Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.1 Piracicaba Jan./Mar. 2013
ORIGINAL ARTICLE
Oral health conditions and self-perception among edentulous individuals with different prosthetic status
Maria Madalena Canuto LemosI, II; Luciane ZaninIII; Maria Leticia Ramos JorgeI; Flavia Martao FlorioII
IDepartment of Dentistry, Faculty of Basic and Health Sciences, Federal University of Valle do Jequitinhonha e Mucuri, Diamantina, MG, Brazil
IIPreventive Dentistry, Sao Leopoldo Mandic School of Dentistry and Research Center, Campinas, SP, Brazil
IIIPreventive Dentistry, Herminio Ometto University Center, Araras, SP, Brazil
ABSTRACT
AIM: To evaluate the objective oral health conditions and self-perception of edentulous individuals wearing functional complete dentures (FCD) and non-functional complete dentures (NFCD) and completely edentulous non-denture wearers, and identify the factors that influence self-evaluation and the impact on quality of life.
METHODS: The convenience sample was selected at the integrated clinic of a Dentistry Course (n=193) and was divided into 3 groups: FCD wearers (n= 54); NFCD wearers (n= 65); 3- edentulous non-denture wearers (n= 74). Data collection was performed by means of interviews, application of the Geriatric Oral Health Assessment Index (GOHAI) and clinical exams. Data were submitted to univariate analysis and logistic regression, considering dichotomization of the sample by the median value of GOHAI (=30).
RESULTS: Individuals with NFCD are 4.5 times more likely to show a low GOHAI score than individuals with FCD; edentulous individuals are 7.5 times more likely to show a low GOHAI score than individuals with FCD; individuals that consider their oral health as regular, poor or bad are 3.1 times more likely to show a low GOHAI score than individuals who consider their oral health as good or excellent.
CONCLUSIONS: Being completely edentulous or wearing NFCD, and having oral health classified as regular, poor or extremely bad were important features for a negative self-perception of oral health, with impact on quality of life.
Keywords: oral health survey, quality of life, complete dentures,edentulism.
Introduction
Life expectancy of the Brazilian population has increased significantly over the last few years, showing the importance of quality of life to the healthy aging and consequent need for specific health policies for this population1-4. Edentulism is a prevalent condition in elderly individuals worldwide5. In Brazil, recent studies have pointed out the presence of edentulism in 7 million individuals aged 65 to 74 years6, and it could be affirmed that complete dentures (CD) continue to be significant instruments of oral rehabilitation for this population7.
Various studies have pointed out the strong association between oral health and quality of life3-15. Compromised oral health may affect the nutritional level as well as physical and mental well being, in addition to diminishing the pleasure of an active social life16-17. Edentulism is a preponderantly negative factor for the oral and general health of individuals, with strong impact on quality of life. Absence of teeth reduces masticatory function, resulting in alterations to dietary habits9,14.
Adequate CD are capable of restoring function and promoting social and psychological well being3,15. Nevertheless, it is important to observe that the majority of these appliances are in an unsatisfactory condition for use18-19, which compromises oral health, with impact on quality of life. Oral lesions, such as stomatitis, inflammatory hyperplasia, traumatic ulcers and angular cheilitis are directly associated with the use of inadequate CD2. Little research has been done about the self-perception of oral health and its impact on the quality of life of individuals7-8,10,15.
Different instruments have been developed to obtain data about self-perception of the oral condition and the impact on quality of life. One of these instruments is the Geriatric Oral Health Assessment Index (GOHAI)20, which groups oral health self-perception in three basic functions: physical, psychosocial and pain/discomfort21.
In this way, the perceived oral health becomes an important tool for diagnosing the priority requirements of this population and implementing actions that result in an improvement in quality of life11, through the development of educational, preventive and social measures and policies specifically for this population.
The aims of this study were to evaluate the objective oral health conditions and self-perception of edentulous individuals wearing functional complete dentures (FCD) and non-functional complete dentures (NFCD) and completely edentulous non-denture wearers, and to identify the factors that influence self-evaluation and the impact on quality of life.
Material and methods
The research consisted of a study involving questions about objective and subjective oral health in a convenience sample composed of 193 participants, age-range between 29 and 100 years (59.7±13.6), who were treated after screening at the Integrated Clinic of the Dentistry Course of the Federal University of Vale do Jequitinhonha e Mucuri - UFVJM, Diamantina, MG, Brazil, between April and December, 2009. The study was approved by the institutional Ethics Committee (Protocol # 026/09).
A pilot study was conducted with 30 participants to test the methodology and instruments to be used. Two weeks later this group was re-evaluated. Calibration for the clinical exam was carried out in accordance with the recommendations of the Examiner Calibration Manual of SB Brazil22, and the Kappa agreement index was 0.91.
The data collection instruments were composed of an interview form, application of the GOHAI index and a clinical exam form. By means of the interview form, sociodemographic data were obtained, and two questions about self-perception were applied: 1- do you consider that you need treatment at present? (yes/no); 2- How would you classify your oral health? (excellent/good/regular/poor/extremely bad). Interviews were conducted individually by a calibrated member of the integrated clinic staff.
For self-evaluation of oral health the GOHAI20 questionnaire was used, composed of 12 items that deal with oral health conditions, by self-perception in three dimensions: the physical, psychosocial and that of pain or discomfort. The physical dimension included diet, speech and swallowing. The psychosocial included concern about and interest in oral health, as well as dissatisfaction with appearance. The dimension of pain and discomfort included the use of medications to alleviate pain and discomfort provided that they appeared in the mouth. For each question, the questionnaire offers the alternatives "always", "sometimes" and "never", which were given scores 1, 2 and 3 respectively. The index is the result of the sum of scores to the questions on a scale from 12 to 36, so that the higher the score the better the oral health self-evaluation.
The researcher performed the clinical exams to determine the objective conditions of the individual's oral health. For each exam, the dental chair, reflector illumination, #5 dental mirror and a wooden spatula were used. The following features were observed: oral lesions, use and need for CD, time of denture wearing and its condition. The clinical exam criteria were based on the WHO Manual23, as described in the examiner manual22.
The volunteers were divided into three groups: Group 1- FCD wearers (n=54), Group 2- NFCD wearers (n= 65) and Group 3- completely edentulous individuals who did not wear dentures (n= 74).
FCD were considered to be those that met the clinical requisites of stability, fit, occlusion, esthetics, retention and integrity19,24. NFCD were considered to be those that had compromised at least one of the requisites required for FCD. Edentulous individuals were considered to be completely edentulous volunteers, at least in one arch, without the presence of CD at the time of the exam.
For statistical treatment of the data the Statistical Package for Social Science (SPSS), version 15.0 Software was used. The impact of the oral condition on the quality of life evaluated by means of dichotomization of GOHAI was chosen as a dependent variable. Univariate analysis was performed to verify the association between each of the independent variables with GOHAI. For dichotomization of the sample, individuals with a positive perception of oral health were considered those whose scores presented values equal to or greater than the median (>30) and negative perception of oral health was considered with the scores presented values below the median. Association of this variable with the independent variables was initially evaluated by means of the Chi-square test. The level of significance as set at 5%. Multiple logistic regression was performed to verify whether the impact of the oral condition on the quality of life was independently associated with the variables.
Results
The volunteers' ages ranged from 29 to 100 years (59.7±13.6), the majority were women (73.6%), 66.3% came from the urban area, 74% had 4 or more years of schooling and 79.2% had a monthly income of approximately US$170 per month or less. As regards the subjective need for treatment, 66.3% affirmed that they needed treatment, but the majority of the volunteers (68%) classified their oral health as good or excellent. The normative need for dentures was verified in 71.5% of the participants. The time of use of the mandibular CD ranged from 1 to 45 years and that of the maxillary CD between 1 and 55 years. Oral lesions were present in 13.5% of the participants.
Table 1 shows the association of the dependent variable GOHAI, dichotomized as a function of the median value (=30), with the independent variables, using the chi-square statistical test. Significant association was verified between the following variables and the impact on quality of life (GOHAI): Study groups, treatment need (subjective), classification of oral health (subjective), need for complete denture use, personal income, time of use of the mandibular denture, time of use of the maxillary denture and presence of oral lesions. The impact was greater among the edentulous patients (68.9%) and NFCD wearers (67.7%), in comparison with the FCD wearers (20.4%). The impact was also greater among the participants who considered their oral health regular, poor or extremely bad (77,4%), in comparison with those who considered it good or excellent (44.3%).
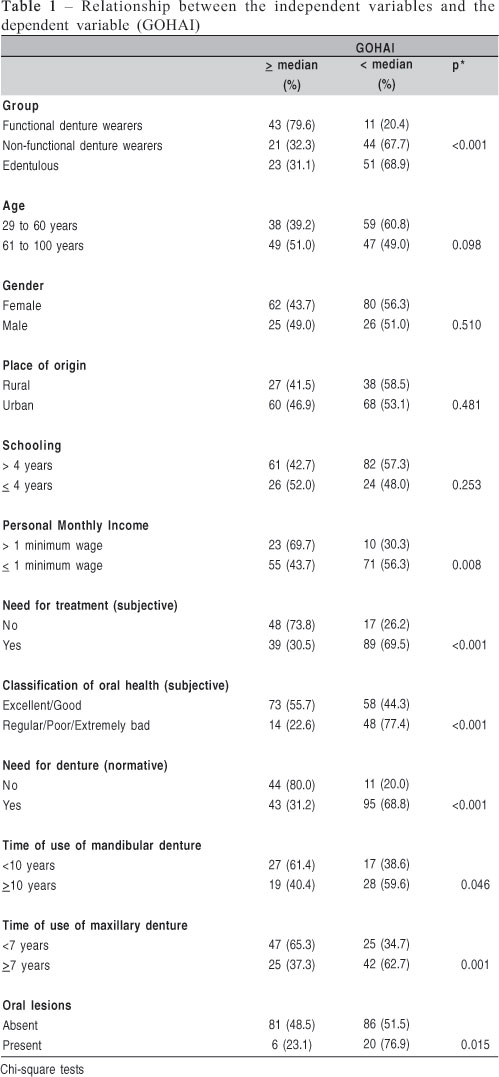
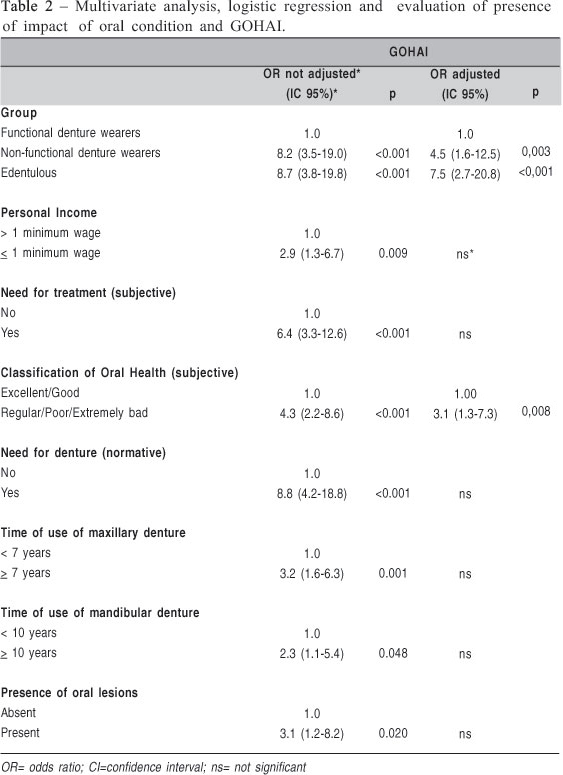
Table 2 shows that individuals who were NFCD wearers presented 4.5 times more chance of a low GOHAI score than those with FCD. Edentulous individuals presented 7.5 times more chance of presenting a low GOHAI score than the FCD wearers. Individuals who classified their oral health as regular, poor or extremely bad presented 3.1 times more chance of presenting a low GOHAI score than those who classified it as good or excellent.
Discussion
Diagnosis of the conditions of health/disease in population groups has traditionally been made by means of approaches based on the biomedical model, in which health is understood simply as the absence of disease, and determination of health needs is obtained only from the normative point of view4,11,25. This point of view ignores important socio-behavioral aspects that must be considered in the evaluation of oral health conditions26. Self-evaluation or oral health has been one of the indicators of quality of life widely used in Dentistry as it reflects the subjective experience of individuals about their functional, social and psychological well being12,27.
In this study, clinical-objective and subjective approaches to oral health were used, based on the self-perception of individuals. To evaluate the subjective conditions of oral health, a transculturally translated version21 of the GOHAI index20 was used. It is a multidimensional evaluation instrument, and has been widely used10,25,27-29.
Although findings in this study were limited by the use of a convenience sample and the perceptions of oral health status in a select sample at the integrated clinic of a Dentistry Course, in the present investigation, a strong association was verified between the variable 'Group' (FCD, NFCD and edentulous) and 'GOHAI', with impact on the quality of life. Oral rehabilitation by means of CD continues to be significant in the dental clinic, in spite of the great technical-scientific advancement of the profession7,30. However, the success and satisfaction with these appliances are directly associated with the physical, functional and psychosocial self-perfection of oral health by individuals31-33. The majority of the participants in the FCD group presented positive evaluation of oral health, corroborating the findings of other studies7-8,15, demonstrating that adequate CD are efficient instruments for recovering the masticatory function and promoting physical, social and psychological health of edentulous individuals, promoting satisfaction, increasing self-esteem and significantly enhancing their quality of life. This was the group with the highest scores for GOHAI, similar to the values obtained by Veyruneet al19.
The NFCD group presented 4.5 times more chance of having a low GOHAI score in comparison with the FCD group and presented a negative evaluation of oral health, demonstrating that the deficient condition of the CD exerts a strong influence on the individual's oral health, resulting in a negative impact on the quality of life, because of the discomfort, difficulty with chewing and expression, reflected in his/her functional, social and psychological well being19,34. Most dentures are found to be in unsatisfactory conditions18-19 and one of the reasons is their long time in use25 because functional qualities such as stability, retention, occlusion and vertical dimension become progressively unfavorable over time, and a specialized follow up is necessary for the maintenance of these dentures16,32.
In this investigation it was verified that the majority of individuals in the edentulous group presented a negative evaluation of oral health, and had 7.5 times more chance of having a low GOHAI score than those in the FCD group, demonstrating that this was the worst condition. These results corroborate those of other investigations that verified that tooth loss has a strong impact on people's life, and involves negative consequences, affecting significantly their quality of life5,7,9,13-14,17.
As regards the subjective classification of oral health, the majority of the volunteers considered their oral health good or excellent, and presented a positive self-perception of oral health, corroborating the results of other investigations4,21. It is worth mentioning that most people see their oral condition in a favorable manner, even under unsatisfactory clinical conditions. This was probably because the clinical criteria of health used by the professional do not coincide with the individuals' perception of oral health21,27, as occurred in this study, demonstrating that objective health measures are insufficient for evaluating the individual's oral health4,35.
Participants who classified their oral health as regular, poor or extremely bad presented 3.1 times more chance of presenting a low GOHAI score than those who classified it as good or excellent, showing a negative evaluation of oral health. These results corroborate those of Martins et al.4, who verified that subjective conditions, related to the impact on quality of life, were more strongly associated with negative self-evaluation of oral health, than objective conditions of health.
The edentulous group presented the worst self-perception of oral health with the greatest impact on quality of life, followed by the NFCD wearers. The need to use a CD or even the use of a NFCD and the classification of oral health as regular, poor or extremely bad, were risk factors for the negative self-evaluation of oral health, demonstrating that the oral condition exerts a strong impact on people's life.
The findings of this study suggest that being completely edentulous, or wearing NFCD, and oral health classification into regular, poor or extremely bad were important features for negative self-perception of oral health, with impact on the volunteers quality of life.
References
1. Souza RF, Patrocínio L, Pero AC, Marra J, Compagnoni MA. Reliability and validation of a Brazilian version of the Oral Health Impact Profile for assessing edentulous subjects. J Oral Rehabil. 2007; 34: 821-6. [ Links ]
2. Freitas JB, Gomez RS, de Abreu MHNG, Ferreira EF. Relationship between the use of full dentures and mucosal alterations among elderly Brazilians. J Oral Rehabil. 2008; 35: 370-6. [ Links ]
3. Silva MES, Magalhães CL, Ferreira EF. Complete removable prostheses: from expectation to (dis)satisfaction. Gerodontology. 2009; 26: 143-9. [ Links ]
4. Martins AMEBL, Barreto SM, Pordeus IA. Objective and subjective factors related to self-rated oral health among the elderly. Cad Saúde Pública.2009; 25: 421-35. [ Links ]
5. Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health. Community Dent Oral Epidemiol. 2005; 33: 81-92. [ Links ]
6. Brazil. Ministry of Health Care/Health surveillance. Departament of Primmary Care. Coordination of Oral Health. Project SB Brazil 2010 -main results. Brasilia; 2011. [ Links ]
7. Carlsson GE, Omar R. The future of complete dentures in oral rehabilitation: A critical review. J Oral Rehabil. 2009; 37: 143-56. [ Links ]
8. Koshino H, Hirai T, Ishijima T, Tsukagoshi H, Ishigami T, Tanaka Y. Quality of life and masticatory function in denture wearers. J Oral Rehabil. 2006; 33: 323-9. [ Links ]
9. Tramini P, Montal S, Valcarcel J. Tooth loss and associated factors in long-term institutionalised elderly patients. Gerodontology. 2007; 24: 196-203 [ Links ]
10. Ellis JS, Pelekis ND, Thomason JM.Conventional rehabilitation of edentulous patients: the impact on oral health-related quality of life and patient satisfaction. J. Prosthod. 2007; 16: 37-42. [ Links ]
11. Mesas AE, Andrade SM, Cabrera MAS. Factors associated with negative self-perception of oral health among elderly people in Brazilian community. Gerodontology. 2008; 25: 49-56. [ Links ]
12. Baker SR, Pearson NK, Robinson PG. Testing the applicability of a conceptual model of oral health in housebound edentulous older people. Community Dent Oral Epidemiol. 2008; 36: 237-48. [ Links ]
13. Gagliardi DI, Slade GD, Sanders AE. Impact of dental care on oral health-related quality of life and treatment goals among elderly adults. Aust Dent J. 2008; 53: 26-33. [ Links ]
14. Brennan DS, Spencer AJ, Thomson-Roberts KF. Tooth loss, chewing ability and quality of life. Qual Life Res. 2008; 17: 227-35. [ Links ]
15. Kuo HC, Yang YH, Lai SK, Yap SF, Ho PS. The Association between health-related quality of life and prosthetic status and prosthetic needs in Taiwanese adults. J Oral Rehabil. 2009; 36: 217-25. [ Links ]
16. Carlsson GE. Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent.1998; 79: 17-23. [ Links ]
17. Pan S, Awad M, Thomason MJ, Dufresne E, Kobayashi T, Kimoto S et al. Sex differences in denture satisfaction. J Dent. 2008; 36: 301-8. [ Links ]
18. McNaugher GA, Benington IC, Freeman R. Assessing expressed need and satisfaction in complete denture wearers. Gerodontology. 2001; 18: 51-7. [ Links ]
19. Veyrune JL, Tubert-Jeannin, Dutheil C, Riordan, PJ. Impact of new prostheses on the oral health related quality of life of edentulous patients. Gerodontology. 2005; 22: 3-9. [ Links ]
20. Atchison KA, Dolan TA. Development of The Geriatric Oral Health Assessment Index. J Dent Educ 1990; 54: 680-7. [ Links ]
21. Silva SRC, Fernandes RAC. Self-perception of oral health status by the elderly. Rev Saude Publica. 2001; 35: 349-55. [ Links ]
22. Brazil. Ministry of Health. Public Policy Department of Health, Department of Primary Care, Technical Department of Oral Health. Project SB 2000. Oral health status of the population in 2000: Examiner's Manual. Brasilia: Ministry of Health; 2001. 49p. [ Links ]
23. World Health Organization. Oral health surveys: basic methods. 4th ed. Geneva.: WHO; 1997. [ Links ]
24. De Baat C, van Aken AAM, Mulder J, Kalk W. "Prosthetic condition" and patients' judgment of complete dentures.J Prosthet Dent. 1997; 78: 472-8. [ Links ]
25. Colussi Cf, Freitas SFT, Calvo MCM. The prosthetic need WHO index: a comparison between self-perception and Professional assessment in na elderly population. Gerodontology. 2009; 26: 187-92. [ Links ]
26. Reis SCGB, Higino MASP, Melo HMD, Freire MCM. Oral health status of institutionalized elderly in Goiânia-GO, Brazil, 2003. Rev Bras Epidemiol. 2005; 8: 67-73. [ Links ]
27. Locker D, Gibson B. Discrepancies between self-ratings of and satisfaction with oral health in two older adult populations. Community Dent Oral Epidemiol. 2005; 33: 280-8. [ Links ]
28. Locker D, Matear D, Stephens M, Lawrence H, Payne B. Comparison of the GOHAI and OHIP-14 as measures of the oral health-quality of life of the elderly. Community Dent Oral Epidemiol. 2001; 29: 373-81. [ Links ]
29. Abud MC, dos Santos JFF, da Cunha VPP, Marchini L. TMD and GOHAI índices of Brazilian institutionalised and community-dwelling elderly. Gerodontology. 2009; 26: 34-9. [ Links ]
30. Silva MES, Villaça EL, Magalhães CL, Ferreira EF. Impact of tooth loss in quality of life. Cienc Saude Col. 2010; 15: 841-50. [ Links ]
31. Bae KH, Kim C, Paik DI, Kim JB.A comparison of oral health related quality of life between complete and partial removable denture-wearing older adults in Korea.J Oral Rehabil. 2006; 33: 317-22. [ Links ]
32. Fenlon MR, Sherriff M. An investigation of factors influencing patients' satisfaction with new complete dentures using structural equation modelling. J Dent. 2008; 36: 427-34. [ Links ]
33. Emami E, Alisson PJ, de Grandmont P, Rompré PH, Feine JS. Better oral health related quality of life: Type of prosthesis or psychological robustness? J Dent. 2010; 38: 232-36. [ Links ]
34. John MT, Koepsell TD, Hujoel P, Miglioretti DL, LeResche L, Micheelis W. Demographic factors, denture status and oral health-related quality of life.Community Dent Oral Epidemiol. 2004; 32: 125-32. [ Links ]
35. Lacerda JT, Castilho EA, Calvo MCM, Freitas SFT. Oral health and daily performance in adults in Chapecó, Santa Catarina State, Brazil. Cad. Saude Publica. 2008; 24: 1846-58. [ Links ]
 Correspondence:
Correspondence:
Flavia Martao Florio
Rua Jose Rocha Junqueira, 13, Ponte Preta
CEP:13045-755, Campinas, SP, Brasil
E-mail: flavia.florio@yahoo.com
Received for publication: October 04, 2012
Accepted: January 10, 2013













