Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.3 Piracicaba Jul./Set. 2012
ORIGINAL ARTICLE
Gender as risk factor for mouth breathing and other harmful oral habits in preschoolers
Lara Jansiski MottaI; Thays Almeida AlfayaII; Ana lúcia Ferreira MarangoniIII; Raquel Agnelli Mesquita-FerrariIV; Kristianne Porta Santos FernandesIV; Sandra Kalil BussadoriIV
IPhD, Professor of Pediatric Dentistry of Nove de Julho University (UNINOVE), São Paulo, SP, Brazil
IIDDS, Graduate Student of Dental Clinic, Graduate Program of Federal Fluminense University (UFF), Niterói, RJ, Brazil
IIIMsc, Private practice, São Paulo, SP, Brazil
IVPhD, Professor of Rehabilitation Sciences, Graduate Program, Nove de Julho University (UNINOVE), São Paulo, SP, Brazil
ABSTRACT
AIM: To analyze associations between the mouth-breathing pattern and other harmful oral habits among preschoolers.
METHODS: An observational, cross-sectional study was carried out involving 198 children from 3 to five 5 of age. A questionnaire, clinical evaluation and specific tests (mirror and water tests) were used for confirmation of the mouth-breathing pattern.
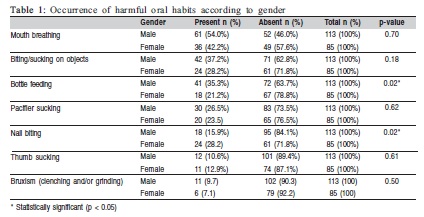
RESULTS: Mean age of the participants was 4.13 ± 0.8 years and 57.1% were male. A total of 87.4% exhibited one or more harmful oral habits. Harmful habits were more common in the male gender (61.8%); this association was statistically significant (p<0.001). Mouth breathing was the most prevalent habit (49%), followed by biting/sucking on objects (33.3%). Regarding gender, statistically significant associations were found for bottle feeding (p=0.02) and nail biting (p=0.02). Mouth breathing was associated with biting on object (p=0.00), pacifier use (p=0.02) and thumb sucking (p=0.00).
CONCLUSIONS: The results of the present study suggest that mouth breathing is significantly associated with biting/sucking on objects, pacifier use and thumb sucking in preschoolers and that the occurrence of harmful oral habits is more prevalent among the male gender. Early diagnosis and intervention should be established in order to avoid future consequences involving the orofacial region.
Keywords: mouth breathing, habits, child.
Introduction
Habit is defined as "a custom or practice acquired by the frequent repetition of a single act that begins in a conscious manner and subsequently becomes unconscious." Oral habits are classified as physiological and non-physiological. Physiological habits include nasal breathing, chewing, speaking and swallowing. Non-physiological habits are often called harmful or parafunctional and include thumb sucking, pacifier sucking, bottle feeding, the tongue placing pressure on the teeth and the mouth-breathing pattern1.
Particular habits may involve emotional factors2-3, such as anxiety4 and sensitivity to stress5. With regard to age, harmful oral habits are common among children and there is a lesser frequency among adolescents6. Such habits have a direct influence over quality of life7 and can affect the stomatognathic system, leading to an imbalance between external and internal muscle forces1. This occurswhen physiological tolerance is surpassed (response to the action performed), leading to alterations in the dentition, musculature and temporomandibular joint8. Temporomandibular disorder may be caused by the intensity of the action of a particular harmful habit9-11. Bone malformations may also result from the duration and frequency of harmful habits1.
As such habits require a multidisciplinary approach to provide integral care to pediatric patients, the aim of the present study was to analyze associations between the mouth-breathing pattern and other harmful habits in children aged 3 to 5 years.
Material and methods
An observational, cross-sectional study was carried out involving students enrolled in public preschools in the city of São Roque, state of São Paulo, Brazil. Convenience sampling was employed, with the evaluation of all children enrolled in the schools between three and five years of age in 2008. All parents/guardians received information regarding the objectives of the study and signed a statement of informed consent in compliance with Resolution 196/96 of the Brazilian National Health Council. This study received approval from the local Human Research Ethics Committee under process #82622/08.
A questionnaire containing objective, closed-ended questions was used to gather information on age, gender and the presence of harmful oral habits. This questionnaire was filled out by the parents/guardians with no time constraint. The aim of the questionnaire was to investigate the presence/absence of harmful habits and associations between the mouth-breathing pattern and nail biting, biting/sucking on objects, thumb sucking, pacifier sucking, bottle feeding and bruxism (teeth clenching/grinding). Children using systemic medications for treatment of the airway problems (colds and influenza) and those with orthodontic or orthopedic appliances of the maxillae were excluded from the study.
Besides the questionnaire, a clinical evaluation and specific tests (mirror and water tests) were performed by a single examiner who had undergone a training process and was supervised by an otolaryngologist for the confirmation of the mouth-breathing pattern. The clinical evaluation involved the determination of the presence/absence of the following signs: long face, drooping eyes, dark circles under the eyes, thin upper lip, dry lips, hypotonic lips, inverted lower lip, narrow nostrils, high-arched palate, inadequate lip seal and anterior open bite. The mirror test consisted of placing a two-sided mirror below the child's nostrils and observing the formation of vapor condensation stemming from respiration. Fogging on the upper part of the mirror indicates nasal breathing and fogging on the lower part or both parts indicates mouth breathing9. The water test was performed after the mirror test. For such, the child held a small amount of water in his/her mouth and maintained the lips in contact without swallowing for three minutes, during which time the effort of the lip commissure was observed. Children who were unable to maintain the lips in contact for three minutes were considered mouth breathers12.
Data analysis was performed using the SPSS 17 program (IBM Corp., Chicago, IL, USA) and involved the chi-squared (÷2) test and Fisher's exact test, with the level of significance set to 5% (p<0.05).
Results
The sample was made up of 198 children between three and five years of age. Mean age was 4.13 ± 0.8 years and 57.1% were male. A total of 87.4% (n = 173) exhibited one or more harmful oral habits: 29.3% (n = 58) had one habit, 30.8% (n = 61) had two habits, 18.2% (n = 36) had three habits and 9.1% (n = 18) had four habits.
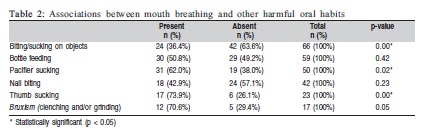
Harmful habits were more common in the male gender (61.8%; n = 107) than the female gender (38.2%; n = 66). The association between the male gender and harmful habits was statistically significant (x2 = 12.773, p<0.001). Regarding the type of habit, the mouth-breathing pattern was the most prevalent (49%; n = 97), following by biting/ sucking on objects (33.3%; n = 66). Gender was significantly associated with bottle feeding and nail biting (Table 1). The mouth-breathing pattern was significantly associated with biting/sucking on objects, bottle feeding and thumb sucking
(Table 2).
Discussion
The results of the present study suggest that the mouthbreathing pattern is significantly associated with biting/sucking on objects, bottle feeding and thumb sucking and that the occurrence of harmful oral habits is more prevalent among the male gender.
Mouth breathing is a potential etiological factor for the alterations to the occlusion and normal facial growth. When combined with other parafunctional habits, the harm to the stomatognathic system is even greater. According to Cattoni et al. (2007)13, children with this habit exhibit pathologic adaptations regarding postural and morphological characteristics of the stomatognathic system. Thus, the early diagnosis of mouth breathing and proper intervention are suggested to avoid the emergence of orofacial abnormalities.
A number of acute and chronic conditions can lead to the mouth breathing pattern. Acute conditions included infectious processes and the introduction of foreign bodies. Chronic conditions include choanal atresia, adenoid hypertrophy, chronic tonsil hypertrophy, nasal septum deformity, nose fracture, allergic rhinitis (and respective medication), polyps, tumors and narrow nasal cavities14. In order to avoid bias in the results of the present investigation, children in use of systemic medication for the treatment of the airways and those with orthodontic or orthopedic appliances on the maxillae were excluded from the study. However, non-reported chronic conditions could have led to the mouth-breathing pattern in the children evaluated. Considering the aim of the study, the researchers did not seek to establish the reason for the habit, but rather its presence or absence.
The present study found a high percentage of harmful habits among the children evaluated. Similar findings are reported in the literature6,15-16. Emodi-Perlman et al. (2012)6 evaluated parafunctional habits in children in the primary and mixed dentition phases, reporting high prevalence rates for biting/sucking on objects and nail biting. The authors point out that stressful events in life are related to an increase in the number of harmful oral habits in children.
Bruxism was the least prevalent habit in the present study and was not associated with mouth breathing. While few studies have been carried out on this subject, Serra-Negra et al. (2010)17 report a high prevalence rate of this habit (33.0%). Carra et al. (2011)15 assessed the prevalence and risk factors of sleep-related bruxism and wake-time tooth clenching in a population ranging from seven to 17 years of age who sought orthodontic treatment. The results indicate that sleep-time and wake-time parafunctions are often associated with signs and symptoms of temporomandibular disorder, sleep problems and behavioral problems and therefore merit attention during dental evaluations.
One limitation of the present study was the failure to evaluate the presence of snoring, which is reported to be common in children. The repercussions of snoring are mainly related to cognitive development18-19 and high blood pressure20. Moreover, snoring may be common in individuals with the habit of bruxism21.
In general, the presence of such habits can compromise the stomatognathic system1,8-11. A study involving both children and adults sought to determine associations between parafunctional habits and the emergence of temporomandibular disorder through the evaluation of the frequency of diurnal bruxism and nail biting, the results of which demonstrated that the female gender was at a significant risk for myofascial pain10. Another study with the same line of reasoning found that parafunctional habits were associated to important symptoms of orofacial pain, indicating that such habits are risk factors for temporomandibular disorder. A study with a 20-year follow up found that parafunctional habits can be persistent, as Angle class II malocclusion and tooth wear in childhood were predictors of increased tooth wear in adulthood22. These findings underscore the importance of the early diagnosis of harmful oral habits and proper intervention in order to avoid future consequences involving the orofacial region.
References
1. Agurto PV, Diaz RM, Cadiz OD, Bobenrieth FK. Oral bad habits frequency and its association with dentomaxilar abnormal development, in children three to six year old in Santiago Oriente. Rev Chil Pediatr. 1999; 70: 470-82. [ Links ]
2. Castelo PM, Barbosa TS, Gaviao MB. Quality of life evaluation of children with sleep bruxism. BMC Oral Health. 2010; 10: 16. [ Links ]
3. Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009; 23: 153-66. [ Links ]
4. Restrepo CC, Medina I, Patino I. Effect of occlusal splints on the temporomandibular disorders, dental wear and anxiety of bruxist children. Eur J Dent. 2011; 5: 441-50. [ Links ]
5. Serra-Negra JM, Paiva SM, Flores-Mendoza CE, Ramos-Jorge ML, Pordeus IA. Association among stress, personality traits, and sleep bruxism in children. Pediatr Dent. 2012; 34: 30-4. [ Links ]
6. Emodi-Perlman A, Eli I, Friedman-Rubin P, Goldsmith C, Reiter S, Winocur E. Bruxism, oral parafunctions, anamnestic and clinical findings of temporomandibular disorders in children. J Oral Rehabil. 2012; 39: 126-35. [ Links ]
7. Simoes-Zenari M, Bitar ML. Factors associated to bruxism in children from 4-6 years. Pro Fono. 2010; 22: 465-72. [ Links ]
8. Okeson JP. Management of temporomandibular disorders and occlusion.6. ed. Saint Louis: Mosby; 2008. [ Links ]
9. Cortese SG, Biondi AM. Relationship between dysfunctions and parafunctional oral habits, and temporomandibular disorders in children and teenagers. Arch Argent Pediatr. 2009; 107: 134-8. [ Links ]
10. Michelotti A, Cioffi I, Festa P, Scala G, Farella M. Oral parafunctions as risk factors for diagnostic TMD subgroups. J Oral Rehabil. 2010; 37: 157-62. [ Links ]
11. Sari S, Sonmez H. Investigation of the relationship between oral parafunctions and temporomandibular joint dysfunction in Turkish children with mixed and permanent dentition. J Oral Rehabil. 2002; 29: 108-12. [ Links ]
12. Jorge EP, Gandini Júnior LG, Santos-Pinto A, Guariza Filho O, Castro ABBAT. Evaluation of the effect of rapid maxillary expansion on the respiratory pattern using active anterior rhinomanometry: case report and description of the technique. Dental Press J Orthod. 2010; 15: 71-9. [ Links ]
13. Cattoni DM, Fernandes FD, Di Francesco RC, Latorre Mdo R. Characteristics of the stomatognathic system of mouth breathing children: anthroposcopic approach. Pro Fono. 2007; 19: 347-51. [ Links ]
14. Motonaga SM, Berte LC, Anselmo-Lima WT. Mouth Breathing: Causes and Changes of the Stomatolognathic System. Braz J Otorhinolaryngol. 2000; 66: 373-9. [ Links ]
15. Carra MC, Huynh N, Morton P, Rompre PH, Papadakis A, Remise C, et al. Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population. Eur J Oral Sci. 2011; 119: 386-94. [ Links ]
16. Medeiros PKM, Cavalcanti AL, Bezerra PM, Moura C. Malocclusions, breast feeding and deleterious buccal habits preschool children: an association study. Pes Bras Odontoped Clin Integr. 2005; 5: 267-74. [ Links ]
17. Serra-Negra JM, Paiva SM, Seabra AP, Dorella C, Lemos BF, Pordeus IA. Prevalence of sleep bruxism in a group of Brazilian schoolchildren. Eur Arch Paediatr Dent. 2010; 11: 192-5. [ Links ]
18. Piteo AM, Kennedy JD, Roberts RM, Martin AJ, Nettelbeck T, Kohler MJ, et al. Snoring and cognitive development in infancy. Sleep Med. 2011; 12: 981-7. [ Links ]
19. Piteo AM, Lushington K, Roberts RM, van den Heuvel CJ, Nettelbeck T, Kohler MJ, et al. Prevalence of snoring and associated factors in infancy. Sleep Med. 2011; 12: 787-92. [ Links ]
20. Li AM, Au CT, Ho C, Fok TF, Wing YK. Blood pressure is elevated in children with primary snoring. J Pediatr. 2009; 155: 362-8. [ Links ]
21. Ng DK, Kwok KL, Poon G, Chau KW, 2002. Habitual snoring and sleep bruxism in a paediatric outpatient population in Hong Kong. Singapore Med J. 2001; 43: 554-6. [ Links ]
22. Carlsson GE, Egermark I, Magnusson T. Predictors of bruxism, other oral parafunctions, and tooth wear over a 20-year follow-up period. J Orofac Pain. 2003; 17: 50-7. [ Links ]
 Correspondence:
Correspondence:
Thays Almeida Alfaya
Rua Doutor Calandrine, 235 A - CEP: 24755-160
São Gonçalo, RJ, Brasil
E-mail: thalfaya@gmail.com
Received for publication: May 16, 2012
Accepted: August 02, 2012













