Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.1 Piracicaba Jan./Mar. 2013
CASE REPORT
Orthokeratinized odontogenic cyst - critical appraisal of a distinct entity
Aditi ByatnalI; Jayalakshmi NatarajanI; Venkadasalapathy NarayanaswamyII; Raghu RadhakrishnanI
IDepartment of Oral and Maxillofacial Pathology, Manipal College of Dental Sciences, Manipal, Manipal University, Karnataka, India
IICraniofacial and Dental Hospital, K. K. Nagar, Madurai, India
ABSTRACT
The orthokeratinized odontogenic cyst (OOC) is a rare developmental jaw cyst. Recognition of OOC as a unique entity has long been due, yet its inexplicable radiographic presentation resembling dentigerous cyst, histological likeness to odontogenic keratocyst (OKC) and inconsistent cytokeratin expression profiles overlapping with both as well as with the epidermis, makes it rather confounding. Diagnosis of OOC is important as the pathologic behavior, clinical outcome and the surgical management of OOC is disparate. This is the report of a case of OOC in relation to an impacted mandibular third molar and critical review of this entity with an emphasis on its biologic characteristics is highlighted.
Keywords: orthokeratinized odontogenic cyst, odontogenic keratocyst, keratocystic odontogenic tumor, intraosseous epidermoid cyst.
Introduction
It has long been documented and established that in addition to odontogenic keratocyst (OKC), the majority of odontogenic cysts produce orthokeratin. Although orthokeratinized odontogenic cyst (OOC) was first described as early as in 1927 by Schultz1, it was first considered to be a variant of OKC. However, with the World Health Organization (WHO) redefining OKC as a neoplasm and redesignating it as keratocystic odontogenic tumor (KCOT) in 2005, it became imperative that OOC had to be separated out from KCOT as a distinct entity. This distinction was germane as the pathogenesis and the progression and prognosis of these two seemingly similar odontogenic cysts is diverse. Equally bewildering of OOC is its resemblance to a dentigerous cyst when it occurs around the crown of an impacted tooth. This report presents a case of OOC in relation to an impacted mandibular third molar and discusses its possible pathogenesis.
Case Report
A 36-year-old male patient presented with a swelling in the right posterior region of the lower jaw of 6 months duration. History revealed that the swelling grew progressively in size with no significant aggravating or relieving factors. Past dental history and medical history was non-contributory. On clinical examination, an intraoral swelling measuring about 2x3 cm in size was observed in the right posterior region of mandible. The swelling was diffuse, asymptomatic, and bony hard on palpation with the overlying mucosa intact.
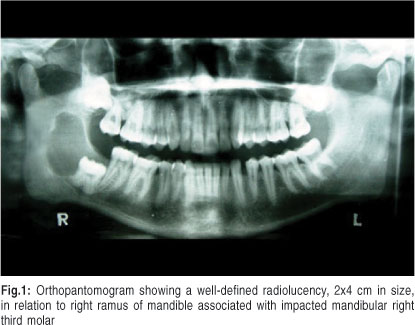
Orthopantomographic examination showed a well-defined radiolucency approximately 2x4 cm in size, in relation to the right ramus of the mandible associated with a distally impacted mandibular right third molar (Figure 1).
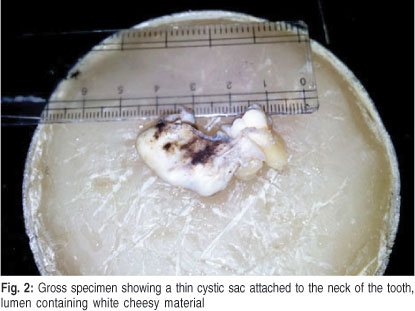
Based on the clinical and radiographic evaluation, a preliminary diagnosis of dentigerous cyst was made. Odontogenic keratocyst and a benign odontogenic tumor were considered in the differential diagnosis. The lesion was surgically enucleated along with the extraction of affected third molar, under local anesthesia and submitted for histopathological examination. Gross examination of the specimen revealed a thin cystic sac attached at the neck of the associated tooth, measuring about 2x4 cm in size. The surface of the cystic lumen appeared smooth and contained white cheesy material (Figure 2).
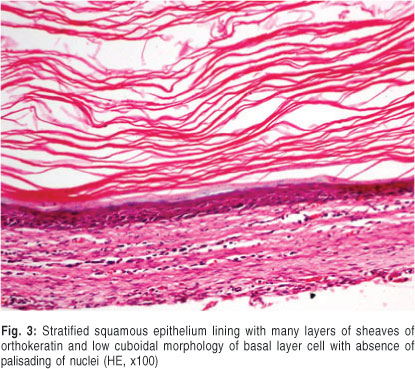
Histopathological examination of the hematoxylin-eosin (HE)-stained sections showed a cystic cavity lined by orthokeratinized stratified squamous epithelium lining, with surface showing sheaves of keratin arranged in many layers. The epithelial lining was about 6-8 layers with a distinct granular cell layer subjacent to cornified layer and basal layer exhibited low cuboidal morphology with absence of palisading of nuclei (Figure 3). The epithelial-connective tissue interface was rather flat and devoid of rete ridges. The capsular tissue was made up of dense fibrous connective tissue with scanty chronic inflammatory cell infiltration. Based on the clinical, radiographic and histopathological features, the cyst was diagnosed as orthokeratinized odontogenic cyst.
Discussion
Jaw cysts, which exclusively result in the orthokeratinization of the lining epithelium, are rather unusual and a descriptive term "orthokeratinized odontogenic cyst (OOC)" has been used for these variants2. The precise incidence of OOCs from the available literature is not consistent as there are no definitive criteria to categorize them as a separate entity. This is reflected by the conflicting documentation of its reported occurrence ranging from 3-11%2. This is further complicated because the majority of them produce orthokeratin and were first considered to be a orthokeratinized variant of OKC.
OOC has been reported to occur among young adults, with a male predominance. Mandible is affected twice more commonly than maxilla, with a predilection for the most posterior region2. Incidentally, about 75% of OOCs are associated with impacted teeth, clinically and radiographically mimicking a dentigerous cyst3. Clinical presentation of OOC with regard to age of occurrence, site of presentation and histochemical profile suggests that it bears a close resemblance to KCOT, yet is different from it with regard to its biologic behavior. OOC may be associated with calcifying odontogenic cyst4, ameloblastoma5, heterotopic cartilage6 or even squamous cell carcinoma3.
The distinction between OOC and KCOT is important as KCOTs can occur at multiple sites, be associated with nevoid basal cell carcinoma syndrome (NBCCS) and recur following surgical enucleation. More importantly, the cysts which show loss of heterozygosity in relation to PTCH gene may progress to malignancy and hence the name KCOT3. The above features such as multiplicity and association with NBCCS, which is commonly associated with KCOTs, are not observed in OOCs according to the report.
Histologically, OOC is characterized by a 4-8-cell-layer-thick orthokeratinized epithelial lining, with prominent granulosum and low cuboidal basal cells; while KCOT epithelial lining is thick, parakeratinized with the basal cells exhibiting typical palisading of the nuclei. Recent study utilizing cellblock technique confirms that the lining epithelium in KCOT shows parakeratination7. Additionally, diffuse and focal epithelial hyperplasia, epithelial budding, reactive cytological alterations, dystrophic calcification, daughter cysts, odontogenic epithelial remnants and ameloblastomatous epithelium could also be noted in KCOT8.
It is generally conceived that KCOTs have their origin in the epithelial remnants of dental lamina9. The usual occurrence of KCOT in the posterior mandible, the increased activity of dental lamina in this region and the ability of dental lamina to keratinize support this concept. Likewise, OOC being intraosseous, having a predilection for posterior mandible where the lining epithelium keratinizes, suggests that OOC may also originate from dental lamina and its remnants. The differences in its histological presentation and contrastingly differing behavior, however, raise a few questions about its histogenesis. All the features that typify an OOC were present in the reported case. The less aggressive nature of OOC seems to correlate with its pattern of cell proliferation and differentiation in their epithelial lining, which differ greatly from KCOT.
Several studies have been carried out using specific markers to underline the differences in their origin and pathogenesis. Dong et al.10 and da Silva et al.11 suggested that OOCs showed fully differentiated, mature keratinocytes, while KCOTs lacked mature keratinocytes. Also, OOCs showed a pattern of normal cellular differentiation, while KCOTs showed certain alterations in the differentiation process. With regard to the capsular tissue, OOCs seemed to be more stable than the KCOT.
A study reported by Aragaki et al.12 on keratin (K) expression in KCOT and OOC, revealed a differential expression between the two. OOC was positive for K1, K10 and Loricrin (LOR), while KCOT was negative for all the three, thus suggesting that keratin profile in OOC was identical to that of epidermis. On the contrary, K4, K13 and K17 expression was strongly positive in KCOT, but negative in OOC, further reiterating that the keratin profile in KCOT was similar to dental lamina. This study, however, did not support the origin of OOC in dental lamina, unlike KCOT. The results of this study also indicated that KCOT and OOC expressed unique sets of keratin subtypes, suggesting that each is a distinct entity and deserve to be treated as two separate jaw cysts of odontogenic origin. Positive expression of K2 and LOR in OOC indicated that the cells were in a completely differentiated state, and thus not aggressive in its behavior.
The most perplexing aspect of OOC is its characteristic attachment to the neck of the tooth, quite similar to a dentigerous cyst (DC), as was noted in this case. As the clinicoradiographic diagnosis of any circumscribed radiolucency around the crown of an impacted tooth is usually a dentigerous cyst, it was not different in present case as well. As the microscopic examination of the cyst fitted well in favor of orthokeratinized odontogenic cyst, the possibility of considering this as a DC with a lining epithelium with keratinization was considered. The attachment of the cystic lining to the neck of the tooth also prompted to contemplate the origin in reduced enamel epithelium. Comparison of orthokeratinized odontogenic cyst with the dentigerous cyst and KCOT was done based on the available literature, to rule out any likeliness of OOC being the orthokeratinized variant of a dentigerous cyst. A table showing the cytokeratin (CK) expression in all the three closely resembling cysts is presented (Table 1).
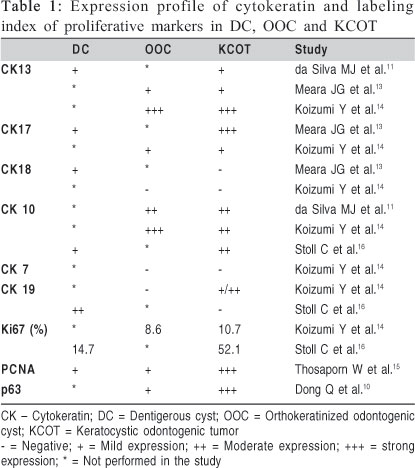
Compilation of these data revealed a considerable overlap in cytokeratin expression. CK 10 and CK17 which is typically expressed in a keratinized epithelium were negative or weakly expressed in dentigerous cyst and moderately or strongly expressed in OOC and KCOT. On the other hand, CK 18 and 19, which are the markers of non-keratinized epithelium, were positive in dentigerous cyst and negative in both OOC and KCOT. With regard to the markers of the odontogenic epithelium of dental lamina and enamel organ, namely CK 7 and CK 13, dentigerous cyst expressed both weakly, OOC expressed CK 7 negatively and CK 13 strongly positive and KCOT expressed CK7 weakly and CK13 strongly positive. This implied that OOC and KCOT might have a common origin in the rests of dental lamina. Despite extensive research on CK expression in these three developmental odontogenic cysts, nothing concrete could be elucidated, as the results were often confounding. This has left the investigators clueless about the definitive cell of origin in the histogenesis of any of the developmental odontogenic cysts.
Results like these have opened the perspectives for the study of other molecular markers of proliferation and prognosis, the most commonly evaluated being p63 and Ki-67 (Table 1). Studies with these antigens suggested that KCOT is by far the most aggressive of the three and OOC, unlike KCOT, may not progress to malignancy. Amaral et al.17 compared the proliferative index (PI) and apoptotic index (AI) between KCOT and ameloblastoma. It was observed that the PI of KCOT was higher than that of ameloblastoma, though no significant difference in AI was observed among the two lesions. According to study by Nadalin et al.18, Ki-67 expression in the suprabasal layer of KCOT correlated positively with the expression and intensity of syndecan-1, supporting the previous studies proving that KCOT is highly proliferative. Another study by Goncalves et al.19 also confirmed these observations in KCOT.
It is perhaps for this reason that the surgical management of OOC is more conservative. Treatment of KCOT remains controversial, and the management modalities can be categorized as either conservative or aggressive20, based on multiple factors including lesion size, anatomic relationship, recurrence pattern, and the cyst's association with NBCCS21. Multiple surgical protocols have been employed in the management of KCOT, which include marsupialization, enucleation, application of Carnoy's solution following enucleation, decompression, marginal or radical surgical resection, and bone implantation22. However, OOC being less aggressive than KCOT is treated conservatively by mere enucleation of the cyst2. Removal of entire cystic lining along with the extraction of impacted tooth is the principal treatment modality in OOC. However, if an erupting tooth must be preserved, conservative treatment should be the treatment of choice23.
Although these three closely related odontogenic cysts may seem to have a common odontogenic origin, the pathogenesis and progression of each one of these is distinct. Use of specific markers of odontogenic epithelium at varying stages of differentiation to rule out a possible odontogenic origin would be the first crucial step. Secondly, since OOC expresses cytokeratins, which are primarily expressed in epidermis, sequestration of the stomadial ectoderm into the developing jaw during embryogenesis is possible. Consideration of OOC as an intraosseous counterpart of epidermoid cyst within the jawbone needs to be addressed24. Clinically and radiographically, both the OOC and intraosseous epidermoid cyst present as hard, progressively growing non-tender enlargement, with a well-defined radiolucency. Likewise, histopathological features of OOC overlap with epidermoid cyst, although the former is usually devoid of skin appendages25. However, observations of Zhang et al.26 showed no significant histological differences between OOC and epidermoid cyst. With few reported cases of intraosseous epidermoid cysts in the maxillofacial region27-28, an intraosseous epidermoid cyst is necessarily a closely related entity, which needs to be considered as a differential diagnosis for OOC.
OOC has been considered as the developmental odontogenic cyst. The exclusivity of this case is the attachment of the cystic lining to the cementoenamel junction, which gave an initial notion of dentigerous cyst. With the support of the literature, it was attempted to untangle the mystery of OOC with regard to its nature and origin. These studies have opened new perspectives, as understanding the pathogenesis of OOC is yet to be unraveled. Due to the overlapping disposition of the reviews and reports, the final conclusion is inscrutable. Digression of thoughts from odontogenic origin of this cyst to the inclusional origin can enlighten the source and pathogenesis of OOC and can help in accurate treatment planning.
References
1. Schultz L. Cysts of maxilla and mandible. J Am Dent Assoc. 1927; 14: 1395-1402. [ Links ]
2. Li TJ, Kitano M, Chen XM, Itoh T, Kawashima K, Sugihara K et al. Orthokeratinized odontogenic cyst: a clinicopathological and immunohistochemical study of 15 cases. Histopathology. 1998; 32: 242-51. [ Links ]
3. Yoshida H, Onizawa K, Yusa H. Squamous cell carcinoma arising in association with an orthokeratinized odontogenic keratocyst. Report of a case. J Oral Maxillofac Surg. 1996; 54: 647-51. [ Links ]
4. de Fatima BV, de Lacerda JC, de Aguiar MC, Gomez RS. Calcifying odontogenic cyst associated with an orthokeratinized odontogenic cyst. Head Neck Pathol. 2008; 2: 324-7. [ Links ]
5. Fregnani ER, Da Cruz Perez DE, Soares FA, Alves FA Synchronous ameloblastoma and orthokeratinized odontogenic cyst of the mandible. J Oral Pathol Med. 2006; 35: 573-25. [ Links ]
6. Ide F, Saito I, Horie N, Shimoyama T. Orthokeratinized odontogenic cyst of the mandible with heterotopic cartilage. Head Face Med. 2009; 3: 150-2. [ Links ]
7. Oenning ACC, Rivero ERC, Calvo MCM, Meurer, Grando LJ. Braz Oral Res. 2012; 26: 355-9. [ Links ]
8. Azevedo RS, Cabral MG, Santos TCRBD, de Oliveira AV, de Almeida OP, Pires FR. Histopathological features of odontogenic tumor: A descriptive study of 177 cases from a Brazilian population. Int J Surg Pathol. 2012; 20: 154-60. [ Links ]
9. Browne RM. The odontogenic keratocyst. Histological features and their correlation with clinical behavior. Br Dent J. 1971; 131: 249-59. [ Links ]
10. Dong Q, Pan S, Sun LS, Li TJ. Orthokeratinized odontogenic cyst: a Clinicopathologic study of 61 cases. Arch Pathol Lab Med. 2010; 134: 271-5. [ Links ]
11. da Silva MJ, de Sousa SO, Correa L, Carvalhosa AA, de Araujo VC. Immunohistochemical study of the orthokeratinized odontogenic cyst: a comparison with the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Radiol Endod. 2002; 94: 732-7. [ Links ]
12. Agaraki T, Michi Y, Katsube K, Uzawa N, Okada N, Akashi T et al. Comprehensive keratin profiling reveals different histopathogenesis of keratocystic odontogenic tumour and orthokeratinized odontogenic cyst. Hum Pathol. 2010; 41: 1718-25. [ Links ]
13. Meara JG, Pilch BZ, Shah SS, Cunningham MJ. Cytokeratin expression in the odontogenic keratocyst. J Oral Maxillofac Surg. 2000; 58: 862-6. [ Links ]
14. Koizumi Y. Odontogenic keratocyst, orthokeratinized odontogenic cyst and epidermal cyst: an immunohistochemical study including markers of proliferation, cytokeratin and apoptosis related factors. Int J Oral-Med Sci. 2004; 2: 14-22. [ Links ]
15. Thosaporn W, lamaroon A, Pongsiriwet S, Ng KH. A comparative study of epithelial cell proliferation between the odontogenic keratocyst, orthokeratinized odontogenic cyst, dentigerous cyst and ameloblastoma. Oral Dis. 2004; 10: 22-6. [ Links ]
16. Stoll C. Stollenwerk C, Riediger D, Mittermayer C, Alfer J. Cytokeratin expression patterns for distinction of odontogenic keratocysts from dentigerous and radicular cysts. J Oral Pathol Med. 2005; 34: 558-64. [ Links ]
17. Amaral FR, Mateus GCP, Bonisson LA, de Andrade BAB, Mesquita RA, Horta MCR, et al. Cell proliferation and apoptosis in ameloblastomas and keratocystic tumors. Braz Dent J. 2012; 23: 91-6. [ Links ]
18. Nadalin MR, Fregnani ER, Silva-Sousa YRC, Perez DE. Syndecan-1 (CD138) and Ki-67 expression in odontogenic cystic lesions. Braz Dent J. 2011; 22: 223-9. [ Links ]
19. Goncalves CK, Fregnani ER, Leon JE, Silva-Sousa YRC, Perez DE. Immunohistochemical expression of p63, epidermal growth factor receptor (EGFR) and notch-1 in radicular cysts, dentigerous cysts and keratocystic odontogenic tumors. Braz Dent J. 2012; 23: 337-43. [ Links ]
20. Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005; 63: 635-9. [ Links ]
21. Madras J, Lapointe H. Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc. 2008; 74: 165-165h. [ Links ]
22. Zhao YF, Wei JX, Wang SP. Treatment of odontogenic keratocysts: a follow-up of 255 Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94: 151-6. [ Links ]
23. Deboni MCZ, Brozoski MA, Traina AA, Acay RR, Naclerio-Homem M. Surgical management of dentigerous cyst and keratocystic odontogenic tumor in children: a conservative approach and 7-year follow-up. J Appl Oral Sci. 2012; 20: 268-71. [ Links ]
24. Vuhahula E, Nikai H, Ijuhin N, Ogawa I, Takata T, Koseki T, et al. Jaw cysts with orthokeratinization: analysis of 12 cases. J Oral Pathol Med. 1993; 22: 35-40. [ Links ]
25. Allon DM, Calderon S, Kaplan I. Intraosseous compound-type dermoid cyst of the jaw. Int J Head Neck Surg. 2010; 1: 103-6. [ Links ]
26. Zhang JY, Dong Q, Li TJ. Int J Oral Maxillofac Surg. 2011; 40: 1296-300. [ Links ]
27. Montebugnoli L, Tiberio C, Venturi M. A rare case of congenital epidermoid cyst of hard palate. BMJ Case Rep. 2011; 4485: 1-4. [ Links ]
28. Singh V, Gupta S, Jaiswal R, Malkunje L. Intra osseous dermoid cyst of mandible - a rare case report. Open journal of stomatology. 2012; 2: 153-6. [ Links ]
 Correspondence:
Correspondence:
Raghu Radhakrishnan
Department of Oral Pathology
Manipal College of Dental Sciences
Manipal University, Manipal, 576 104, India
Phone: +91 820 2922204
Fax: +91 820 2571966
E-mail: raghu.radhakrishnan@gmail.com
Received for publication: October 15, 2012
Accepted: December 14, 2012













