%) (Figure 1). The number of persons per household was between 2 and 4 people (64.56%).
Data reveal that users from 33 districts of Pelotas andhome users make use of the five selected UHS. Most of them were from the neighboring district of Fragata (26.6%), and 2.7% were residents in neighboring towns (Capão do Leão, Canguçu, Piratini, Turuçu and Cerrito).
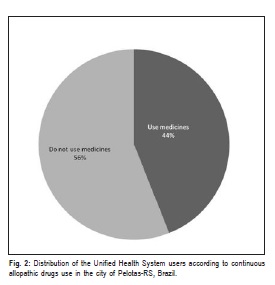
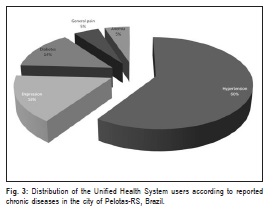
A considerable portion of the sample reported to use allopathic medicines (43.84%) (Figure 2). Hypertension was reported by the UHS users as the most common chronic disease (46.58%) (Figure 3).
Discussion
UHS users interviewed were mostly female (84.08%), but it is important to mention that one of the HBUs chosen for this study was a Children's Clinic. According to Ribeiro et al.6, women are more concerned with health and are traditionally responsible for the care to children and other sick family members. This fact explains the discrepant percentage when compared to the number of males in current study. Owing to such characterization, high investments must be made so that women have healthier lives. Medical doctors should be trained to treat this female public by clear communication and in places where they feel comfortable. Comprehensive health facilities with more flexible hours are also of great importance12.
Moreover, the difference in dealing with men's health provokes serious reflections. Most conventional health indicators show that a gap exists between the sexes and their access to health services. A higher male mortality exists at almost every age and for almost all causes. Moreover, life expectancy at birth and in other age ranges is always lower among men. In addition, various diseases affect men more. It is an issue that must be considered when dealing with family health and, by extension, a healthy community. In fact, in general, there are health programs that include children, adolescents, women and the elderly; there are none, however, with the exception of programs for workers' health, whichspecifically target the adult male13.
The income level and age structure of the population should be taken into account to organize the provision of health services and health expenditures for each country according to its model of medical assistance14. In examining the age group which demands services at the UHS, some authors have observed a high prevalence of the elderly and relate this fact to the aging population. About 70% of the elderly in the World Health Search and National Research by Domiciliary Sample (PNAD-2003) reported having at least one chronic illness condition. Moreover, the proportion of people with health problems increases according to age in both sexes. Thus the elderly population is a great user of health services. In developed countries, the use of these services among people aged 65 years and over is three to four times greater than its proportional size in the population15. In the present study, increased service offer for the elderly was not reported since the elderly population comprised only 18% of the sample. A broader age group in the population sampled was within the 41-50-year-old age range (21.02%), followed by the 20-30-year-old age range (20.42%).
The features such as women and low income in this study are consistent with other studies that portray the reality of the users of the UHS. Ribeiro et al.6 have also characterized individuals as women (2:1) with low schooling level (52.8% with up to 3 years of study) and a concentration on the first four quintiles of family income with an excess of individuals in the first two quintiles.
Several studies indicate that the individual's position in the social structure is an important indicator of health needs, and the pattern of perceived risk tends to be disadvantageous for those individuals belonging to the underprivileged social groups16. In a 2008 study carried out in the city of Pelotas, the authors concluded that the socioeconomic status influenced the use and the type of health service, with difficulties in accessing health care17.
A marked change occurs when the structure of service consumption among income groups was analyzed: high income groups consume more outpatient services and consumption of hospital services tends to increase as the income rises. Moreover, a change occurs in the type of outpatient service used: the higher income groups use predominantly private practices and clinics, whereas the smaller income groups use more clinics and health centers11.
Such events go contrary to the third principle of the Unified Health System, which says that every citizen has the right to humane care that is friendly and free from any discrimination. This principle refers to the universal nature of the UHS as a health system for all Brazilians, which has yet to happen; this proves, in practice, discrimination and restricted access9.
A considerable portion of the studied population claimed to use allopathic medicines regularly. The cost of drugs has a similar pattern with regard to spending money on health care, which means that the poorest people (who have more morbidity and therefore have greater need to consume drugs) tend to spend less on this item. Restricting the use of drugs among people with low purchasing power becomes evident when one notes that the weight of that spent on household income is proportionally greater than for those with higher income11.
Arterial hypertension was the most common pathology, which indicates a prevalence of chronic diseases, with an increasing rate in recent decades, and the prevalence of cardiovascular conditions18. A study by the National Research per Residence Sample revealed similar results for the disease that most affects UHS users. The authors reported that the disease most often cited by study participants was hypertension (43.9%), and the proportion decreased with age in both sexes15.
It is very difficult to generalize the results of a convenience sample to any population that has practical relevance. However, convenience sampling provides useful information for other studies involving probability sampling techniques. Despite limitations, the present study suggests that the data collected from this convenience sample can represent the socio-demographic profile of UHS users and is an appropriate sampling strategy to provide national population data that will inform and contribute towards the current and future public health policies in Brazil.
Some aspects of the UHS are highly successful. A social basis exists so that the reform may continue; in fact, thousands of workers and millions of Brazilians recognize the importance of the UHS. However, impairments exist with regard to both the users and the system19,20.
The results obtained in the present survey reveal that understanding the characteristics of HBU users and the associated socio-demographic context may contribute to a better health care for citizens and confirm the UHS contribution towards the universality and the equity of public health care.
Acknowledgements
This project was partially funded by an undergraduate grant provided by the National Council for Scientific and Technological Development (CNPq), Brazil.
References
1. Castilla EE, Luquetti DV. Brazil: Public Health Genomics. Public Health Genomics 2009;12:53-8. [ Links ]
2. Oliveira DC, Sá CP, Gomes AMT, Ramos RS, Pereira NA, Santos WCR. Brazilian National Health Policy: health professionals' social representation. Cad Saude Publica. 2008;24:197-206. [ Links ]
3. Cesconetto A, Lapa JS, Calvo MCM. Evaluation of productive efûciency in the Uniûed National Health System hospitals in the State of Santa Catarina, Brazil. Cad Saude Publica. 2008;20:2407-17. [ Links ]
4. Moretti-Pires RO. Complexity in the Family Health and education of future health professionals. Interface (Botucatu). 2009;13:153-66. [ Links ]
5. Brazilian Institute of Geography and Statistics (IBGE). National Survey by Household Sample Survey: Access and use of health services in 2003. Rio de Janeiro: IBGE; 2005. [ Links ]6. Ribeiro MCSA, Barata RB, Almeida MF, Silva ZP. Sociodemographic profile and utilization patterns of the public health care system (SUS)– PNAD 2003. Cien Saude Colet. 2006;11:1011-22.
7. Silva ZP, Ribeiro MCSA, Barata RB, Almeida MF. Sociodemographic profile and utilization pattern of health services of the Unified Health System (SUS). Cien Saude Colet. 2011;16:3807-16. [ Links ]
8. Buss PM, Pellegrini Filho A. Inequalities in health in Brazil, our most serious disease: comments on the reference document and the work of the National Commission on Social Determinants of Health. Cad Saude Publica. 2006;22:2005-8. [ Links ]
9. Backes DS, Koerich MS, Rodrigues ACRL, Drago LC, Klock P, Erdmann AL. What do the users think and say about the Brazilian Health System (SUS)? An analysis of meanings based on the users' rights booklet. Cien Saude Colet. 2009;14:903-10. [ Links ]
10. Horta NC, Sena RR, Silva MEO, Oliveira SR, Rezende VA. Practice of family health teams: challenges for the promotion of health care. Rev Bras Enferm. 2009;62:524-9. [ Links ]
11. Travassos C, Viacava F, Fernandes C, Almeida CM. Social and geographical inequalities in health services utilization in Brazil. Cien Saude Colet. 2000;5:133-49. [ Links ]
12. Torres MEA, Ribeiro PM, Machado CJ. Access to gynecological consultations in Belo Horizonte, Minas Gerais, Brazil. Rev Bras Estud Popul. 2008;25:49-69. [ Links ]
13. Schraiber LB, Figueiredo WS, Gomes R, Couto MT, Pinheiro TF, Machin R et al. Health needs and masculinities: primary health care services for me. Cad Saude Publica. 2010;26:961-70. [ Links ]
14. Guanais FC. Health equity in Brazil. BMJ. 2010;341:c6542. [ Links ]
15. Lima-Costa MF, Barreto SM, Giatti L. Health status, physical functioning, health services utilization, and expenditures on medicines among Brazilian elderly: a descriptive study using data from the National Household Survey. Cad Saude Publica. 2003;19:735-43. [ Links ]
16. Evans RG, Barer ML, Marmor TR. Why are some people healthy and others not?: the determinants of health of populations. Nova York: Aldine De Gruyter; c1994. p.3-26. [ Links ]
17. Dias-da-Costa JS, Gigante DP, Horta BL, Barros FC, Victora CG. Pattern of health services utilization by adults of the Pelotas birth cohort from 1982 to 2004-5, Southern Brazil. Rev Saude Publica. 2008;42:51-9. [ Links ]
18. Malta DC, Cezario AC, Moura L, Neto OLM, Silva Jr. JB. Building surveillance and prevention for chronic non communicable diseases in the national Unified Health System. Epidemiol Serv Saude. 2006;15:47-65. [ Links ]
19. Campos GS. Political and organizational challenges in the Brazilian Unified National Health System: twenty years of public policy. Cad Saude Publica. 2008;24:2200-1. [ Links ]
20. Gouveia GC, Souza WV, Luna CF, Souza-Junior PRB, Szwarcwald CL. User satisfaction in the Brazilian health system: associated factors and regional difference. Rev Bras Epidemiol. 2009;12:281-96. [ Links ]
 Correspondence:
Correspondence:
Rafael Guerra Lund
Programa de Pós-Graduação em Odontologia
Faculdade de Odontologia - Universidade
Federal de Pelotas (UFPel)
Rua Gonçalves Chaves, 457/504
CEP: 96015-000 - Pelotas, RS, Brasil
E-mail: rafael.lund@gmail.com
Received for publication: September 28, 2011
Accepted: March 12, 2012













