Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.11 no.4 Piracicaba Out./Dez. 2012
ORIGINAL ARTICLE
Fracture resistance of over-flared root canals filled with MTA and resin-based material: an in vitro study
Salma B. AbdoI; Sam'an Malik MasudiII; Norhayati LuddinIII; Adam HusienIV; Mohd Fadhli KhamisV
IBDS, MSc, PhD Student, Department of Restorative Dentistry, School of Dental Sciences, University Sains Malaysia, Malaysia
IIDDS, MS, School of Dental Sciences, Department of Restorative Dentistry, University Sains Malaysia, Malaysia
IIIBDS, Department of Restorative Dentistry, School of Dental Sciences, University Sains Malaysia, Malaysia
IVBDS, Department of Restorative Dentistry, School of Dental Sciences, University Sains Malaysia, Malaysia
VBDS, PhD, Department of Craniofacial Sciences & Oral Biology, School of Dental Sciences, University Sains Malaysia, Malaysia
ABSTRACT
AIM: To measure the fracture resistance of over-flared roots filled with a variety of materials (gutta-percha-nano HA, resilon-epiphany, composite and mineral trioxide aggregate - MTA) using the Instron machine test and micro-computed tomography (Micro CT) Scan. In addition, scanning electron microscopy (SEM) images were used to illustrate the type of fracture patterns of the specimens.
METHODS: One hundred and twenty extracted human mandibular singlerooted premolars were selected. A total of 105 out of the selected teeth were prepared to the working length and over-flared, leaving the apical 5 mm undisturbed. Fifteen samples had no treatment and were used as a positive control group (Group +ve). The 105 test teeth were further divided into 7 groups of 15 samples each. One of the 7 groups was designated as negative control (Group -ve) where teeth were over prepared and left without obturation. Remaining groups were filled with gutta-percha-nanoHA (Group1), gutta-percha-nano HA+composite (Group 2), gutta-percha-nano HA+MTA (Group 3), resilon-epiphany (Group 4), resilon-epiphany+composite (Group 5), and resilon-epiphany+MTA (Group 6). Fracture resistance of all samples was measured using the Instron testing machine. Three samples from each group had the depth of their fracture line measured by Micro CT Scan, and 2 samples from each group had their fracture pattern illustrated using SEM.
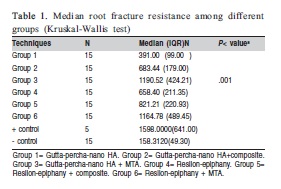
RESULTS: The highest fracture resistance was observed in Group +ve, followed by Groups 3, 6, 5, 2, 4, 1, and Group -ve, with values (in N) of: 1598 (641.0), 1190.5(424.2), 1164.7 (489.4), 821.2 (220.9), 683.4(179), 658.4 (211.3), 658.4 (99.0), 158.3(49.3), respectively. Statistical analysis for root fracture resistance showed highly significant difference between all groups with p value < 001.
CONCLUSIONS: Micro CT Scan and SEM analysis indicated the ability of MTA to withstand vertical force.
Keywords: instron machine, scanning electron microscopy, micro CT scan, mineral trioxide aggregate.
Introduction
It has been postulated that endodontic treatment results in reduction of fracture strength of teeth1. Brittleness of the dentin in the endodontically treatedteeth has been attributed to dehydration and loss of collagen cross-linking2. However, more recent studies concluded that neither dehydration nor endodontic treatment caused degradation of the physical or mechanical properties of the dentin3-7. One of the aims of root canal filling is to reinforce the dentin and increase the fracture resistance8. Other authors have suggested that filling the coronal and radicular lost tooth structure with bonded restorative materials, such as glass ionomer cement or composite resin, could reinforce the compromised teeth9-12. These bonding materials have also been examined for use as root canal filling materials but were disregarded due to problems in working properties and lack of hermetic seal resulting in leakage13. Mineral trioxide aggregate (MTA) is a fine biocompatible hydrophilic material that hardens in the presence of moisture or blood. MTA has been successfully used for root-end fillings, perforation repairs, pulp capping, pulpotomy and apexification treatment14-16. The fracture resistance of the tooth structure following use of MTA as an apical barrier has been investigated in teeth with open apices17-18. Results indicated that teeth treated with MTA had significantly more resistance to fracture as compared with those filled with calcium hydroxide (CH)18. However, thus far, use of MTA as a root filling material to reinforce weakened root structure has not been investigated19.
The aim of this study was to measure the fracture resistance of over-flared root canals filled with different materials (gutta-percha-nano HA, resilon-epiphany, composite and MTA).
Material and methods
One hundred and twenty freshly extracted single-rooted intact human mandibular premolars were selected for this study. Selected teeth exhibited no fracture lines as determined by examination under a dental microscope (Motic Digital Microscope, France) at x25 magnification level. Following extraction, teeth were stored in distilled water at room temperature. Fifteen out of 120 sample teeth had no treatment and were used as a positive control group (Group +ve). The remaining 105 teeth were assigned to test groups and prepared based on the following sequence:
• Teeth were sectioned from the cementoenamel junction using a high speed diamond bur.
•The working length was established 1 mm short of the apical foramen using a size 15, K file (Dentsply Maillefer, Ballaigues, Switzerland).
• All root canals were instrumented to an apical size of 30, taper 0.06 using rotary ProFile system (Dentsply Tulsa Dental Specialties, Tulsa, OK, USA), following steps of crowndown technique and intermittent irrigation with 5.25% sodium hypochlorite (NaOCl)
• Subsequent to the instrumentation, smear layer was removed from all canals using 10 mL of 17% EDTA solution followed by 10 mL of NaOCl.
• Gates Glidden size 6 drills was used to the depth of 10 mm, leaving untouched the apical 5 mm.
• Further widening of the coronal 5 mm of each canal was done by using a diamond bur with a coolant system.
• After finishing the preparation, samples were further irrigated with 10 mL of distilled water and dried using paper points.
The 105 prepared test teeth were further sub-divided into 7 groups of 15 samples each. One of the 7 groups was designated as negative control (Group -ve) where teeth were prepared as above and left without obturation. The remaining 6 groups were filled as follows:
Group 1 (n=15): Obturation was done with .06 tapered gutta-percha master points (Diadent, Chongju, Korea), dipped in nano HA sealer (a new sealer has been introduced by the school of Dental Sciences, Universiti Sains Malaysia, Malaysia, known as Nano-Hydroxyapatite (Nano-HA) sealer. The nano HA crystals which ranging from 40-60 nm in sizes were synthesized by wet chemical method by using CH and phosphoric acid (H3PO3) as Ca and P precursors, respectively.
Lateral compaction was performed using medium-fine gutta-percha accessory cones coated slightly with nano HA and appropriate finger spreaders (Dentsply Tulsa Dental Specialties).
Group 2 (n=15): The apical 5 mm of root canals were filled with gutta-percha and nano HA. Subsequently, the root canals were etched for 20 s with 37% phosphoric acid etchant (Superetch, SDI, Australia), rinsed, and dried. A dentin/enamel adhesive system (Stae, SDI, Australia) was placed inside the root canals using a Microbrush (Microbrush, Inc. USA) applicator and light cured for 10 s. A light-cured composite (3M Filter SupremeXT, Germany), was extruded into the root canals. Light-transmitting, size 3 plastic posts (Luminex post Dentatus, USA) were coated with Vaseline then centered and fully seated into the canals. The lightcuring probe was placed directly over the Luminex post and the entire complex was light-cured multidirectionally for 2 min. After curing, the Luminex post was removed using a hemostat and the space created by the post was filled with gutta-percha/nano HA.
Group 3(n=15): The apical 5 mm was filled with gutta-percha and nano HA. MTA (ProRoot, Dentsply Tulsa Dental Specialties) was mixed with sterile water to attain a grainy, sandy mixture. MTA mixture was placed in the canals using a Messing gun. Then, light-transmitting, size 3 plastic post (Luminex post Dentatus, USA) were coated with petroleum jelly then centered and fully seated into the canals. After 3-4 h, the Luminex posts were removed using hemostat and the space created by Luminex post was filled with guttapercha /nano HA.
Group 4 (n=15): Obturation was done with 0.06 tapered Resilon cones (Pentron Dental Products, Wallingford, CT, USA). Epiphany sealer was mixed according to the manufacturer's instructions. Self-etching primer (Epiphany Primer; Pentron Dental Products) was introduced into the canal using applicator brushes. A master Resilon cone coated with Epiphany sealer was inserted into the canal. Lateral compaction was performed using Resilon cones. Material in the root canal was light cured for 30 s with a light-curing unit (Hilux UltraPlus, Turkey).
Group 5 (n=15): This group is similar to group 2, but resilon/epiphany was used instead of GP/Nano HA.
Group 6 (n=15): This group is similar to group 3, but resilon/epiphany was used instead of GP/nano HA.
All the roots were mounted vertically in self-cured acrylic resin (Sofa Dental, Kerr Company, Germany) blocks exposing 5 mm of the coronal portion. The acrylic blocks were placed on the lower plate of the universal testing machine (Instron 5982, UK). The upper plate was fitted with 4 mm diameter steel spherical. The steel spherical tip was lowered to engage the entire coronal surface of the roots and subjected to a gradually increasing force (1 mm/min), which was directed vertically and parallel to the long axis of the roots. The force level at which the fracture occurred was measured and recorded in Newton (Fig. 1.2).

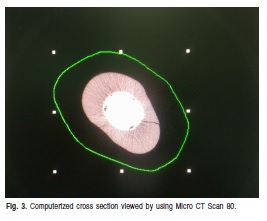
In addition, three-dimensional reconstructions of the roots were obtained using a high-resolution micro CT system (ìCT 80, Switzerland). Three roots from each group were selected and positioned to be scanned in frontal slices. The scan resolution was set at 15 ìm and the beam energy 45 kV. This setting, which corresponds to an effective energy of approximately 24 keV (Fig. 3), was used to measure the depth of fracture line.
Scanning electron microscopy (SEM) was used to analyze the pattern of fracture line. Three roots from each group were selected and placed in numbered containers and dehydrated in a graded series of ethanol solutions. The samples were then dried overnight at room temperature. The dried samples were numbered, mounted on aluminum stubs, placed in a high-vacuum (Polaron SCS 15, Germany) and coated with gold-palladium to render the specimens electrically conductive. Subsequently, the surfaces of samples were examined by a scanning electron microscope (Gemini, Munich, Germany) at 5 Kv.
Results
The results showed that the highest fracture resistance was observed in positive control group (Group +ve), followed by Groups 3, 6, 5, 2, 4 and 1 with values (in N) of 1598 (641.0), 1190.5(424.2), 1164.7 (489.4), 821.2 (220.9), 683.4(179), 658.4 (211.3), 658.4 (99.0) respectively. The lowest fracture resistance force was seen in Group -ve, which was measured at 158.3(49.3) (Table 1).
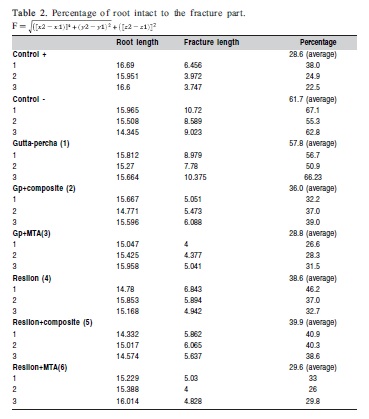
Micro CT Scan showed that roots of Group +ve had the lowest percentage of fracture (28.6%), followed by Group 3 (28.8%), Group 6 (29.8%), Group 2 (36.0%), Group 4(38.6%), Group 5(39.9%) and Group -ve (61.7%). The highest percentage of root fracture was observed in Group1 (66.23%), as shown in Table 2.
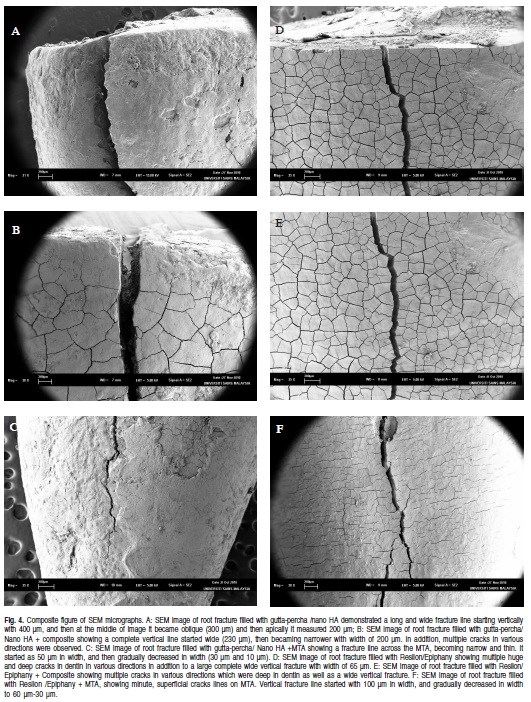
SEM analusis showed that application of vertical force on to the root canals filled with MTA resulted in a single deep vertical fracture line whereas those filled with composite and resilon exhibited several cracks and fracture lines all over the roots (Fig. 4).
Discussion
Previous studies have suggested that the fracture resistance of teeth decrease as mechanical instrumentation destroys the integrity of the internal walls of the root canal20-26. Obviously, mechanical instrumentation of the root canal is an unavoidable step in endodontic treatment23,27,. According to Kivanc et al.25, (2009), the fracture strength of teeth withthin wall and filled roots is affected by the remaining dentin thickness.
When extracted human teeth are used in fracture resistance studies, the potential for large and uncontrollable variations exists. Therefore, when possible, all controllable factors should be standardized23,27.
Use of dentin-bonded composite resins for intraradicular reinforcement of teeth with significant loss of coronal and radicular structures has been suggested as a desirable alternative to morphologic dowel rehabilitation28-32. The rationale for the use of dentin-bonded resins has been well documented. When the light–transmitting technique for bonded composite rehabilitation is used, the intraradicular composite undergoes polymerization shrinkage in the direction of the bonded interface. This shrinkage will result in volumetric space for post manipulation and cementing materials if needed28-32.
In the present study, analysis of the results seem to point out that, the roots in MTA groups (groups 3, 6) were significantly more resistant to fracture as compared with the gutta-percha (group1), resilon (group4) or composite groups (groups 2 and 5).This indicates that MTA not only provides resistance to bacterial penetration by closing the open apex33-34, but also could strengthen the tooth by increasing resistance to fracture. In addition, it was observed that roots filled with MTA had similar fracture resistance when compared with the healthy roots.
This study also showed no significant difference in root reinforcement properties between composite resin and MTA (Groups 2, 3, 5, and 6) when the apical third of the roots were filled with gutta-percha or resilon. The results seem to indicate that gutta-percha and resilon would have no effect on the fracture resistance when used as root-end filling material. Although some studies suggest that due to its adhesive property, resilon may reduce the apical microleakage when compared with gutta-percha10,35.
MTA is a biocompatible, radiopaque material and harder to infiltrate as compared with calcium hydroxide16-17. Results of the study by Hatibovic´-Kofman et al.18 (2008) showed that after 1 year, the teeth filled with MTA had significantly more resistance to fracture compared with those filled with CH or the control18. MTA is a versatile material and it can be used to salvage teeth which are deemed non-restorable due to the extensive caries, developmental anomalies, iatrogenic damage created by excessive root canal preparation or excessive root taper. However, several factors could influence MTA's compressive strength. These include but not limited to the type of MTA, the mixing liquid, the condensation pressure on the material, the pH value of the mixing liquid, and the condition of MTA storage16,33-34. One of the main disadvantages of MTA is that it has a long setting time. However, this shortcoming can be remedied by changing the particle size.
In this study, Micro CT scan 80 was used to measure the depth of fracture lines in a three-dimensional manner. The results indicated that MTA had the highest ability to absorb or to withstand the load applied when compared with composite, resilon and gutta-percha. In the current study, there was a difference in fracture pattern detected amongst the 6 test groups. The fractures began at the cervical area within the filling materials. In MTA groups the pattern of fracture line images showing multiple narrow, incomplete, separated cracks vertically and obliquely with only one vertical line. As it crossed the MTA it became narrower and thinner and then it disappeared. Composite and resilon images showed the presence of several cracks all over the dentin in multiple directions. Additionally, there were large wide vertical and horizontal fracture lines and the filling material is exposed with voids and non-homogenous areas at the periphery. This occurred because of stress concentration at the cervical area of the remaining root structure due to the following reasons, first the samples had thin dentinal root canal wall and a thick layer of resin composite. Consequently, large polymerization contraction stresses of the resin composite concentrated at the adhesive interface36. Second, creeping of incompletely polymerized resinous sealers resulted in failure along the sealer dentin interface37. Third, the presence of residual monomers in the root canals38, and most importantly, the low cohesive, tensile and compressive strengths, and modulus of elasticity of the currently available root filling materials when compared with dentin39, with the former behaving as elastomers that dissipate instead of transmit stresses40.
In conclusion, MTA can be used to reinforce thin-walled roots and replace the lost radicular dentin. The use of Micro CT scan 80 in this study showed that MTA has the ability to absorb or withstand the load when compared with composite, resilon, and gutta-percha. The fracture pattern for roots filled with MTA is only one vertical line which is initially wide and becomes progressively narrower. Whereas roots filled with composite and resilon show several cracks all over the root in addition to the vertical root fracture.
References
1. Richard S, Schwart Z, James W, Robbins. Post placement and restoration of endodontically treated teeth. A literature review. J Endod. 2004; 30: 289-301. [ Links ]
2. Coelho RA, Oliveira AG, Souza-Gabriel AE, Silva SRC, Silva-Sousa YTC, Silva RG. Ex-vivo evaluation of the intrapulpal temperature variation and fracture strength in teeth subjected to different external bleaching protocols. Braz Dent J. 2011; 22: 32-6. [ Links ]
3. Huang T J, Schilder H, Nathanson D. Effects of moisture content and endodontic treatment on some mechanical properties of human dentin. J Endod. 1992; 18: 209-15. [ Links ]
4. Pereira JR, Mendonça Neto T, Porto VC, Pegoraro LF, Valle AL. Influence of the remaining coronal structure on the resistance of teeth with intraradicular retainer. Braz Dent J. 2005; 16: 197-201. [ Links ]
5. Marchi GM, Mitsui FH, Cavalcanti AN. Effect of remaining dentine structure and thermal-mechanical aging on the fracture resistance of bovine roots with different post and core systems. Int Endod J. 2008; 41: 969-76. [ Links ]
6. Pereira JR, de Ornelas F, Conti PC, do Valle AL. Effect of a crown ferrule on the resistance of endodontically treated teeth restored with prefabricated posts. J Prosthet Dent. 2006; 95: 50-4. [ Links ]
7. Pereira JR, Valle AL, Shiratori FK, Ghizoni JS, Melo MP. Influence of intraradicular post and crown ferrule on the fracture strength of endodontically treated teeth. Braz Dent J. 2009; 20: 297-302. [ Links ]
8. Tang W, Wu Y, Smales R J. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010; 36: 609-17. [ Links ]
9. Sagsen B, Er O, Kahraman Y, Akdogan G. Resistance to fracture of roots filled with three different techniques. Int Endod J. 2007; 40: 31-5. [ Links ]
10. Fukui Y, Komada W, Yoshida K, Otake S, Okada,D, Miura H. Effect of reinforcement with resin composite on fracture strength of structurally compromised roots. Dent Mater J. 2009; 28: 602-9. [ Links ]
11. Wilkinson K L, Beeson TJ, Kirkpatrick TC. Fracture resistance of simulated immature teeth filled with resilon, gutta-percha, or composite. J Endod. 2007; 33: 480-3. [ Links ]
12. Zogheib LV, Pereira JR, Valle AL, Oliveira JA, Pegoraro LF. Fracture resistance of weakened roots restored with composite resin and glass fiber post. Braz Dent J. 2008; 19: 329-33. [ Links ]
13. Hammad M, Qualtrough A, Silikas N. Effect of new obturating materials on vertical root fracture resistance of endodontically treated teeth. J Endod. 2007; 33: 732-6. [ Links ]
14. Islam I, Chng H K, Yap AU. Comparison of the physical and mechanical properties of MTA and portland cement. J Endod, 2006; 32: 193-7. [ Links ]
15. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review—Part I: chemical, physical, and antibacterial properties. J Endod. 2008; 36: 16-27.
16. Parirokh,M., Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010; 36: 400-13. [ Links ]
17. Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006; 22: 154-6. [ Links ]
18. Hatibovic-Kofman S, Raimundo L, Zheng L, Chong L, Friedman M, Andreasen J. O. Fracture resistance and histological findings of immature teeth treated with mineral trioxide aggregate. Dental Traumatol. 2008; 24: 272-6. [ Links ]
19. Lawley GR, Schindler WG, Walker WA, Kolodrubetz D. Evaluation of ultrasonically placed MTA and fracture resistance with intracanal composite resin in a model of apexification. J Endod. 2004; 30: 167-72. [ Links ]
20. Karapinar Kazandag M, Sunay H, Tanalp J, Bayirli G. Fracture resistance of roots using different canal filling systems. Int Endod J. 2009; 42: 705-10. [ Links ]
21. Weiger R, Heuchert T, Hahn R, Lost C. Adhesion of a glass ionomer cement to human radicular dentine. Dent Traumatol. 1995; 11: 214-9. [ Links ]
22. Wu X, Chan ATT, Chen YM, Yip K H K, Smales RJ. Effectiveness and dentin bond strengths of two materials for reinforcing thin-walled roots. Dent Mater.2007; 23: 479-85. [ Links ]
23. Moosavi H, Maleknejad F, Kimyai S. Fracture resistance of endodonticallytreated teeth restored using three root-reinforcement methods. J Contem Dent Practe. 2008; 9: 30. [ Links ]
24. Sim T P, Knowles J C, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. 2001; 34: 120-32. [ Links ]
25. Kivanc B, Alacam T, Ulusoy O, Genc O, Gorgul G. Fracture resistance of thin-walled roots restored with different post systems. Int Endod J. 2009; 42: 997-1003. [ Links ]
26. Ulusoy O Ý A, Genc O, Arslan S, Alacam T, Gorgul G. Fracture resistance of roots obturated with three different materials. Oral Surg Oral Med Oral Pathol and Endodontology. 2007; 104: 705-8. [ Links ]
27. Schafer E, Zandbiglari T, Schafer J. Influence of resin-based adhesive root canal fillings on the resistance to fracture of endodontically treated roots: an in vitro preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103: 274-9. [ Links ]
28. Bitter K, Kielbassa AM. Post-endodontic restorations with adhesively luted fiber-reinforced composite post systems: a review. Am J Dent. 2007; 20: 353-60. [ Links ]
29. Goncalves LA, Vansan LP, Paulino SM, Sousa Neto MD. Fracture resistance of weakened roots restored with a transilluminating post and adhesive restorative materials. J Prosthet Dent. 2006; 96: 339-44. [ Links ]
30. Bodrumlu E, Tunga U. Apical leakage of Resilon obturation material. J Contem Dent Pract. 2006; 7: 45-52. [ Links ]
31. Aptekar A, Ginnan K. Comparative analysis of microleakage and seal for 2 obturation materials: Resilon/Epiphany and gutta-percha. J Can Dent Assoc. 2006; 72: 245. [ Links ]
32. Chogle S, Mickel AK, Chan DM, Huffaker K, Jones JJ. Intracanal assessment of mineral trioxide aggregate setting and sealing properties. Gen Dent. 2007; 55: 306-11. [ Links ]
33. Holt DM, Watts JD, Beeson TJ, Kirkpatrick TC, Rutledge, R.E. The antimicrobial effect against enterococcus faecalis and the compressive strength of two types of mineral trioxide aggregate mixed with sterile water or 2% chlorhexidine liquid. J Endod. 2007; 33: 844-7. [ Links ]
34. Baumgartner G, Zehnder M, Paque F. Enterococcus faecalis Type Strain Leakage through Root Canals Filled with Gutta-Percha/AH Plus or Resilon/Epiphany. J Endod. 2007; 33: 45-7. [ Links ]
35. Rueggeberg F, Margeson D. The effect of oxygen inhibition on an unfilled/filled composite system. J Dent Res. 1990; 69:1652-8. [ Links ]
36. Nunes VH, Silva RG, Alfredo E, Sousa-Neto MD, Silva-Sousa YTC. Adhesion of epiphany and ah plus sealers to human root dentin treated with different solutions. Braz Dent J. 2008; 19: 46-50. [ Links ]
37. Filipov IA, Vladimirov SB. Residual monomer in a composite resin after light-curing with different sources, light intensities and spectra of radiation. Braz Dent J. 2006; 17: 34. [ Links ]
38. Texeira FB, Teixeira ECN, Thompson J, Leinfelder KF, Trope M. Dentinal bonding reaches the root canal system. J Esthet and Rest Dent. 2004; 16: 348-54. [ Links ]
39. Zmener O, Banegas G, Pameijer CH. Bone tissue response to a methacrylate-based endodontic sealer: a histological and histometric study. J Endod. 2005; 31: 457-9. [ Links ]
 Correspondence:
Correspondence:
Salma B Abdo
Tawam Dental Centre-Tawam Hospital Office:
(+971-3)7070719 –Mobile (+971-50)7850020
P.O. Box : 15258 Abu Dhabi, United Arab
Emirates
E-mail: salma114@hotmail.com
Received for publication: July 27, 2012
Accepted: October 18, 2012













