Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.2 Piracicaba Abr./Jun. 2012
ORIGINAL ARTICLE
Sensitivity and accuracy of panoramic radiography in identifying calcified carotid atheroma plaques
Janaína Sens BastosI; Thalita Queiroz AbreuI; Sebastião Barreto de Brito FilhoII; Kelston Paulo Felice de SalesIII; Fernanda Ferreira LopesIV; Ana Emília Figueiredo de OliveiraV
IMSc student, Graduate Program in Dentistry, School of Dentistry, Federal University of Maranhão, Brazil
IIMSc, Professor, Department of Medicine II, School of Medicine, Federal University of Maranhão, Brazil
IIIMSc student in Vascular Surgery, School of Medicine, Federal University of São Paulo, Brazil
IVPhD, Professor, Discipline of Semiology, Department of Dentistry I, School of Dentistry, Federal University of Maranhão, Brazil
VPhD, Professor, Department of Dentistry I, School of Dentistry, Federal University of Maranhão, Brazil
ABSTRACT
Atherosclerosis is a chronic inflammatory disease that can cause death and physical and/or mental disabilities. It represents a serious public health problem owing to the high healthcare costs involved in rehabilitating patients. Among the different methods available for diagnosing atherosclerotic disease, color Doppler examination may be considered the "gold standard." On the other hand, panoramic radiography of the jaws (PRJ) is a diagnostic resource commonly used by dentists, and the obtained images allow examining other structures apart from the maxilla and the mandible.
AIM: To evaluate the sensitivity and accuracy of panoramic radiography in identifying calcified carotid atheroma, and compare the results to those obtained with color Doppler examination.
METHODS: Forty-two cervical regions were evaluated in panoramic radiographs and color Doppler scans. The kappa test (p < 0.05) was used to assess agreement between the examinations. Data were tested for sensitivity, specificity and negative predictive value, as well as positive and negative likelihood ratios.
RESULTS: The kappa value was 0.11. The sensitivity and specificity of PRJ were 73.9 and 36.8%, respectively, and the positive and negative likelihood ratios were 1.2 and 0.7, respectively.
CONCLUSIONS: Although a low correlation between PRJ and color Doppler examination was observed, as shown by the kappa test, the sensitivity of PRJ in identifying calcified carotid atheroma was considered acceptable.
Keywords: stroke, carotid artery diseases, radiography, panoramic.
Introduction
Atherosclerosis is an inflammatory disease that produces circulatory changes caused by fat deposits on the walls of the arteries. When the carotid arteries are involved, it can cause stroke – a cerebral vascular accident (CVA) – that can be ischemic or hemorrhagic1. The formation of atheromatous plaques in the carotid artery – also called calcified carotid atheromatous plaques (CCAP) – is not a simple and inevitable degenerative process resulting from advanced age, but rather a chronic inflammatory disease that can develop into an acute clinical condition owing to plaque rupture, rendering the patient susceptible to thromboembolism or stroke2.
Stroke is the third leading cause of death in the United States, accounting for over 150,000 deaths/year, ranking only behind cardiovascular disease and cancer3-4. By 2009, it was the first cause of death in Brazil, claiming over 300,000 deaths/year5. It represents a serious public health problem because it causes death and physical and/or mental disabilities– approximately 60% of survivors suffer from such disabilities6 –and have high costs involved in treating and rehabilitating patients.
The main risk factors said to favor or accelerate the atherosclerotic process are: heredity, dyslipidemia, smoking, hypertension, diabetes, viral infections, elevated homo-cysteine (an amino acid derived from eating meat and dairy products) in the blood, obesity, sedentary lifestyle and stress7. Preventive measures and early diagnosis are key factors to reduce the prevalence of the disease. However, a non-invasive, inexpensive and reliable diagnostic method still lacks. Angiography, which considered the "gold standard" for diagnosing this disease, is an invasive method that can cause major complications8, and Color Doppler (also known as Laser Doppler flowmetry or Duplex Scan), although fast, accurate, noninvasive and painless9, is not yet widely accessible to all strata of society because of its high costs (Figures 1A, 1B).
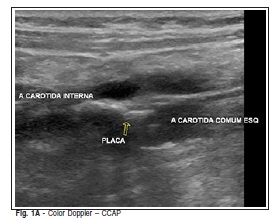
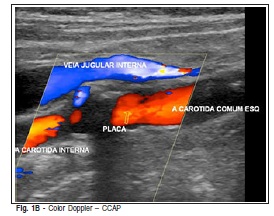
Since 1981, the presence of radiopaque images on panoramic radiographs has been described as a sign of the presence of CCAP10-11, indicating that this examination could contribute to the early diagnosis of stroke risk. There are studies reporting that partially calcified atherosclerotic lesions can be observed in panoramic radiographs of the jaws (PRJ)12-13. The image of the calcification is described as a nodular, radiopaque mass in one or more areas, either elongated or triangular, of various sizes, measuring from 1.5 to 4.0 cm, and as observable below and posteriorly to the angle of the mandible, adjacent to the intervertebral spaces between C2, C3, and C48,14-15 (Figures 2A, 2B).
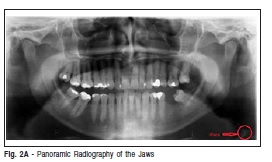
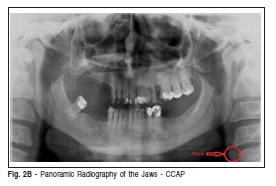
Some studies have reported calcifications in dental panoramic radiographs between the second, third and fourth cervical vertebrae, which were later confirmed by color Doppler examination as atheromatous plaques16-17. Because panoramic radiography may be able to detect CCAP during routine examinations, thus enabling proper referral of patients for appropriate treatment, it has the potential to promote a significant reduction in the morbidity rate caused by this disorder, and a substantial reduction in the healthcare costs associated with atherosclerosis18. Nevertheless, because panoramic radiographs cover several different anatomical areas, developing the ability to perform differential diagnosis of the structures that comprise the carotid region is of utmost importance. This ability involves comprehensive anatomical knowledge of structures such as the hyoid bone, epiglottis, calcified submandibular and styloid ligaments, and triticeouscartilage, as well as of pathological processes such as sialoliths, phleboliths, and calcified lymph nodes19.
In view of these considerations, it is reasonable to assume that PRJ has a great potential in identifying CCAP, or should at least be further investigated as a diagnostic tool for atherosclerosis. Nevertheless, there is still controversy in the literature about its use as a reliable method for this purpose, and great divergence in results. This could be explained by the different methodologies used and because the methods used for comparative analysis of panoramic radiographs in these studies are not considered the "gold standard," and are based solely on radiographic interpretation for diagnostic conclusion.
Based on the methodological limitations of the existing studies, on the fact that dentists use panoramic radiographs routinely, and on the fact that early detection of patients at risk for developing atherosclerosis is an important public health goal, the purpose of the present study was to evaluate the sensitivity and accuracy of PRJ in identifying CCAP compared with color Doppler examination.
Material and methods
Sample
In this study, the accepted ethical principles governing human experimentation were followed closely, after approval was obtained from the Ethics Committee of the Federal University of Maranhão (Protocol n. 2311-005753/2009-57).
The sample was calculated based on the estimated prevalence of calcification in the carotid artery, approximately 2%. The following parameters were used for calculating sample size: significance level of 0.05 and maximum permissible error of ± 5%, thus producing n = 31.
In the period from August 2009 to June 2010, panoramic two dental radiologists evaluated PRJ of patients of both genders in a clinic commissioned by the Public Health System in the city of São Luis, MA, Brazil. Radiographic diagnosis of CCAP was considered conclusive when there was agreement between both examiners regarding the presence of CCAP and the side in which its presence was detected. Twenty-one panoramic radiographs were considered by the examiners as undoubtedly positive for the diagnosis of CCAP, on at least one side, thus leading to an analysis of 42 cervical regions (n = 42).
The inclusion criteria for all participants of this study was the detection of an image suggestive of CCAP on at least one side of the PRJ in patients who were at least 40 years of age, and who agreed to undergo color Doppler angiography.
Radiographic examination
PRJ was performed using the standard positioning technique, Orthophos 3 Ceph X-ray equipment (Sirona Dental Systems GmbH, Germany) and 15 x 30 cm panoramic film (Eastman Kodak Co., Rochester, NY, USA). The films were processed automatically (Revell-XTec Ltd., São Paulo, SP, Brazil), with appropriate developer and fixer solutions (Kodak Brazilian Trade and Industry Ltd., Sao José dos Campos, SP, Brazil).
Interpretation of the radiographic images was performed by two dentists, with less than three years of experience as radiology specialists, and in an environment with dimmed light and using a light box. The presence of CCAP could be unilateral or bilateral. Both sides of each one of the 21 patients were evaluated, for a total of 42 cervical exams (n = 42).
Doppler Examination
All 21 patients with positive radiographic exams for CCAP on at least one side of the PRJ were subjected to Doppler examination at the Presidente Dutra University Hospital, São Luis, MA, Brazil. A Dupplex Scan equipment (General Electric, New York, USA) was used owing to its reliability in demonstrating blood flow in the artery under study. A physician specialized in angiology had previously determined the presence of stenosis and/or obstruction caused by an atheromatous plaque. In the same way as done in the radiographic examination, both sides of each exam were evaluated, also totaling 42 cervical analyses (n = 42).
Statistical methods
Data were analyzed statistically using BioEstat 5.0 software, according to criteria adopted by the related literature20. The kappa agreement test (p < 0.05) was used to assess and compare sensitivity, specificity, negative predictive value (NPV), accuracy (ACC), positive likelihood ratio (PLR) and negative likelihood ratio (NLR) for the different examinations. The kappa values and their interpretations were < 0 (no agreement), 0 to 0.19 (very weak agreement), 0.20 to 0.39 (poor agreement), 0.40 to 0.59 (moderate agreement), 0.60 to 0.79 (substantial agreement), and 0.8 to 1.0 (excellent agreement), following criteria previously approved21.
The sensitivity test was used to match the PRJ's ability to detect the disease when its presence was confirmed, i.e., to assess how many positive and negative results were found using PRJ for the cases found positive in the color Doppler examination ("gold standard")18. Sensitivity was calculated as follows:
Sensitivity (%) = true positives / (true positives + false negatives) x 100.
The specificity test was used to identify the true negatives determined by PRJ in individuals who were genuinely healthy, as revealed by the Doppler examination. It was calculated as follows:
Specificity = true negatives / (true negatives + false positives) x 100.
The NPV for PRJ was calculated to assess how many test results among those that proved negative were actually negative according to the Doppler examination. It was calculated as follows:
NPV (%) = true negatives / (true negatives + false negatives) x 100.
PRJ's accuracy was defined as the proportion of successful examinations, i.e., the total number of truepositives and true negatives, as confirmed by the Doppler examination. It was calculated as follows:
ACC = (true positives + true negatives) / total.
The likelihood ratio is a means of describing the performance of a diagnostic test. It expresses how many times the result of a given test is more likely (or less likely) to occur in affected subjects compared to unaffected subjects. If a test is dichotomized (positive/negative), two types of likelihood ratio describe its ability to separate those affected from those not affected: one associated with a positive test and another associated with a negative test, respectively calculated as follows:
PLR = sensitivity / (1 - specificity), and
NLR = (1 - sensitivity) / specificity.
Results
Of the 42 cervical analyses (L and R sides of 21 patients), 17 images visualized on the PRJ were confirmed by the Doppler examination (true positives), with 6 non-visualized sides (false negatives). PRJ identified 12 images of CCAP that were not confirmed by the Doppler examination (false positives), with 7 sides that were truly without disease (true negatives) (Table 1).
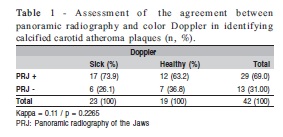
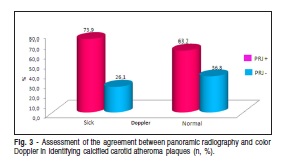
We found a kappa value of 0.11 (p = 0.2265), indicating that the agreement between the Doppler and the PRJ examinations was weak and not significant (Table 1). The sensitivity calculated for PRJ was 73.9%, indicating that 73 out of 100 patients with the disease were correctly identified and 26 were considered erroneously healthy. The calculated specificity was 36.8%, indicating that 36 out of 100 patients with the disease were identified as healthy and 63 were considered erroneously sick.
The NPV of PRJ was found to be 53.8%, indicating that 53 out of 100 patients who had a negative result in the PRJ examination actually did not have CCAP, or, stated differently, 53.8% of the diagnoses found to be negative by PRJ were correct, and 46.2% of the diagnoses initially considered negative by PRJ were actually positive in the color Doppler examination.
The likelihood ratios were as follows: PLR = 1.2 and NLR = 0.7. The higher the PLR, the better the test, and, in order to be considered a good test, the PLR should be significantly higher than 1. This would mean that a positive outcome is more likely to be a true-positive than a false-positive. The lower the NLR (closer to 0), the better the test. This would mean that a negative result is more likely to be a real negative than a false negative.
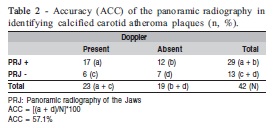
The accuracy found for PRJ was 57.1%, indicating that this examination provided a correct diagnosis – a true positive or a true negative – in 57 out of 100 patients. The sensitivity and accuracy results obtained with the use of PRJ for the identification of calcifications in the carotid artery indicate that this test could contribute to reducing the risk of patients suffering a stroke (Table 2).
Discussion
When atheromatous plaques of the carotid bifurcation region are identified, the first feature to note is the size of the obstruction. If it blocks less than 60% of the artery, simply inhibiting platelet aggregation associated with thrombus formation can treat the patient. When the obstruction is greater than 60%, invasive procedures are required to remove the plaque22. Panoramic radiography is limited to identifying CCAPs, and cannot evaluate its exact location, or the degree of the obliteration13.
The main limitation of this study was that the population evaluated consisted of a selective group (patients with an image suggestive of CCAP detected in panoramic radiographs), rather than the general population. Nonetheless, this bias can also be considered one of its strengths, from a methodological standpoint, because it compared the sensitivity and accuracy of PRJ to that of the "gold standard" method (Doppler) in identifying the presence of atherosclerotic plaques, considering that PRJ is an exam commonly requested by dentists, in which the occasional presence of CCAP is a radiographic finding.
The NPV found in this study was not substantial (63.2%), considering that atherosclerotic diseases are among the major causes of death worldwide. However, the sensitivity of PRJ in identifying CCAP was significant (73.9%) when compared to angiographic examination (color Doppler imaging), which is considered the "gold standard" (Figure 3).
Although the sensitivity of PRJ in identifying CCAP was 73.9%, its accuracy was only 57.1% and its specificity was 36.8%, a trend confirmed by the kappa test (0.11). Thus, PRJs should not be suggested as a diagnostic imaging examination for the identification of CCAP, as proposed by some authors. The results of the present study corroborate those of previous studies19, which stated that a radiopacity between C2, C3 and C4 in a panoramic radiograph does not always represent a CCAP.
Our results differ from those of a previous study23 that found PRJ sensitivity and specificity values of 22.2% and 90.0%, respectively, for identifying CCAP using CT as the "gold standard." The authors also concluded that panoramic radiographs could be considered a diagnostic method with moderate accuracy and low sensitivity for the detection of CCAP. This difference may be explained by the different "gold standards" adopted for comparison with PRJ.
In a previous study24, PRJ presented low sensitivity and no accuracy for detecting calcification or stenosis. Only one dental radiologist interpreted the panoramic radiographs in that study, and the authors used two different radiographic xray apparatuses (Siemens Corp., Iselin, New Jersey, USA or Gendex Corp., Milwaukee, Wisconsin, USA) for image acquisition. In contrast, the authors also mentioned that the Doppler images were obtained at various locations, and interpreted by different radiologists.
A study assessing the performance of digital PRJ in forty patients with carotid atherosclerotic disease diagnosed by angiography found NPV and sensitivity values of 46% and 60%25, which differ from those found in our study (53.8% and 73.9%, respectively). One possible explanation for this divergence in results is the different characteristics of the projection devices used, particularly the rotation system, the section thickness and the apparatus calibration19.
A survey8 conducted at the Health Department of the city of Valença, RJ, Brazil, reviewed panoramic radiographs and Doppler images of 16 patients to investigate whether there was agreement between the diagnosis of CCAP in the Doppler color and in the PRJ images. The results indicate substantial agreement between these tests (kappa = 0.78), contrasting with those of the present study. This difference may be explained by the different sample sizes and by the different number of evaluators used to assess the panoramic radiographs.
In another study8, calcifications were observed in 9.4% of PRJs, but not confirmed by the color Doppler examination, and were considered false positives; in the same study, 3.1% of results were considered false negatives, meaning that the color Doppler examination revealed the presence of calcifications that went undetected in the PRJs. In contrast, Fig. 3 - Assessment of the agreement between panoramic radiography and color Doppler in identifying calcified carotid atheroma plaques (n, %). the present study showed even higher values for false positives (63.2%) and false negatives (36.8%).
It is noteworthy that the identification of CCAP in panoramic radiographs may not be a simple task. Published articles8,23, and ours alike, have used dental radiologists in their methodology, leading one to believe that false results, whether positive or negative, could be even greater if the radiographic analysis were performed by general dentists, less trained to visually identify pathologies. A previous study8 showed that a general dentist, who is more familiar with evaluating the maxilla, mandible and temporomandibular joint cannot adequately perform the identification of CCAP in panoramic radiography. In that study8, dental radiologists found evidence of calcification in the carotid artery in 9 out of 1,818 panoramic radiographs examined, whereas the general dentist, examining the same panoramic radiographs, failed to identify any of these calcifications.
Misinterpretation could be linked to the various anatomical structures existing in the cervical region studied, representing differential diagnoses. In 1981, when the panoramic radiograph was described for the first time as an aid in identifying patients at risk for stroke, calcification in the region of the carotid artery bifurcation was identified in 2% of cases, of which 88% were actually carotid artery calcifications and the remaining 12% were calcified lymph nodes or salivary calculi11.
Although PRJ may not be considered a reliable method to detect calcifications in the carotid artery, it should be used as a referral for the Doppler25 examination (the "gold standard") and other specialists8.
Merely detecting calcifications or stenosis of the carotid artery in PRJ is of limited value in assessing the risk of stroke, insofar as it does not take into account plaque vulnerability26-28. According to a recommendation of the American Heart Association, physicians should routinely assess the vulnerability of all major arterial plaques27, including their morphology, as well as biochemical and molecular factors, none of which can be identified by means of panoramic radiography.
Dental clinicians should refer all patients with atheromalike lesions to a physician, since early aggressive treatment has been shown to reduce strokes, fatal or otherwise11. On the other hand, owing to the wide divergence of results observed, it remains unclear whether dentists could be adequately trained to reduce the number of false positive diagnoses to an acceptable level. Otherwise, unnecessary referrals to physicians could occur, leading to unnecessary tests and increased healthcare spending29. We believe that knowledge of this topic should be generalized, and general dentists should be trained in identifying carotid artery alterations.
Within the limitations of the present study, PRJ presented good sensitivity and only moderate accuracy in identifying calcified carotid atheroma plaques compared with color Doppler examination. These results were confirmed by the observed positive likelihood and negative likelihood ratios. These results support previous findings and point to enhancing the prospects of an interdisciplinary approach, where dentists can refer their patients to other specialists, who, in turn, may reach a definitive diagnosis based on specific tests and prescribe the proper treatment.
References
1. Manual Merck. [cited 2012 Feb 6]. Available from:http://mmspf.msdonline.com.br/pacientes/manual_merck/ secao_03/cap_026.html.
2. Lusis AJ. Atherosclerosis. Nature. 2000; 407: 233-41. [ Links ]
3. Hertzer NR, O'Hara PJ, Mascha EJ, Krajewski LP, Sullivan TM, Beven EG. Early outcome assessment for 2228 consecutive carotid endarterectomy procedures: the Cleveland clinic experience from 1989 to 1992. J Vasc Surg. 1997; 26: 1-10. [ Links ]
4. Almog DM, Illig KA, Khin M, Green RM. Unrecognized carotid artery stenosis discovered by calcifications on a panoramic radiograph. J Am Dent Assoc. 2000; 131, 1593-7. [ Links ]
5. Ministério da Saúde. [cited 2012 Feb 6]. Available from: http://189.28.128.178/sage/. [ Links ]
6. Uthma, AT, Al-Saffar, AB. Prevalence in digital panoramic radiographs of carotid area calcification among Iraqi individuals with stroke-related disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105: 68-73. [ Links ]
7. Azevedo JRD. Aterosclerose. [cited 2012 Feb 6] .Available from: http://boasaude.uol.com.br/lib/ShowDoc.cfm?LibDocID=3118& Return CatID=1770. [ Links ]
8. Romano-Sousa CM, Krejci L, Medeiros FMM, Graciosa-filho RG, Martins MFF, Guedes VN, et al. Diagnostic agreement between panoramic radiographs and color Doppler images of carotid atheroma. J Appl Oral Sci. 2009; 17: 45-8. [ Links ]
9. Frauchiger B, Schimid HD, Roedel C, Moosmann P, Staub D. Comparison of carotid arterial resistive indices with intima-media thickness as sonographic markers of atherosclerosis. Stroke. 2001; 32: 836-41. [ Links ]
10. Levy BA, Mandel DDS. Calcified carotid artery imaged by computed tomography. J Oral Maxillofac Surg. 2010; 68: 218-20. [ Links ]
11. Friedlander AH, Lander A. Panoramic X-ray identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol. 1981; 51: 102-4. [ Links ]
12. Friedlander AH. Identification of stroke prone patients by panoramic and cervical spine radiography. Dentomaxillofac Radiol. 1995; 24: 160-4. [ Links ]
13. Manzi FR, Tuji FM, Almeida SM, Neto FH, Bóscolo FN. Panoramic radiography as an auxiliary in detecting patients at risk for cerebrovascular accident. Rev Assoc Paul Cir Dent. 2001; 55: 131-3. [ Links ]
14. Senosiain-Oroquitea A, Pardo-López B, de Carlos-Villafranca F, González-Montoto, Cobo-Plana J. Detección de placas de ateroma mediante radiografias dentales. RCOE. 2006; 11: 297-303. [ Links ]
15. Pornprasertsuk-Damrongsri S, Thanakun S. Carotid artery calcification detected on panoramic radiographs in a group on Thai population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101: 110-5. [ Links ]
16. Freymiller EG, Sung EC, Friedlander AH. Detection of radiation-induced atheromas by panoramic radiography. Oral Oncology. 2000; 36: 175-9. [ Links ]
17. Almog DM, Tsimidis K, Moss ME, Gottilieb RH, Carter LC. Evaluation of a training program for detection of carotid artery calcifications on panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 90: 111-7. [ Links ]
18. Ramesh A, Pabla T. Panoramic radiographs: a screening tool for calcified carotid atheromatous plaque. J Mass Dent Soc. 2007; 56: 20-1. [ Links ]
19. Kamikawa RS, Pereira MF, Fernandes A, Meurer MI. Study of the localization of radiopacities similar to calcified carotid atheroma by means of panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102: 579-81. [ Links ]
20. Ayres M, Ayres Jr M, Ayres DL, Santos AS. BioEstat Versão 5.0.Belém: Sociedade Civil Mamirauá, MCT-CNPq; 2007. [ Links ]
21. Teixeira AC, Cruvinel DL, Roma FR, Luppino LF, Resende LHP, Sousa T, et al. Evaluation of the agreement between clinical and laboratorial exams in the diagnosis of leprosy. Rev Soc Bras Med Trop. 2008; 41: 48-55. [ Links ]
22. Guimarães GO, Oliveira IE, Nobile Junior D, Messina Calderón JC, Saddy MS. Radiografia panorâmica: identificação de pacientes suscetíveis ao acidente vascular cerebral por meio da detecção de ateromas na bifurcação da carótida. ConScientiae Saúde 2005; 4: 97-104. [ Links ]
23. Yoon SJ, Yoon W, Kim OS, Lee JS, Kang BC. Diagnostic accuracy on panoramic radiography in the detection of calcified carotid artery. Dentomaxillofac Radiol. 2008; 37: 104-8. [ Links ]
24. Madden RP, Hodges JS, Salmen CW, Rindal DB, Tunio J, Michalowicz BS, et al. Panoramic Radiography Does Not Reliably Detect Carotid Artery Calcification Nor Stenosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103: 543-8. [ Links ]
25. Damaskos S, Griniatsos J, Tsekouras N, Georgopoulos S, Klonaris C, Bastounis E, et al. Reliability of panoramic radiograph for carotid atheroma detection: a study in patients who fulfill the criteria for carotid endarterectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106: 736-42. [ Links ]
26. Nighoghossian N, Derex L, Douek P. The vulnerable carotid artery plaque: current imaging methods and new perspectives. Stroke. 2005; 36: 2764-72. [ Links ]
27. Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part I. Circulation. 2003; 108: 1664-72. [ Links ]
28. Bhatia V, Bhatia R, Dhindsa S, Dhindsa M. Imaging of the vulnerable plaque: new modalities. South Med J. 2003; 96: 1142-7. [ Links ]
29. Farman AG, Farman TT, Khan Z, Chen Z, Carter LC, Friedlander AH. The role of the dentist in detection of carotid atherosclerosis. SADJ. 2001; 56: 549-53. [ Links ]
 Correspondence:
Correspondence:
Janaína Sens Bastos
Rua 01, Lote 08, Condomínio Village Intermares,
Casa 31 - Planalto Vinhais I
CEP: 65074-856 - São Luís – MA, Brasil
E-mail: janaina100s@gmail.com
Received for publication: November 29, 2011
Accepted: April 18, 2012













