Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.3 Piracicaba Jul./Set. 2012
ORIGINAL ARTICLE
Preliminary investigation to achieve patency of MB2 canal in maxillary molars
Tauby de Souza Coutinho-FilhoI; Eduardo Diogo Gurgel-FilhoII; Francisco José Souza-FilhoIII; Emmanuel João Nogueira Leal da SilvaIV
IDDS, MSc, PhD, Professor, State University of Rio de Janeiro, Endodontics Department, Rio de Janeiro, RJ, Brazil
IIDDS, MSc, PhD, Professor, University of Fortaleza, Department of Endodontics, Fortaleza, CE, Brazil
IIIDDS, MSc, PhD, Professor, State University of Campinas, Endodontics Division, Piracicaba, SP, Brazil
IVDDS, MSc, PhD, student, State University of Campinas, Endodontics Division, Piracicaba, SP, Brazil
ABSTRACT
AIM: To establish a preliminary investigation about the possibility to achieve patency of second mesiobuccal canal (MB2) in mesiobuccal roots of maxillary molars.
METHODS: Three hundred and five first maxillary molars were examined with direct vision and with magnification. The root canal configurations were classified according to the possibility to achieve patency in MB2 canals. Clearing technique was also performed to illustrate root canal anatomy and verify the presence of extra canals not identified with magnification.
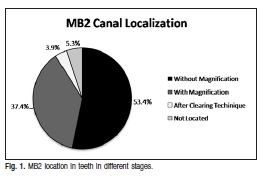
RESULTS: The prevalence of MB2 canals detected only with direct vision was 53.4% and the use of the surgical operating microscope increased rate detection to 90.7%. The clearing technique revealed the presence of MB2 canal in 12 more teeth (94.7%). In 49.1% of the localized MB2 canals, it was not possible to achieve patency.
CONCLUSIONS: The findings of the presented study revealed that it was only possible to achieve patency in 50.9% of the MB2 canals, showing that achieve patency in the MB2 canal is much more challenging than locating them.
Keywords: maxillary first molar, mesiobuccal second canal, operating microscope.
Introduction
The success of endodontic treatment depends on the location, cleaning, shaping and sealing of the root canal system1. The knowledge of root canal system anatomy is essential to determine the success of endodontic therapy. Anatomical studies are of great importance to aid the understanding of the internal morphology and anatomical variations of the root canal system2-4.
The permanent maxillary first molar has one of the most complex root and canal anatomies. This morphology has been studied and it is accepted that the mesial root often has more than one canal1-2,5-6. In the literature, the mesiobuccal (MB) root of the maxillary first molar has generated more research and clinical investigation than any other root7. The incidence of second mesiobuccal canals (MB2) has been reported in a range of between 33% and 96%1-2,5-10. However, the clinical detection of MB2 in maxillary molars has been lower than that of laboratorybased reports and this canal could be detected in less than 40% of maxillary first molars11-12.
The use of the surgical operating microscope (SOM) facilitates detectionand negotiation of more MB2 canals in both in vitro and clinical studies13-15. A high incidence of MB2 canals was reported in the mesiobuccal roots of the first maxillary molars ex vivo, and it was also demonstrated that the use of the operating microscope increased the ability of the dental clinician to locate the MB213.
Although the literature shows a high incidence of MB2 canal, Sempira & Hartwell16 reported that only 33% of maxillary first molars had a negotiable MB2 canal, as determined by use of SOM in vivo. The most important causes of non-negotiable MB2 canal location are diffuse calcification, pulp stones and debris17. Given this low incidence of negotiable MB2 canals, the aim of this study was to establish a preliminary investigation about the possibility to achieve of MB2 canals in mesiobuccal roots.
Material and methods
A total of 305 extracted human maxillary molars that had been stored in distilled water were used in this study. The floor of the pulp chamber was then explored in order to locate the MB1 and MB2 and to verify the possibility to achieve patency in MB2 canals.
Initially the canals were located with direct vision. The canal was negotiated and confirmed by insertion of a size 08 and 10 K-file (Dentsply-Maillefer, Ballaigues, Switzerland). Further efforts to locate canals were carried out under magnification using the SOM (x20, DFV, MC-M 1232; São Paulo, SP, Brazil) and the canals were negotiated with a size 08 and 10 K-file. After instrumentation a radiograph was performed.
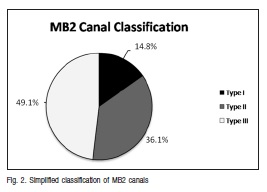
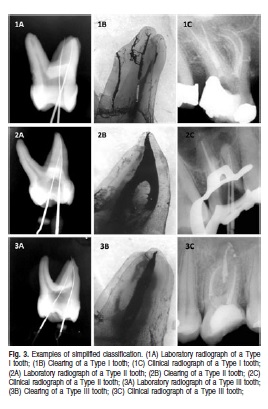
The root canal configuration in each root was determined by using a simplified classification of root canal configurations. Type I being two separate and distinct canals from pulp chamber to the apex, Type II being two canals leaving the pulp chamber and merging to form a single canal short to the apex, and Type III being interrupted access with no canal or roots with just one canal. Type I and Type II were classified as possible to achieve patency and Type III was the canal that was not accessible to the apex.
After this, to illustrate root canal configuration, teeth were prepared using a clearing technique. Teeth were immersed in Indian ink (Pelikan, São Paulo, SP, Brazil) under 600-mmHg vacuums for 40 min and then kept for 10 days in an incubator at 37ºC. A final wash with tap water to remove excess ink was performed. The teeth were demineralized with a 5% hydrochloric acid solution for 3 days, dehydrated with ascending grades of alcohol, immersed in methyl salicylate and rendered transparent18.
Results
Under direct vision, the MB2 canal was located in 163 teeth (53.4%). With the use of the SOM, the MB2 canal was located in 114 additional teeth, totalizing 277 teeth (90.7%). The clearing technique disclosed the presence of a MB2 canal in 12 more teeth, totalizing 289 teeth (94.7%), while 16 teeth had a single canal in the mesiobuccal root (5.3%). This prevalence can be seen in Figure 1.
A total of 45 canals were classified as Type I canals (14.8%), 110 classified as Type II canals (36.1%), 150 as Type III canals (49.1%). These results can be seen in Figure 2 and the images and examples of the classification are found in Figure 3. Patency was achieved in only 50.9% of the localized MB2 canals.
Discussion
Successful endodontic treatment demands adequate cleaning, shaping and filling of the root canal system. For this, clinicians must have comprehensive knowledge about root canal morphology. Anatomical variations may be present in teeth subjected to endodontic treatment. In that perspective, the incidence of the MB2 canal in the mesiobuccal root of the maxillary first molar is always a matter of interest to the endodontic community13. Failure to detect and treat the second MB2 canal system will result in a decreased longterm prognosis2.
Previous studies showed that the use of SOM increased detection of MB2 canals from 51 to 81%13,19-20. A total MB2 detection rate of 93.3% was observed when cone bean computed tomography (CBCT) was used in first molars21.
The findings of the present study observed that the prevalence of MB2 canals detected with direct vision was 53.4% and the association with the SOM increased rate detection to 90.8%. This can be justified by the fact that the higher magnification and illumination can be useful for access cavity preparation, instrumentation and filling22-23. It can improve the clinician's view of the complexity of the root canal anatomy and aid in the location of additional canals, fins or ribbons. Thus, the use of SOM to detect the ML canal orifice of maxillary first and second molars may enhance the success of endodontic procedures13.
Although there are several reports demonstrating the efficacy of the SOM in locating MB2 canals, Sempira and Hartwell16 reported that 33% of maxillary first molars had a negotiable MB2 canal as determined by use of SOM in vivo. In this study, the accessibility of located MB2 canals was evaluated. Only 14.8% of the tooth had two separate and distinct canals from pulp chamber to the apex. In the remaining cases occurs the intersection of MB2 with the MB canal (36.1%) or its unexpected ending at 3 or 4 mm of entry and roots with just one canal (49.1%). This unexpected ending may be because of calcified MB2 canals that prevented the full instrumentation of the canal. Previous research suggests that non-negotiable factors of MB2 canal location were diffuse calcification, pulp stone debris and tortuous pathway17,24-25. The MB2 canal can be challenging to treat because it might share an orifice with MB1 or can be harbored within, or just apical to, that of the MB1 canal. In cases of union with the MB canal, treatment is possible since it passes the entrance angle to the MB. Clinically, it can be seen the impossibility of instrument penetration on both canals simultaneously. It becomes evident when a file is introduced into one canal and the other does not go down and vice versa.
The most complex cases are those where the penetration of the files is stopped suddenly, usually at 3 or 4 mm from its entrance. In the present study, this type of canal was observed in 49.1% of maxillary first molars in MB2 canals. The patency was achieved in only 50.9% of the localized MB2 canals. This prevalence is much lower than the total number of MB2 canal orifices (94.7%). Previous reports, have also shown that the accessibility of located MB2 canals orifices is much lower than the total number of these canals16,26. Neaverth et al.27 suggested that a modified access preparation and countersinking techniques may help in the MB2 canals treatment. They also reported that with these techniques they were able to treat 77.2% of MB2 canals in maxillary first molars. However, even with these highs rates of treated canals, several MB2 canals could not be instrumented. This large number of canals left untreated in several studies demonstrates the need to emphasize de frequency and clinical significance of these canals.
Achieving patency of MB2 canal is much more challenging than locating them. In the endodontic treatment of first molars, the MB2 canal occurs on an average frequency of 94.7%. It should be possible to perform its treatment at the same frequency, but this does not occur. In the present study, the cleaning technique revealed that the complex anatomy and the tortuous pathway of the root canal system justify the difficulties in penetrating the entire length of the MB canal.
Based on the findings of the present study, it can be concluded that it was only possible to achieve patency in 50.9% on MB2 canals, showing that achieve patency in the MB2 canal is much more challenging than locating them.
References
1. Pattanshetti N, Gaidhene M, Kandari AM. Root canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait populationa clinical study. Int Endod J. 2008; 41: 755-62. [ Links ]
2. Weine FS, Healey HJ, Gerstein H, Evanson L. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surg Oral Med Oral Pathol. 1969; 28: 419-25. [ Links ]
3. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984; 58: 589-99. [ Links ]
4. Friedman S. Prognosis of initial endodontic therapy. Endod Top. 2002; 2: 59-88. [ Links ]
5. Weng XL, Yu SB, Zhao SL, Wang HG, Mu T, Tang RT, Zhou XD. Root canal morphology of permanent maxillary teeth in the Han nationality in Chinese Guanzhong area: e new modified root canal staining technique. J Endod. 2009; 35: 651-6. [ Links ]
6. Blattner TC, George N, Lee CC, Kumar V, Yelton CDJ. Efficacy of cone-beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: a pilot study. J Endod. 2010; 36: 867-70. [ Links ]
7. Cleghorn B, Christie W, Dong CCS. Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod. 2006; 32: 813-21. [ Links ]
8. Kobayashi C, Sunada I. Root canal morphology and its possibility for penetration. Part 3.Maxillary molar. Jap J Cons Dent. 1987; 30: 1674-83. [ Links ]
9. Carvalho MCC, Zuolo ML. Orifice location with a microscope. J Endod. 2000; 26: 532-4. [ Links ]
10. Imura N, Hata G, Toda T, Otani SM, Fagundes MIRC. Two canals in mesiobuccal roots of maxillary molars. J Endod. 1998; 38: 410-4. [ Links ]
11. Weller RN, Hartwell GR. The impact of improved access and searching techniques on detection of the mesiolingual canal in maxillary molars. J Endod. 1989; 15: 82-3. [ Links ]
12. Wasti F, Shearer AC, Wilson NH. Root canal systems of the mandibular and maxillary first permanent molar teeth of south Asian Pakistanis. Int Endod J. 2001; 34: 263-6. [ Links ]
13. Coutinho-Filho T, Cerda RSL, Gurgel-Filho ED, De-Deus G, Magalhães KM. The influence of the surgical operating microscope in locating the mesiolingual canal orifice: a laboratory analysis. Braz Oral Res. 2006; 20: 59-63. [ Links ]
14. Yoshioka T, Kikuchi I, Fukumoto Y, Kobayashi C, Suda H. Detection of the second mesiobuccal canal in mesiobuccal roots of maxillary molar teeth ex vivo. Int Endod J. 2005; 38: 124-8. [ Links ]
15. Wolcott J, Ishley D, Kennedy W, Johnson S, Minnich S,Meyers J. A 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J Endod. 2005; 31: 262-4. [ Links ]
16. Sempira HN, Hartwell GR. Frequency of second mesiobuccal canals in maxillary molars as determined by use of an operative microscope: a clinical study. J Endod. 2000; 26: 673-4. [ Links ]
17. Ibbarrola JL, Knowles KI, Ludlow MO, McKinley IB Jr. Factors affecting the negotiability of second mesiobuccal canals in maxillary molars. J Endod. 1997; 38: 236-8. [ Links ]
18. Almeida JF, Gomes BP, Ferraz CC, Souza-Filho FJ, Zaia AA. Filling of artificial lateral canals and microleakage and flow of five endodontic sealers. Int Endod J 2007; 40: 692-9. [ Links ]
19. Yoshioka T, Kobayashi C, Suda H. High detection rate of root canal orifices under microscope. J Endod. 2002; 28: 452-3. [ Links ]
20. Alaçam T, Tinaz AC, Genç O, Kayaoglu G. Second mesiobuccal canal in maxillary first molars using microscope and ultrasonics. Aust Endod J. 2008; 34: 106-9. [ Links ]
21. Bauman R, Scarfe W, Clark S, Morelli J, Scheetz J, Farman A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int Endod J. 2011; 44: 752-8. [ Links ]
22. Görduysus MO, Görduysus M, Friedman S. Operative microscope improves negotiation of second mesiobuccal canals in maxillary molars. J Endod. 2001; 27: 683-6. [ Links ]
23. Kontakiotis EG, Palamidakis FD, Farmakis ET, Tzanetakis GN. Comparison of isthmus detection methods in the apical third of mesial roots of maxillary and mandibular firts molars: macroscopic observation versus operating microscope. Braz Dent J. 2010; 21: 428-31. [ Links ]
24. Constante IG, Davidowicz H, Barletta FB, Moura AA. Location and angulation of curvatures of mesiobuccal canals of mandibular molars debrided by three endodontic techniques. Braz Oral Res. 2007; 21: 22-8. [ Links ]
25. Estrela C, Bueno MR, Sousa-Neto MD, Pécora JD. Method for determination of root curvature radius using cone-beam computed tomography images. Braz Dent J. 2008; 19: 114-8. [ Links ]
26. Tuncer AK, Haznedaroglu F, Sert S. The location and accessibility of the second mesiobuccal canal in maxillary first molar. Eur J Dent. 2010; 4: 12-6. [ Links ]
27. Neaverth EJ, Kotler LM, Kaltenbach RF. Clinical investigation of in vivo endodontically treated maxillary first molars. J Endod. 1987; 13: 506-12. [ Links ]
 Correspondence:
Correspondence:
Tauby de Souza Coutinho-Filho
Rua Santo Afonso 110, Sala 707, Tijuca,
Rio de Janeiro, RJ, Brasil
CEP: 20511-170
E-mail: taubycf@hotmail.com
Received for publication: February 28, 2012
Accepted: May 17, 2012













