Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.1 Piracicaba Jan./Mar. 2013
ORIGINAL ARTICLE
Is depression associated with periodontal status in elderly?
Leonel Ramonnd Ferreira VianaI; Consuelo Penha CastroI; Hellen-Bry Wanderley PereiraII; Adriana de Fátima Vasconcelos PereiraI; Fernanda Ferreira LopesI
IDepartment of Dentistry, Dental School, Federal University of Maranhão, São Luís, MA, Brazil
IIFederal University of Maranhão, São Luís, MA, Brazil
ABSTRACT
AIM: To examine whether the depression is associated with periodontitis in elderly and to evaluate oral hygiene of these patients.
METHODS: One hundred and ninety one individuals aged 60 years or more were randomly selected. Periodontal examination was performed in full mouth by probing depth and clinical attachment loss in 6 sites for each tooth. The Simplified Oral Hygiene Index (OHI-S) per individual was also obtained. Depression was assessed by the Geriatric Depression Scale (GDS-15) to show how the elderly have been feeling during the last week.
RESULTS: Only SOHI was statistically significant (t = 4.7169, p<0.001), which better explains the variance in periodontal status. The variable GDS-15 revealed no significant values (t=0.3901, p=0.6971).
CONCLUSIONS: There was no association between periodontitis and depression in elderly, but there was association between periodontitis and oral hygiene.
Keywords: depression, periodontitis, oral hygiene, elderly.
Introduction
Aging is a constant and complex process that occurs in all types of body cells, although it presents special features in certain organs and systems1. According to the World Health Organization (WHO), the chronological level of 60 years of age is used to define an elderly population in developing countries2.
Oral conditions and depressive symptoms in elderly have been little studied. There are few studies about the association between periodontal disease and depression in elderly3; however, several studies have addressed the association between periodontal disease and stress4-6. The depressed activity of neutrophils and macrophages linked to human physical and psychological states, such as family problems, aging and unemployment, can clarify the role of depression on periodontal condition7.
Considering that depression and periodontal diseases are accompanied by an activation of inflammatory responses, the aim of this study was to examine whether depression in elderly may be a systemic factor associated with periodontitis and to evaluate oral hygiene of these patients.
Material and methods
This cross-sectional study was conducted in accordance with the resolution 196/96 of the Brazilian National Health Council and Complementary, and was approved by the Ethics Committee of the Federal University of Maranhão (Protocol number 2315-012694/2008-90).
Population and Sample
Sample size calculation was performed using the Bioestat 3.0 (Ayres M., MCT-CNPq, Belém, PA, Brazil), which indicated a minimum sample of 188 elders with a power test of 80% and alpha level of 5%8. The sample was formed by random number table and was composed by 191 subjects aged 60 years or more from those attending the university for third-age persons of Federal University of Maranhão. Smokers, edentulous individuals and those who underwent periodontal treatment less than 6 months before were excluded.
Data Collection
A questionnaire was used to assess personal health history and physical factors. The Geriatric Depression Scale (GDS-15) was applied to detect depressive symptoms in elderly by 15 negative/affirmative questions. One point was assigned for each positive answer, where 0-4 points was considered normal, 5-10 points were diagnosed with a probable light depression and 11-15 points with a probable severe depression9.
A full-mouth periodontal examination was performed. The extent measure of attachment loss was performed by measurements of probing depth (PD) and clinical attachment loss (CAL) using a Williams periodontal probe (Hu Friedy®, Chicago, IL, USA) parallel to the tooth long axis10. The Simplified Oral Hygiene Index (OHI-S) for every individual11 was also obtained, and classified as adequate and inadequate (regular and poor). Severe periodontitis was diagnosed based on PD 3 4mm and CALe" 5mm12.
Statistical Analysis
Logistic regression model was used to verify whether at least one of the independent variables (the OHI-S and GDS-15) had influenced the dependent variable (severe periodontitis). The chi-square test was used to analyze the distribution of severe periodontitis, oral hygiene and geriatric depression. For all the tests was used the significance level of 5%.
Results
Among the 191 participants, 156 (81.7%) were female and 35 (18.3%) were male aged 60 years or more, and the mean age was 68.8 years. The educational status of the elderly was an average 5.6 years of study. Most participants were married corresponding to 71 (37.17%), followed by widowed (64/33.51%), single (40/20.94%) and divorced (16/8.38%).
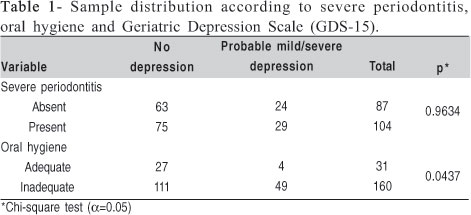
Severe periodontitis was present in 104 (54.4%) elders, while 160 (83.7%) revealed inadequate oral hygiene and 138 (72.3%) did not have depression. Table 1 illustrates the sample distribution according to depression, oral hygiene and severe periodontitis. Ordinal logistic regression model measured the outcome variable (periodontal status) and the exposure variables (depression, oral hygiene) and showed an association between periodontal status and oral hygiene, which was used as adjustment for confounding bias, and lack of association between periodontal status and depression in elderly (Table 2).

The periodontal dependent variable and the independent variables, OHI-S and depression, were also submitted to the multiple regression test, which showed the value of F (regression) as significant (F= 11.4549, p<0.001), accepting that at least one of the variables had influence on periodontal status. Among the partial regression coefficients, only the OHI-S was statistically significant (t=4.7169, p<0.001) which may better explain the variance on periodontal status. The GDS-15 revealed no significant values (t=0.3901, p = 0.6971).
Discussion
Depression is the result of several interdependent neurobehavioral symptoms. The variation may be explained by stress factors that have been associated with a decrease in immune function and increase of the susceptibility to infections. Moreover, if the relation stress/periodontal disease is true, greater prevalence of this disease can be found among patients with severe depression5.
This study evaluated depression as a perceived risk factor associated with periodontal disease in elderly, but no Tobacco smoking has been associated with an increased prevalence and severity of periodontal diseases, and there is evidence that systemic and local malondialdehyde (MDA) levels are increased by smoking in addition to having an impact on periodontitis13. In this study, smokers were excluded to eliminate this potential confounder, based on the fact that smoking may be considered a risk factor for further periodontal disease progression among healthy elderly people aged 70 years and over8. Periodontal disease in elderly is a common process of aging and there were no significant correlations between mean serum levels of disease markers and additional attachment loss8, so the risk factors for systemic diseases such as diabetes and coronary heart disease were included in our study.
The World Health Organization2 classifies the aging process in four stages: the middle-elderly from 45 to 59 years old, the elderly from 60 to 74 years old, the ancient from 75 to 90 years old and extreme old age from 90 years onwards. Thus, the age group chosen for evaluation in this study was composed by elders aged 60 years or more, since the epidemiological studies indicated greater severity6,14 and prevalence15 of periodontal disease in people over 50 years6,14-15.
A case-control study has been conducted to determine whether severe periodontitis and its treatment are associated with oxidative stress16. The authors found that patients with severe periodontitis exhibited higher Diacron-reactive oxygen metabolites (D-ROM) levels, so they suggest a positive association between severe periodontitis and oxidative stress. Croucher et al.17 showed that periodontitis may be related to psychological stress in adults. However, these studies have non-homogenous samples, so it is possible that depression among young and old subjects is different and the elderly who reported depression may only have developed this condition recently, instead of having a psychiatric disorder earlier in life.
Periodontal examination was conducted in all teeth and not only in the index teeth. This choice provides the best way to assess accurately the prevalence and severity of periodontal disease in a population18. The partial examination underestimates the extension, severity and prevalence of periodontitis when compared with the full mouth method10.
Within the limitations of this study, it was concluded that there was no difference in frequency distribution of periodontitis between elderly with depression or not, but the elderly with depression showed significantly more inadequate oral hygiene. So, there was no association between periodontitis and depression in elderly, but there was association between periodontitis and inadequate oral hygiene, which it was used as adjustment for confounding bias. Due to the high frequency of inadequate oral hygiene in elderly, great need for dental care to this age group is required, so this study has provided data to emphasize the need of dentists in multidisciplinary elderly care teams.
Acknowledgements
The authors thank the State of Maranhão Research Foundation (FAPEMA) for the scholarship grant to the Graduate program.
References
1. Oliveira MC, Schoffen JPF. Oxidative Stress Action in Cellular Aging. Braz Arch Biol Technol. 2010; 53: 1333-42. [ Links ]
2. WHO Library Cataloguing in Publication Data. Integrating poverty and gender into health programmes: a sourcebook for health professionals: module on ageing. Geneva: WHO; 2006. [ Links ]
3. Persson GR, Persson RE, MacEntee CI, Wyatt CC, Hollender LG, Kiyak HA. Periodontitis and perceived risk for periodontitis in elders with evidence of depression. J Clin Periodontol. 2003; 30: 691-6. [ Links ]
4. Goyal S, Jajoo S, Nagappa G, Rao G. Estimation of relationship between psychosocial stress and periodontal status using serum cortisol level: a clinico-biochemical study. Indian J Dent Res. 2011; 22: 6-9. [ Links ]
5. Peruzzo DC, Benatti BB, Ambrosano GM, Nogueira-Filho GR, Sallum EA, Casati MZ et al. A Systematic Review of Stress and Psychological Factors as Possible Risk Factors for Periodontal Disease. J Periodontol. 2007; 78: 1491-1504. [ Links ]
6. Wimmer G, Janda M, Wieselmann-Penkner K, Jakse N, Polansky R, Pertl C. Coping with stress: its influence on periodontal disease. J Periodontol. 2002; 73: 1343-51. [ Links ]
7. Bartolomucci A. Social stress, immune functions and disease in rodents. Front Neuroendocrinol. 2007; 28: 28-49. [ Links ]
8. Ogawa H, Yoshihara A, Amarasena N, Hirotomi T, Miyazaki H. Risk factors for periodontal disease progression among elderly people. J Clin Periodontol. 2002; 29: 592-7. [ Links ]
9. Sousa RL, Medeiros JGM, Moura ACL, Souza CLM, Moreira IF. Validity and reliability of the Geriatric Depression Scale for the identification of depressed patients in a general hospital. J Bras Psiquiatr. 2007; 56: 1027. [ Links ]
10. Borges-Yánez AS, Irigoyen-Camacho ME, Maupomé G. Risk factors and prevalence of periodontitis in community-dwelling elders in Mexico. J Clin Periodontol. 2006; 33: 184-94. [ Links ]
11. Albandar, JM, Rams TE. Global epidemiology of periodontal diseases: an overview. Periodontol 2000. 2002; 29: 7-10. [ Links ]
12. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4: 1-6. [ Links ]
13. Tonguç MÖ, Öztürk O,Sütçü R, Ceyhan BM, Kýlýnç G, Sónmez Y, Yetkin Ay Z et al. The impact of smoking status on antioxidant enzyme activity and malondialdehyde levels in chronic periodontitis. J Periodontol. 2011 82: 1320-8. [ Links ]
14. Hilgert JB, Hugo FN, Bandeira DR, Bozzetti MC. Stress, cortisol, and periodontitis in a population elderly 50 years and over. J Dent Res. 2006; 85: 324-8. [ Links ]
15. Heitz-Mayfield LJ, Schätzle M, Löe H, Bürgin W, Anerud A, Boysen H, Lang NP. Clinical course of chronic periodontitis. II. Incidence, characteristics and time of occurrence of the initial periodontal lesion. J Clin Periodontol. 2003; 30: 902-8. [ Links ]
16. D'Aiuto F, Nibali L, Parkar M, Patel K, Suvan J, Donos N. Oxidative stress, systemic inflammation, and severe periodontitis.J Dent Res. 2010; 89: 1241-6. [ Links ]
17. Croucher R, Marcenes WS, Torres MC, Hughes F, Sheiham A. The relationship between life events and periodontitis. A case control study. J Clin Periodontol. 1997; 24: 39-43. [ Links ]
18. Ramachandra SS, Mehta DS, Sandesh N, Baliga V, Amarnath J. Periodontal probing systems: a review of available equipment. Compend Contin Educ Dent. 2011; 32: 71-77. [ Links ]
 Correspondence:
Correspondence:
Fernanda Ferreira Lopes
Rua das Jaqueiras, nº5, Qd.55 Bairro Renascença I
CEP: 65075-220 São Luís, MA, Brasil
Phone: +55 98 33018575 / 33018577
E-mail: fernanda.f.lopes@gmail.com
Received for publication: November 24, 2012
Accepted: March 04, 2013













