Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.2 Piracicaba Abr./Jun. 2012
ORIGINAL ARTICLE
Role of periodontics in the treatment to traumatized teeth: a 4-year retrospective evaluation
Adriana de Jesus SoaresI; Mariana Amade Mendes BrazãoII; Renato Correa Viana CasarinIII; Juliana Yuri NagataIV; Márcio Zaffalon CasatiIII; Francisco José de Souza FilhoV
ICollaborator Professor, Department of Restorative Dentistry, Endodontics Area, UNICAMP - University of Campinas, Piracicaba, SP, Brazil
IIMaster's degree student, São Leopoldo Mandic Institute and Research Center, Campinas, SP, Brazil
IIIFull professor, UNIP - Paulista University, São Paulo, SP, Brazil
IVPhD student, Department of Restorative Dentistry, Endodontics Area, UNICAMP - University of Campinas, Piracicaba, SP, Brazil
VFull Professor, Department of Restorative Dentistry, Endodontics Area, UNICAMP - University of Campinas, Piracicaba, SP, Brazil
ABSTRACT
Treatment of dental trauma should be planned based on a multidisciplinary approach. It is known that the maintenance of oral health in these situations depends not only on the viability of dental tissues, but also on the periodontal damage occurred and the emergency therapeutic procedures performed.
AIM: The purpose of this epidemiological retrospective study was to assess the periodontal involvement in traumatized teeth treated at the Piracicaba Dental School/,UNICAMP Dental Trauma Attendance Service (DTAS), during a period of 4 years.
METHODS: Clinical charts of patients (n=203) treated between 2006 and 2009 at DTAS were retrospectively analyzed.
RESULTS: A total of 295 traumatized teeth were assessed about history, type of dental trauma, and periodontal tissue damage detected during clinical and radiographic examination. Moreover, the treatment associated with periodontal damage resolution was also determined. Of the 295 traumatized teeth, 184 had periodontal damage (62.3%) and from this total, crown-root fractures with invasion of biological width were found in 42% of the cases, followed by bone injury (30%). Regarding the periodontal treatment performed, periodontal surgery to re-establish the biological width prevailed between procedures with 39% of the cases.
CONCLUSIONS: It could be concluded that Periodontics has an essential role in the multidisciplinary approach for the treatment of traumatized patients and that the conjunct work is important to re-establish the overall oral health.
Keywords: prevalence diagnosis, tooth fractures.
Introduction
The incidence of dental trauma in children and school-age young people has increased considerably over the years1-2. Epidemiological studies show a strong relationship between trauma occurrence and anatomic characteristics such as accentuated overjet and inadequate lip seal3-4. In addition to anatomic factors, the causes of the growing incidence of dental trauma in younger people may be associated with the practice of contact and radical sports, although automobile accidents and urban violence also figure in the prevalent level of dental trauma5.
Dental trauma usually involves damage to cementum, periodontal ligament,dentin, and pulp. Its severity may be classified according to the level of damage to the supporting tissues as well as to the type of fracture3. In this context, it is important to consider that the traumatic sequel may involve not only the dental structures but also their surrounding tissues6. It brings a necessity to adopt a multidisciplinary vision for the treatment planning with the goal of maintenance and re-establishment of oral health7. It is known that dental trauma, even in its mildest form, invariably injuries the periodontal ligament fibers2-3,8. Thus, correct diagnosis and treatment protocols focused on the re-establishment of the health of periodontal tissues become essential to the treatment of traumatized patients. However, there are few published studies that evaluate the role of Periodontics during diagnosis and attendance of traumatized teeth. The multidisciplinary involvement aims to correlate the clinical variables for each specialty, ensuring comprehensive care to the trauma patient.
In this context, the purpose of this epidemiological retrospective study was to assess the periodontal involvement in traumatized teeth, assisted by a dental trauma service for a period of 4 years.
Material and methods
The study design was approved by the Ethics Committee of Piracicaba Dental School, University of Campinas (Protocol #106/2007). Patient charts, containing the clinical and radiographic files of patients treated at the Piracicaba Dental School/,UNICAMP Dental Trauma Attendance Service (DTAS), between 2006 and 2009, were reviewed by an expert examiner.
Data Collection
Patient personal data including age, gender and medical history were collected. In addition, trauma history related to tooth affected, etiology and type of injury were analyzed. Related to clinical examination, tests of sensibility, palpation, mobility, vertical and horizontal percussion tests were performed.
Regarding periodontal involvement, signals and symptoms of the teeth such as gingival bleeding, disruption of periodontal ligament fibers, and presence of subgingival fractures were assessed. According to these signals, periodontal injury was categorized in: biologic width invasion, bone injury, gingival inflammation, and aesthetic impairment.
Signals of periodontal disease occurred before the moment of the trauma was excluded, according to wholemouth periodontal examination. Moreover, the entire periodontal treatment to these traumatized teeth was determined and performed by a periodontist.
Data were subjected to statistical analysis for Fisher's nonparametric samples (p<0.05).
Results
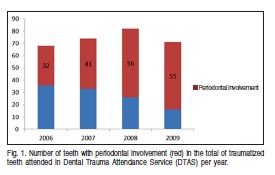
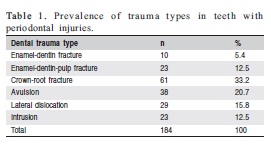
Two hundred and three patients (295 teeth) were treated at DTAS between 2006 and 2009. Of this total, 135 (66%) patients presented at least one tooth with periodontal involvement, which represents 184 (62.3%) teeth with association between dental trauma and periodontal injuries ( Figure 1). Patient age varied from 8 to 70 years old, and the majority of them were males (68%). The most common type of trauma was crown-root fracture (n=61 teeth, 33%); followed by avulsion (n=38 teeth, 20%), and lateral luxation (n=29 teeth, 15.8%) ( Table 1).
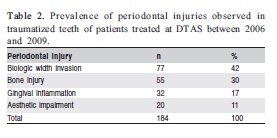
Regarding the periodontal involvement, biologic width invasion was the most common condition, which was observed in 77 teeth (42%). Bone injury was the second type of periodontal involvement, affecting 55 teeth (30%) ( Table 2).
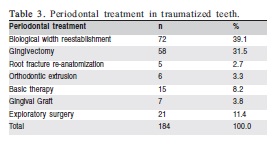
The treatment adopted in the majority of the cases was a periodontal surgery to re-establish the biologic width with adjunct of gingivectomy and osteotomy, performed in 39% of the cases. Although gingivectomy was a frequent procedure (52 cases), alternatives to treat subgingival crown root fracture such as orthodontic extrusion and fracture re-anatomization were also performed in 6% of the cases ( Table 3).
Discussion
Retrospective studies allow a clear view of the subject matter and demonstrate its most important aspects9-10. However, there is no study focusing on the role of Periodontics in attendance of a traumatized patient. Considering that most of the trauma promotes periodontal and pulpal damage, the information provided by epidemiological studies could be important in planning future approaches to the treatment of traumatized patients. In this retrospective study, most of the traumatized teeth (62.3%) were associated with a periodontal injury. The number of traumatized teeth follows an ascending order each year, which can be related to the disclosure of dental trauma services in schools of in Piracicaba and region2.
The most common trauma related to periodontal injuries was complex crown root fractures involving enamel, dentin, pulp and cement, with 61 teeth involved (33.2%). Periodontal injury was more related to biologic width invasion (n=77 teeth, 42%). This is probably due to the angle and direction of the impact in which the trauma is related that may cause a deeper destruction. When the biologic width is invaded, an inflammatory reaction occurs on the periodontium, which causes alveolar bone resorption in order to generate more space for new connective tissue. Consequently, a deepening gingival groove is opened which can lead to chronic inflammation11. The average of biologic width is established, as follows12: gingival sulcus: 0.69 mm; junctional epithelium: 0.97 mm; and connective tissue attachment: 1.07 mm. So, there is 2 to 3 mm of sound tooth structure coronal to the alveolar bone crest to the junctional epithelium and connective tissue attachment that can properly join the tooth. In these situations, the re-establishment of the biologic width with increased clinical crown may be performed through surgical crown lengthening procedures, surgical or orthodontic extrusion, each one when properly indicated6-7.
Surgical crown lengthening procedures are the most common technique that allows rehabilitation of the biologic width, especially in cases of caries, prosthetic preparations and invoices13. They are important for the rehabilitation of periodontal health and removal of irritation that might damage the periodontium. The millimeter that is needed from the bottom of the junctional epithelium to the tip of the alveolar bone is held responsible for the lack of inflammation and bone resorption, and as such the development of periodontitis14. In cases of dental trauma, these procedures are indicated when there is inadequate clinical crown for retention due to tooth fracture and root resorption within the cervical third of the root in teeth with adequate periodontal attachment; placement of sub gingival restorative margins; unequal, excessive or unaesthetic gingival levels for aesthetics; teeth with inadequate interocclusal space for proper restorative procedures due to supraeruption; and restorations which violate the biologic width15. Meantime, there are some contraindications of these techniques namely deep fracture requiring excessive bone removal; post-surgery unaesthetic outcomes; tooth with inadequate crownroot ratio (ideally 2:1 ratio is preferred); non-restorable teeth; teeth with increased risk of furcation involvement; unreasonable impairment of aesthetics; and unreasonable impairment of adjacent alveolar bone support14.
Considering dental trauma frequently involves anterior teeth in young individuals, who are highly associated with a severe overjet and an inadequate coverage lip16, aesthetic involvement should be taken into account. In these cases, as the aesthetics of the patient may be affected, surgical crown lengthening procedures are not indicated because of the risks of gingival recession13. Heithersay17 1973, said that to minimize gingival recession caused by gingivectomy associated with removal of bone, orthodontic extrusion (forced eruption) should be performed prior to surgery, mainly in fractures. It may be explained because this extrusive moving acts not only on the tooth but also on its oral support, gingival ligament fibers and alveolar bone, allowing a posterior osteotomy18. An example occurs when lateral luxation promotes bone break-up, needing a periodontal surgery in the location of the fracture for the re-establishment of biologic width. Periodontal grafts with bone or soft tissue may also be performed in order to have better aesthetic post-trauma, matching with the periodontal plastic surgery, which aims to improve the environment periodontal facilitation of hygiene and ensure appropriate aesthetics. Plastic surgery is used to reduce periodontal gingival recession, preservation and reconstruction of the alveolar, interdental papilla gain and to improve aesthetics, especially after avulsion and replantation, as well as intrusions5,10,19. Some of the contraindications to forced eruption are inadequate crownto-root ratio, lack of occlusal clearance for the required amount of eruption and any possible periodontal complications14.
Another periodontal treatment is the exploratory surgery, performed in cases where the fracture line is not radiographically visible. This is frequently held, especially in cases of fractures and oblique fractures of the crown and root. These conditions require periodontal access not only to establish the patient's oral health but also to allow the optimization of the placement of rubber sheet for absolute isolation, a fundamental procedure in endodontics. In some cases, such as oblique fractures of the teeth prior to biologic width invasion, a re-anatomization using diamond drill bits that return the correct spacing after an exploratory periodontal surgery helps exposing the fracture line. In these conditions, there is no need for gingivectomy or orthodontic extrusion20.
Since 2003, DTAS has treated traumatized patients with multidisciplinary care in the areas of periodontics, restorative dentistry and oral-maxillofacial surgery with a high-quality professional staff. This conjunct work favors integrated patient treatment, considering that support tissues are frequently affected when a dental trauma occurs, as can be seen in the present study. Thus, the improvement of health and full reestablishment of these patients may be achieved beginning with interdisciplinarity between endodontics and periodontology in treating dental trauma.
In view of the present results, it could be concluded that periodontal damage occurs frequently in dental trauma, and its treatment has an essential role in the multidisciplinary approach to re-establish overall oral health.
References
1. Kumar A, Bansal V, Veeresha KL, Sogi GM. Prevalence of traumatic dental injuries among 12- to 15-year-old schoolchildren in Ambala district, Haryana, India. Oral Health Prev Dent. 2011; 9: 301-5. [ Links ]
2. Souza-Filho FJ, Soares AJ, Gomes BPFA, Zaia AA, Ferraz, CCR, Almeida JFA. Evaluation of the traumatic dental injuries attended at the Traumatic Dental Center of Dental School of Piracicaba, Brazil. RGO. 2009; 14: 111-6. [ Links ]
3. Bonini GC, Bönecker M, Braga MM, Mendes FM. Combined effect of anterior malocclusion and inadequate lip coverage on dental trauma in primary teeth. Dent Traumatol. 2012 Feb 27. doi: 10.1111/j.1600-9657.2012.01117.x. [Epub ahead of print] [ Links ].
4. Borzabadi-Farahani A, Borzabadi-Farahani A, Eslamipour F. An investigation into the association between facial profile and maxillary incisor trauma, a clinical non-radiografic study. Dent Traumatol. 2010; 26: 311-6. [ Links ]
5. Stewart GB, Shields BJ, Fields S, Comstock RD, Smith GA. Consumer products and activities associated with dental injuries to children treated in United States emergency departments, 1990-2003. Dent Traumatol. 2009; 25: 399-405. [ Links ]
6. Eichelsbacher F, Denner W, Klaiber B, Schlagenhauf U. Periodontal status of teeth with crown-root fractures: results two years after adhesive fragment reattachment. J Clin Periodontol. 2009; 36: 905-11. [ Links ]
7. Poi WR, Cardoso LC, de Castro JC, Cintra LT, Gulinelli JL, de Lazari JA. Multidisciplinary treatment approach for crown fracture and crownroot fracture - a case report. Dent Traumatol. 2007; 23: 51-5. [ Links ]
8. Sharma D, Garg S, Sheoran N, Swami S, Singh G. Multidisciplinary approach to the rehabilitation of a tooth with two trauma episodes: systematic review and report of a case. Dent Traumatol. 2011; 27: 321-6. [ Links ]
9. Guedes OA, de Alencar AH, Lopes LG, Pécora JD, Estrela C. A retrospective study of traumatic dental injuries in a Brazilian dental urgency service. Braz Dent J. 2010; 21: 153-7. [ Links ]
10. Santos SE, Marchiori EC, Soares AJ, Asprino L, de Souza Filho FJ, de Moraes M, et al. A 9-year retrospective study of dental trauma in Piracicaba and neighboring regions in the State of São Paulo, Brazil. J Oral Maxillofac Surg. 2010; 68: 1826-32. [ Links ]
11. Eichelsbacher F, Denner W, Klaiber B, Schlagenhauf U. Periodontal status of teeth with crown-root fractures: results two years after adhesive fragment reattachment. J Clin Periodontol. 2009; 36: 905-11. [ Links ]
12. Shobha KS, Mahantesha, Seshan H, Mani R, Kranti K. Clinical evaluation of the biological width following surgical crown-lengthening procedure: A prospective study. J Indian Soc Periodontol. 2010; 14: 160-7. [ Links ]
13. Kina JR, Dos Santos PH, Kina EF, Suzuki TY, Dos Santos PL. Periodontal and prosthetic biologic considerations to restore biological width in posterior teeth. J Craniofac Surg. 2011; 22: 1913-6. [ Links ]
14. Nugala B, Kumar BS, Sahitya S, Krishna PM. Biologic width and its importance in periodontal and restorative dentistry. J Conserv Dent. 2012; 15: 12-7. [ Links ]
15. Jorgic-Srdjak K, Dragoo MR, Bosnjak A, Plancak D, Filipovic I, Lazic D. Periodontal and prosthetic aspect of biological width part II: Reconstruction of anatomy and function. Acta Stomatol Croat. 2000; 34: 441-4. [ Links ]
16. Gupta S, Kumar-Jindal S, Bansal M, Singla A. Prevalence of traumatic dental injuries and role of incisal overjet and inadequate lip coverage as risk factors among 4-15 years old government school children in Baddi-Barotiwala Area, Himachal Pradesh, India. Med Oral Patol Oral Cir Bucal. 2011; 16: e960-5. [ Links ]
17. Rotundo R, Bassarelli T, Pace E, Iachetti G, Mervelt J, Pini Prato G. Orthodontic treatment of periodontal defects. Part II: A systematic review on human and animal studies. Prog Orthod. 2011; 12: 45-52. [ Links ]
18. Barboza EP, Monte-Alto RF, Ferreira VF, Carvalho WR. Supracrestal gingival tissue measurements in healthy human periodontium. Int J Periodontics Restorative Dent. 2008; 28: 55-61. [ Links ]
19. Soares AJ, Gomes BPFA, Zaia AA, Ferraz CCR, Souza-Filho FJ. Relationship between clinical–radiographic evaluation and outcome of teeth replantation. Dental Traumatol. 2008; 24: 183-8.
20. Bate AL, Lerda F. Multidisciplinary approach to the treatment of an oblique crown-root fracture. Dent Traumatol. 2010; 26: 98-104. [ Links ]
 Correspondence:
Correspondence:
Adriana de Jesus Soares
Av. Doutor Nelson Noronha Gustavo Filho, 150,
CEP:13092-526, apto 112B, Edifício Alpha Park,
Bairro Vila Brandina, - Campinas, SP, Brasil
E-mail: ajsoares.endo@uol.com.br
Received for publication: May 08, 2012
Accepted: June 15, 2012













