Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.2 Piracicaba Abr./Jun. 2012
ORIGINAL ARTICLE
Musculoskeletal disorders in upper limbs in dental students: exposure level to risk factors
Patrícia Petromilli Nordi Sasso GarciaI; Camila PinelliII; Juliana dos Reis DerceliIII; Juliana Álvares Duarte Bonini CamposI
IDDS, MS, Adjunt Professor, Department of Community Dentistry, Araraquara School of Dentistry, UNESP – Univ Estadual Paulista, Araraquara, SP, Brazil
IIDDS, MS, Assistant Professor Doctor, Department of Community Dentistry, Araraquara School of Dentistry, UNESP – Univ Estadual Paulista, Araraquara, SP, Brazil
IIIDDS, Master student in Restorative Dentistry, Department of Restorative Dentistry, Ribeirão Preto School of Dentistry, USP – University of São Paulo, Ribeirão Preto, SP, Brazil
ABSTRACT
AIM: This study assessed the risk factors of undergraduate students to develop musculoskeletal disorders (MSD) in the upper limbs, regarding gender, type of dental clinical procedure, mouth region treated, and the four-handed dentistry practice.
METHODS: Dental students enrolled in the 8th semester in the Araraquara School of Dentistry, UNESP, Brazil, were photographed while practicing 283 dental procedures. The Rapid Upper Limb Assessment (RULA) method was used to evaluate the working postures of each student. The photographs were evaluated and a final risk score was attributed to each analyzed procedure. The prevalence of risk factors of developing MSD was estimated by point and by 95% confidence interval. The association between the risk factor of developing disorders and variables of interest were assessed by the chi-square test with a significance level of 5%.
RESULTS: The risk factors of developing MSD were high, regarding most dental procedures performed by the undergraduate students (score 5: 7.07%, CI95%: 4.08-10.06%; score 6: 62.54%, CI95%: 56.90-68.18%). There was no significant association between the RULA final score and gender (p=0.559), and type of dental procedure (p=0.205), and mouth regions by arch (p=0.110) or hemi-arch (p=0.560), and the use of four-handed dentistry (p=0.366).
CONCLUSIONS: It can be concluded that gender, type of dental clinical procedure, mouth region treated, and practice of four-handed dentistry did not influence the risk of developing MSD in the upper limbs among the dental students evaluated; however, they are at a high risk of developing such disorders.
Keywords: human engineering, dentistry, occupational health, students, dental.
Introduction
Due to the restricted work area, the need for manual dexterity, the long time in a sitting position, without breaks, and the needed firmness and stability of the hands, dentistry is a profession that requires prolonged periods of static muscle activity, which can lead to musculoskeletal disorders (MSD)1-4.
The MSD related to this type of work activity are mainly in the upper limbs and may result in sick leave, reduced productivity and/or having to abandon the professional career4-6. The most common MSD in dentistry are chronic low back pain, neck tension syndrome, trapezius myalgia, shoulder joint injury e carpal tunnel syndrome and upper extremity tendonitis7. De Carvalho et al.8 (2001) emphasize that dentists are among those most susceptible to develop MSD, such as tendonitis, synovitis, tenosynovitis and bursitis.
Studies have indicated a wide variety of causative factors associated withMSD in dentistry. Some of these result from the physical burden of clinical work and the psychosocial factors since the beginning of a dentists' academic training, or during their undergraduate course3,5-6,9. Within the psychosocial factors one can also highlight the lack of prospects for professional growth, pressures at work, work-related negative influence on private life, the need to deal with difficult people, work routine, problems with the dental staff and work-related stress10.
However, there is little research investigating the prevalence of MSD among dental students2-3,5,7-8,11. Therefore, given the pressures of tertiary education and the physical burden of clinical training, this seems to be an area that lacks research, which needs to be explored, since the problems may actually begin during the training period. This study was carried out to assess the level of risk factors of MSD in the upper limbs of undergraduate dental students by gender, regarding gender, type of dental clinical procedure, mouth region treated, and the four-handed dentistry practice.
Material and methods
Sample Design
This was an observational study. All students (n=75) of both genders, enrolled in the 8th semester of the undergraduate course at the School of Dentistry Araraquara – UNESP were invited and agreed to participate. As sampling unit, all clinical procedures performed by students (n=283) were considered over a period of two months at the Integrated Clinic twice a week. On average, 3.8 procedures were performed per student. The study was approved by the local Ethics Committee (protocol # 40/08).
Recording the work postures
The work postures during the various clinical procedures were photographed using a CANON 5.0 G5 digital camera. In order to enable viewing the process of the body regions, three key points were defined in a pilot study, and then photographed in the experiment. The pilot study was based on the definition of points to take the photographs, training the operator and intra-examiner calibration. To define the points in a simulated procedure, several photographs were taken of different regions regarding the operator and the dental chair. In order to better visualize the regions to be evaluated by the Rapid Upper Limb Assessment (RULA) method, during the training of the individual responsible for the photographs, it was stipulated that the photographs should be obtained sequentially, holding the camera at about 1.5 m. from the ground, at the height of the eyes. For intra-examiner calibration, 10 undergraduate students were photographed during 50 clinical procedures, which were not included in the definitive experiment. To estimate the reliability of the angular deviation measurement by the Image-Tool software (UTHSCSA, Houston TX, USA), the photographs were analyzed in duplicate, with a one-week interval between assessments.
The photographs were taken by a regular dental surgeon researcher, previously trained in the pilot study, who was different from the professor in ergonomics. Such procedure avoided interferences with work postures, which means that the students were not behaving artificially while the photographs were taken. The photographs were taken at least 10 min after the surgical procedures started, hence allowing the students to become comfortable in their postures2.
The sequential photographic records for different parts of the body were carried out with the photographer holding the camera close to the eyes at a distance of about 1.5 m from the ground, orthogonally.
Although the students had previously authorized being photographed for the study, the idea was that photographer would go unnoticed and without interfering in the dentistpatient procedure. All photographs were taken and then analyzed by the Dental Ergonomics Professor, who was previously calibrated in the pilot study (k=0.91). The Image-Tool software12 was used for measuring the angles of the body regions of interest for further analysis with the RULA method.
Posture assessment method
The RULA method was used, according to McAtamney and Corlett13 (1993). It uses a posture assessment diagram and three score tables. When associated, such score tables allow assessing the exposure to risk factors for developing MSD, by using the risk scores. This method analyzes only one side of the body and produces a final risk score for it. In the present study, the side evaluated corresponded to the dominant hand of the student.
In accordance with RULA, the individual's body is divided into two groups: A and B. Group A corresponds to the regions of the arm, forearm and wrist, and group B corresponds to the region of the neck, trunk and legs. For each of these six segments, a score is issued, depending on the observed posture. The lowest scores are related to the positions with the least risk factors. These scores (A and B) must be added to the scores related to the way the assessed muscle group is used (a static posture maintained for longer than a minute or repeated more than four times per minute) and the load/force the muscle is subjected to (endurance, intermittent force or load of the object being manipulated).
It should be noted that score 1 was standardized for the muscle and score 0 for force/load, following the recommendations of Gandavadi, Ramsay and Burke2 (2007), as the musculature used in dental work is static, and the external load used does not exceed 2 kg.
According to the RULA method, the final risk scores range from 1 to 7. Scores 1 to 2 are considered low risk, in other words acceptable. Scores 3 to 4 represent medium risk, pending further investigations for postural changes to be undertaken in the long term. Scores 5 and 6 are of high risk, requiring a prompt investigation for changes to be made in the short term. A score 7 is considered a significantly high risk for MSD, that is, investigations and changes in these work postures should be performed immediately to reduce the excessive load on the musculoskeletal system and the individual's risk of injury.
Assessing the procedures performed
A final risk score was obtained for each dental procedure by analyzing the photographs of students performing various clinical procedures.
The dental procedures were categorized and divided into: "preparatory", which are those that prepare the oral cavity to receive the restorative/rehabilitation treatment (clinical examination, dental scaling and polishing, endodontic treatments, extractions and periodontal surgery), and "restorative/rehabilitation", which are those that restore the lost dental tissue (sealing with resin materials or glass ionomer cements, provisional restorations, glass ionomer cement, amalgam and composite resin restorations) or replace lost teeth (implant-supported dentures, fixed, removable and complete dentures). All procedures were categorized and divided according to guidelines adopted by the Integrated Clinic course at the School of Dentistry of Araraquara, UNESP, Brazil.
Statistical analysis
The prevalence of the exposure level to risk factors for MSD in the upper limbs was estimated by point and by 95% of confidence interval. The final score of the risk obtained by RULA is the dependent variable, and gender, type of procedure performed, four-handed work practice and mouth region treated are the independent variables. The association between the variables of interest was analyzed using the Chi-square test (χ2). A significance level of 5% was used for all analyses.
Results
Among the 283 clinical activities, female students performed 71.02%, and most activities were restorative/rehabilitation procedures (60.78%), performed by the fourhanded method (65.37%) and carried out in the upper arch (57.60%).
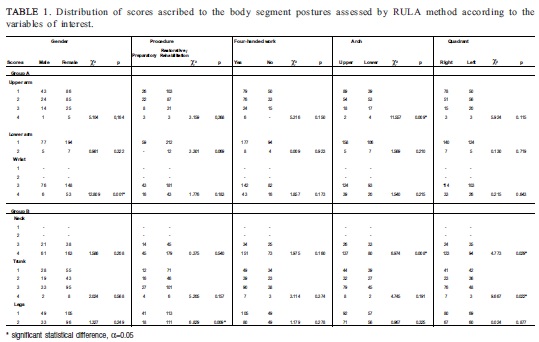
Table 1 shows the results of the association between the scores assigned to the positions of body segments and the variables of interest (gender, type of procedure, four-handed work practice, and mouth region treated).
The body parts with less risk score were the arm and forearm, while the wrist and neck showed the highest risk scores.
A significant association was observed between wrist score and gender (χ2=12.809; p=0.001), with women showing higher wrist scores. There was only significant association between the scores ascribed to the surgical procedure performed and the legs of the students surveyed (χ2=6.829; p=0.009), with higher risk scores when performing restorative/rehabilitation procedures. No statistically significant association was observed among the scores ascribed to all body segments and to the four-handed procedure.
Regarding the associations with the region of the mouth ("upper"/"lower" and "right"/"left"), the procedures performed in the whole mouth were excluded (n=7) because they did not allow assessing the arches (upper/lower) independently.
There were a larger number of procedures with high neck scores when working in the upper region (χ2=6.974;p=0.008) and on the right side (χ2=4.773; p=0.029) of the mouth. Regarding the arm, there was a larger number of procedures in the upper region, when compared with the lower region of the mouth (χ2=11.557; p=0.009). The trunk showed a higher score, when working on the right quadrant (χ2=9.667; p=0.022), regardless of the low or top arch.
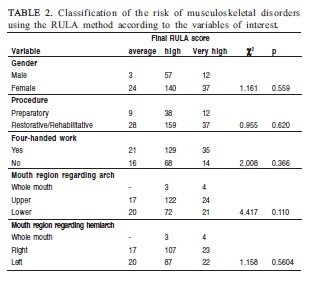
Considering the dental procedures performed, the risk of MSD in the upper limbs, based on the final RULA score, were classified as medium in 13.07% (IC95%: 9.14-17.00%), high in 69.61% (IC95%: 64.25-74.97%) and very high in 17.31% (IC95%: 12.90-21.72%) of the individuals assessed.
Table 2 shows the distribution of the final risk classification of MSD, according to the variables of interest.
There was no significant association between the risk classification and the variables of interest (gender, type of procedure performed, four-handed work practice, and the mouth region treated).
Discussion
The risk assessment of MSD in the upper limbs among dentists is important due to the specificity of the work place and the activity performed.
There are several risk assessment methods for such disorders13-19. In this study, the RULA method was selected for assessing the risk, since it enables a prompt and appropriate study of the individuals' workload, regardless of their professional area2.20-21.
Because the body is divided into segments, according to the RULA method, it is possible not only to obtain a final risk score of the individual, but also to observe the body parts that contribute to a greater or lesser intensity, in order to obtain the individual's final risk score. Thus, with the accuracy of the methodology used in RULA, as well as its reliability and validity, measured by the study of McAtamney and Corlett13 (1993), the important contribution of the present study for the area of ergonomics applied to dentistry is endorsed, since there is a scarcity of studies, especially among undergraduate dental students5.7-8.
It was found that the wrist and neck were the body parts that had higher risk scores. This result can be explained by the fact that the dentist works in an area that is small, dark and difficult to access, with the patient lying in the dental chair and the professional making movements to use several instruments to preform procedure that require force, extension, flexion, pronation, supination and rotation of the wrists. All this increases the risk of MSD3,9,22-23.
Moreover, despite the patient's proper positioning in the dental chair and the dentist striving to maintain a neutral and balanced posture according to the basic requirements of an ergonomic posture4, the continuous work performed in front of or below the dentist's eyes leads to a slight head tilt forward and down to have the best viewing angle6, which is achieved when a distance of 30 cm to 40 cm is maintained between the operator's eyes and the patient's mouth4. If such distance is reduced, there is a need for a greater inclination of the neck forward. If this is done over a long period of time, the cervical spine is not able to support the whole spine and muscles of the neck. Also, the upper chest will constantly constrict in order to bear the weight of the head forward, hence resulting in a painful symptom pattern called Neck Tension Syndrome6.
Regarding the high risk score observed in the wrist of the individuals, it should be considered that despite all technological and scientific advances, a dental surgical procedure is essentially manual, which can cause an overload on the wrists. According to Fish and Morris-Allen24 (1998), in professions such as dentistry, which require the use of small hand tools, the permanence of the wrist joint at rest seems impossible because certain medical procedures require that the wrist remains bent for a certain amount of time. This continuous flexing of the wrist may increase the risk of professionals to be affected by the carpal tunnel syndrome25.
Analyzing the risk of MSD in relation to gender, it was observed that female subjects had higher wrist scores than males ( Table 1). According to Coury et al.26 (2001) men and women may develop different movement strategies to perform the same task as they have different body size, muscle strength and aerobic capacity. This assertion can justify the results obtained in this study, which raises concern. The higher load on the wrists of female subjects, combined with a greater number of domestic tasks26-27 and the influence of sex hormones on the articulation26 may render this group to be more susceptible to developing MSD in the wrist when actually performing the profession.
Regarding the type of procedure, there was a significant association only with the legs, with greater postural constraints when performing restorative/rehabilitation work ( Table 1). When observing the leg risk scores, it was found that body weight was inappropriately distributed between the legs and feet of the operators in this type of procedure, which can be explained by their higher mental and physical demands when treating patients.
With regard to the four-handed work practice, there was no significant association with the risk score of different body parts. An interesting fact is that Marshall et al.28 observed that professionals working four-handed reported having more pain than those who did not, suggesting that this type of work was unable to prevent MSD and neurological symptoms. However, the professionals assessed reported that they had not been trained in four-handed work, which might have influenced or contributed to the results obtained.
Regarding the association between the scores of body parts and the oral cavity region to be treated, a significant association was observed for the arm and neck scores, when compared to the arch (upper/lower) and the neck and trunk, in relation to the quadrant (right/left) ( Table 1).
The work in the lower region presented higher arm scores, because the students were possibly working with their shoulders and/or elbows raised, a posture usually adopted when they do not position the dental chair horizontally for oral cavity procedures. Specifically in the lower arch, the students tend to keep the backrest of the seat relative to the seat at an angle greater than 30 degrees because they believe that the more it is raised, the more operative space they will be able to see. However, by raising the backrest, the patient's mouth ultimately is much higher than the operator's elbows, even with the backrest of the dental chair fully lowered. In this situation, to have access to the operative field, the student lifts his shoulders or elbows.
In the case of the upper arch, the student does not position the patient with the backrest as high as he does for the lower arch, but then the patient is not in a position where the upper occlusal plane is perpendicular to the ground, which is recommended for a direct view when working on the arch4. He then needs to change his posture, and in this case, it is not the access to the operative field that is difficult, but rather his view. Thus, to facilitate a direct view of the arch, he leans his neck too far out, with this inclination often associated to the trunk.
Regarding the work quadrant (right/left), the right side was related to higher scores in both the neck and trunk. While it is believed that the quadrant corresponding to the dentist's working side, the right side, enables a more appropriate working posture, it is a mistake in some situations, because if the patient is not properly positioned in the dental chair, visualization of the operative field is in fact difficult, requiring the inclination and/or torsion of the neck and trunk.
By analyzing the results of the arch and the work quadrant, the main factor assumed to have influenced getting the high risk scores in some parts of the body (arms, neck and trunk) was the patient's inadequate positioning in the dental chair, which rendered access and viewing difficult to achieve. According to Valachi and Valachi4 (2003) placing the patient in an awkward position can result in a prolonged static muscle tension in the neck and shoulders. As a result, the authors recommended that the patient's positioning must be according to the mouth region to be treated.
The risk scores assessment for each segment of the body enabled observing the influence of specific body parts in the final RULA score. However and additionally, getting the final RULA score is vital, since it generally expresses the individual's risk to develop MSD in the upper limbs over time2,13,20. A high percentage of procedures performed by dental undergraduate students was observed and classified as high risk.
There was no significant association between the final RULA score and the variables of interest ( Table 2), indicating that the difficulties intrinsic to the dental practice can lead to possible MSD3,9,22-23,28-29, irrespective of the nature of work performed.
Another fact worth mentioning is that the wrong posture adopted by students during the course may perpetuate and worsen over time, especially when they later work as dentists5. Moreover, during their activities, while the undergraduate students might be subject to all kinds of discomforts, many health problems will only become apparent over time. Unfortunately, during their undergraduate course, they are more concerned with the procedure they are performing than with how they are performing it.
One should also consider that although these students, still in their pre-clinical life, are educated and instructed to work in the different regions of the oral cavity using ergonomic postures, with the patient and equipment properly placed, their postures may be influenced by harmful habits acquired from different experiences, not always based on the ergonomics requirements30.
This way, studies that analyze early on the prevalence and progression of MSD in dental students are truly needed, because the methods the students use to acquire manual dexterity in the first years of dental school can influence how these disorders will be developed and continued in the future11.
In conclusion, in the analysis of the different body segments and the variables of interest, there was significant association only between gender and wrist, between type of procedure and legs, and between treated mouth region, arm, neck and trunk. For most procedures performed by the undergraduate students, the final risk score using the RULA method was classified as high, with no significant association between them and the gender, type of procedure performed, four-handed work practice and treated mouth region.
References
1. Prasad V, Pratheeth G, Madhumietha A. Repetitive strain injuries and its incidence in practicing dentists. Int J Comtemp Dent. 2011; 2: 6-11. [ Links ]
2. Gandavadi A, Ramsay JRE, Burke FJT. Assessment of dental student posture in two seating conditions using RULA methodology - a pilot study. Br Dent J. 2007; 203: 601-5. [ Links ]
3. Melis L, Abou-Atme YS, Cottogno L, Pittau R. Upper body musculoskeletal symptoms in Sardinian Dental Students. J Can Dent Assoc. 2004; 70: 306-10. [ Links ]
4. Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003; 134: 1604-12. [ Links ]
5. Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professional. Int J Dent Hyg. 2009; 7: 59-165. [ Links ]
6. Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003; 134: 1344-50. [ Links ]
7. Werner RA, Franzblau A, Gell N, Hamann C, Rodgers PA, Caruso TJ, et al. Prevalence of upper extremity symptoms and disorders among dental and dental hygiene students. J Calif Dent Assoc. 2005; 33: 123-31. [ Links ]
8. Carvalho MVD, Soriano EP, Caldas Jr AF, Campello RIC, Miranda HF, Cavalcanti FID. Work-related musculoskeletal disorders among Brazilian dental students. J Dent Educ. 2009; 73: 624-30. [ Links ]
9. Lindfors P, Thiele U, Lundberg U. Work characteristics and upper extremity disorders in female dental health workers. J Occup Health. 2006; 48: 192-7. [ Links ]
10. Gambhir RS, Singh G, Sharma S, Brar R, Kakar H. Occupational health hazards in current dental profession – a review. Open Occup Health Saf J. 2011; 3: 57-64.
11. Rinsing DW, Bennett BC, Hursh K, Plesh O. Reports of body pain in a dental students population. J Am Dent Assoc. 2005; 136: 81-6. [ Links ]
12. Wilcox DC, Dove SB, McDavid WD, Greer DB. UTHSCSA ImageTool - Version 3.0. [cited 2012 Feb 22] Available from: http://compdent.uthscsa.edu/dig/itdesc.html. [ Links ]
13. McAtamney L, Corlett EN. RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon. 1993; 24: 91-9. [ Links ]
14. Bao S, Howard N, Spielholz P, Silverstein B. Two posture analysis approaches and their application in a modified rapid upper limb assessment evaluation. Ergonomics. 2007; 50: 2118-36. [ Links ]
15. Fransson-Hall C, Gloria R, Kilbom A, Winkel J, Karlqvist L, Wiktorin C. A portable ergonomic observation method (PEO) for computerized on-line recording of postures and manual handling. Appl Ergon. 1995; 26: 93-100 [ Links ]
16. Karhu O, Härkönem R, Sorvali P, Vepsäläinem P. Observing working postures in industry: examples of OWAS application. Appl Ergon. 1981; 12: 13-7. [ Links ]
17. Kemmlert KL. A method assigned for the identification of ergonomics hazards - PLIBEL. Appl Ergon. 1995; 26: 199-211. [ Links ]
18. Kilbom A, Person J. Work technique an its consequence for musculoskeletal disorders. Ergonomics. 1987; 30: 273-9. [ Links ]
19. Seth V, Weston RL, Freivalds A. Development of a cumulative trauma disorder risk assessment model for the upper extremities. Int J Ind Ergon. 1999; 23: 281-91. [ Links ]
20. Fountain LJK. Examining RULA'S postural scoring system with selected physiological and psychophisiological measures. Int J Occup Saf Ergon. 2003; 9: 375-84. [ Links ]
21. Massaccesi M, Pagnotta A, Soccetti A, Masali M, Masiero C, Greco F. Investigation of work-related disorders in truck drivers using RULA method. Appl Ergon. 2003; 34: 303-7. [ Links ]
22. Biswas R, Sachdev V, Jindal V, Ralhab S. Musculoskeletal disorders and ergonomic risk factors in dental practice. Indian J Dent Pract. 2012; 4: 70-4. [ Links ]
23. Sarkar PA, Shigli AL. Ergonomics in General Dental Practice. People´s J Scient Res. 2012; 5: 56-60. [ Links ]
24. Fish DR, Morris-Allen DM. Musculoskeletal disorders in dentists. New York State Dent J. 1996; 64: 44-8. [ Links ]
25. Hamann C, Werner RA, Franzblau A, Rodgers PA, Siew C, Gruninger S. Prevalence of carpal tunnel syndrome and median mononeuropahty among dentists. J Am Dent Assoc. 2001; 132: 163-70. [ Links ]
26. Coury HJCG, Porcatti IA, Alem MER, Oishi J. Influence of gender on work-related musculoskeletal disorders in repetitive tasks. Int J Ind Ergon. 2001; 29: 33-9. [ Links ]
27. Nordander C, Ohlsson K, Balogh I, Hansson GA, Axmon A, Persson R, et al. Gender differences in workers with identical repetitive industrial tasks: exposure and musculoskeletal disorders. Int Arch Occup Environ Health. 2008; 81: 939-47. [ Links ]
28. Nutalapati R, Gaddipati R, Chitta H, Pinninti M, Boyapati R. Ergonomics in Dentistry and the prevention of musculoskeletal disorders in dentists. Internet J Occup Health. 2010; 1: 1-9. [ Links ]
29. Garbin AJÍ, Garbin CAS, Diniz DG, Yarid SD. Dental students' knowledge of ergonomic postural requirements and their application during clinical care. Eur J Dent Educ. 2011; 15: 31-5. [ Links ]
30. Gupta S. Ergonomic applications to dental practice. Indian J Dent Res. 2011; 22: 816-22. [ Links ]
 Correspondence:
Correspondence:
Patrícia Petromilli Nordi Sasso Garcia
Rua Humaitá 1680, Centro
CEP:14801-903 - C.P.331 - Araraquara, SP - Brasil
E-mail: psgarcia@foar.unesp.br
Received for publication: May 03, 2012
Accepted: June 15, 2012