Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.2 Piracicaba Abr./Jun. 2013
ORIGINAL ARTICLE
Could idiopathic osteosclerosis have correlations with palatally impacted maxillary canines?
Cesar Augusto Rodenbusch PolettoI; Claudinéia ItiberêII; Sérgio Aparecido IgnácioIII; Lucilia KurikiIV; Orlando Motohiro TanakaIV; Elisa CamargoIV
IArea of Orthodontics and Radiology, University of Planalto Catarinense (UNIPLAC), Lages, SC, Brazil and Pontifical Catholic University of Paraná (PUCPR), Curitiba, PR, Brazil
IIDentist, Curitiba, PR, Brazil
IIIArea of Biostatistics, Dental School, Pontifical Catholic University of Paraná (PUCPR), Curitiba, PR, Brazil
IVArea of Orthodontics, Dental School, Pontifical Catholic University of Paraná (PUCPR), Curitiba, PR, Brazil
ABSTRACT
AIM: To investigate the association between palatally impacted maxillary canines (PIC) and idiopathic osteosclerosis.
METHODS: A sample of 54 subjects (28 females and 26 males, mean age of 12.98±1.59 years) with PIC was selected from the records of 1,650 orthodontic patients treated at the Discipline of Orthodontics clinics at the Dental School of the Pontifical Catholic University of Paraná (PUCPR), in Curitiba, PR, Brazil. A control group of 54 subjects with normally erupted canines was also selected from the same files (mean age of 12.93±1.58 years). Panoramic, lateral skull, postero-anterior skull, periapical and occlusal radiographs, as well as stone casts of the patients were examined. The Kolmogorov-Smirnov test revealed a normal distribution of gender and age in the groups. The results were analyzed with the Chi-square test (α=0.05).
RESULTS: There were no statistically significant differences (p>0.05) between the groups. Four patients from each group had idiopathic osteosclerosis (7.41%), a rate that falls in the prevalence range reported in the literature.
CONCLUSIONS: No correlation was observed between palatally impacted maxillary canines and idiopathic osteosclerosis.
Keywords: diagnosis, tooth, unerupted, osteosclerosis.
Introduction
Idiopathic osteosclerosis is an asymptomatic, non-expansive and localized increase of bone radiopacity caused by an increase in the width of the bone trabeculae at the expense of medullary space. It is usually located in the mandibular premolar region1-3. The lesion has benign characteristics and seems not to increase over time4.
Peck5 listed several dental anomalies that seemed to indicate a pattern. Among them were missing teeth, conoid teeth, teeth with reduced size (generalized or localized), delayed tooth formation and eruption (generalized or localized), infraocclusion (more frequently in primary teeth), palatally impacted canines, maxillarycanine/premolar transposition, mandibular canine/lateral incisor transposition, and distal angulation of a non-erupted second mandibular premolar. According to this author, other associations will be discovered as researchers focus on the genetic pattern of these anomalies.
After the third molars, the permanent maxillary canine is the most frequently involved tooth in cases of impaction6-7. Palatally impacted maxillary canines seem connected to a genetic condition, and are often associated with other dental and skeletal disturbances7.
The aim of the present study was to investigate whether an increased prevalence of idiopathic osteosclerosis exists in patients with palatally impacted maxillary canines.
Material and methods
A total of 1,650 patient records from the files of the Discipline of Orthodontics of the Dental School of the Pontifical Catholic University of Paraná (PUCPR) were reviewed for this study. The Experimental Group (EG) consisted of 54 (3.27%) patients who presented 62 palatally impacted maxillary canines; these patients had ages starting at 12 years and 5 months to ensure a definite diagnosis of palatal impaction. According to Ericson and Kurol8, the best age to establish a clinical diagnosis of maxillary canine impaction using digital palpation and checking for the presence of a buccal bulge would be starting at 9 years because the clinical signs are not evident before this age. As for gender, 28 cases were observed among females (51.85%) and 26 among males (48.15%).
The Control Group (CG) consisted of 54 patients, 28 females and 26 males, with approximately the same age (12.93±1.58 years) as those of the patients in the EG (12.98±1.59 years), with normally erupted canines. The Kolmogorov-Smirnov test indicated normal distribution of gender and age in the groups.
The patients’ orthodontic documentation, which included a set of radiographs (panoramic, lateral skull, postero-anterior skull, periapical and occlusal), photographs and stone casts, was used for diagnosing the cases of palatally impacted maxillary canines. The methods were the three-dimensional localization using orthogonal radiographs and the Clark method. The canine was considered palatally impacted whenever it was unerupted and the patient was already in the C5 cervical maturation stage, as proposed by Baccetti9.
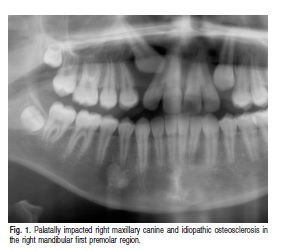
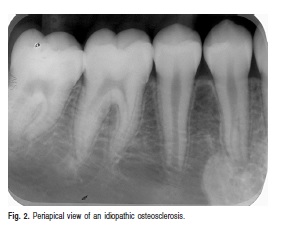
The diagnosis of idiopathic osteosclerosis was also established based on the patient’s radiographic examinations. Idiopathic osteosclerosis was observed as a bone radiopacity increase located inside the bone, measuring 3 mm or more, with no radiolucent halo and no apparent cause (Figures 1 and 2), as proposed by Langlais et al.1, and White and Pharoah3. Radiopaque lesions associated with dental caries, deep restorations or tooth extraction regions were not diagnosed as idiopathic osteosclerosis, since they could be the result of condensing osteitis or residual condensing osteitis, when located in a tooth extraction region. Lesionslocated in tooth extraction regions could also be the result of alveolar sclerosis. Exostoses of the torus type were excluded by evaluating the intraoral photographs and the gypsum casts of the orthodontic documentation. The projected image of a soft tissue calcification was discarded by analyzing the radiograph with a projection perpendicular to the panoramic radiograph or to the lateral skull radiograph, namely the posteroanterior skull radiograph.
Initially, canine impaction was assessed and idiopathic osteosclerosis was identified in 30 patient records (15 from the CG and 15 from the EG), at two time points (day zero and 30 days later), by a single radiology specialist, and by applying the Kappa agreement test. The test indicated agreement between the assessments (p<0.05), obtaining the lowest kappa value of 0.7830 (a value greater than 0.60 is recommended). All radiographs of both groups were then analyzed and the data were tabulated for application of the Chi-square statistical test (α=0.05).
Results
Four cases of osteosclerosis were observed in EG and 4 cases CG (7.41%). No significant correlation was found between osteosclerosis and either of the groups (p>0.05).
Discussion
One of the most important requisites for treating and preventing a disease is to know its etiologic factor. The term idiopathic has been used whenever science has failed to define the cause of a certain change. Nevertheless, pursuit for the origin goes on and nowadays several pathological conditions have been shown to have a genetic condition as a causal factor. Some changes overlap and often share the same origin. These associations may help in the early diagnosis of some serious disease as the Gardner syndrome, for example. One of its first manifestations in the oral cavity is the presence of osteomas in the maxillary bones. Later on, the patient develops malignant intestinal tumors that are hard to treat and have a more doubtful prognosis. A dentist on the alert may suspect a new case of Gardner syndrome by observing atypical osteoma-like lesions in a young patient and referring him/her to medical evaluation10.
Palatally impacted maxillary canines seem to have a genetic etiology6,11, and are frequently associated with other changes, such as microdontia of maxillary lateral incisors11-12, delayed tooth eruption13 and fusion of the clinoid processes of the sella turcica14. Idiopathic osteosclerosis is a bone tissue structural change whose etiologic factor remains unknown. It is also known as enostosis or dense bone island, terms used more frequently by medical literature to describe radiopaque lesions found occasionally, mostly in the long bones. Its most common location in the jaws is the mandible, mainly in the premolar and molar regions.
Although idiopathic osteosclerosis is not a rare entity, little importance has been given by orthodontists to its occurrence, as demonstrated by the small number of studies published on this topic in orthodontic journals. In a study on the incidental findings made on panoramic radiographs of orthodontic patients, Bondemark et al.15 observed that idiopathic osteosclerosis was the most frequent finding, outnumbering even periapical inflammatory lesions and marginal bone resorptions.
Diagnosing idiopathic osteosclerosis accurately is a difficult task, since this lesion may be radiographically mistaken for exostosis, including torus mandibularis and palatinus, residual condensing osteitis, alveolar calcification after exodontia (whether complicated or not), bone architectural change in response to occlusal trauma on an inclined tooth, particularly on mandibular second molars, when the first molars are missing. The lesion may even be mistaken for a radiographic projection over bone of a soft tissue calcification. The mere presence of teeth, their carious lesions, occlusal traumas and infectious processes, as well as the primary teeth shedding process, may also cause bone tissue architectural changes, adding to the abovementioned enostoses and dense bone islands.
The dentist’s approach towards idiopathic osteosclerosis is also not unanimous in the literature. Williams and Brooks4 followed adult patients with idiopathic osteosclerosis for a decade and concluded that it remained stable. McDonald-Jankowski2 studied idiopathic osteosclerosis lesions in radiographic examinations after a 9-year interval and found that lesion size may decrease and that that there may be complete remission in some cases. These findings reinforce the recommendation for no intervention.
There are, however, reports of complications arising from the presence of idiopathic osteosclerosis in the maxillary bones. Bennett and McLaughlin16 warned that bone sclerosis might delay or even obstruct space closure after tooth extractions during orthodontic treatment. Nakano et al.17 reported a case of tooth inclination caused by idiopathic osteosclerosis growth. Marques-Silva et al.18 described a case where idiopathic osteosclerosis caused deviation of a tooth eruption route. This, in turn, led to the resorption of the adjacent tooth. Mah et al.19 suggested that caution should be taken in biomechanical planning and orthodontic movement in sclerotic bone areas, and also that computerized tomography examination may aid in this planning.
Alveolar sclerosis is a condition histologically very similar to idiopathic osteosclerosis. Baumgaertel20 reported a very interesting case where the tooth movement process through an alveolus repaired with sclerotic bone was not possible using the conventional retraction technique, requiring extra anchorage obtained by means of mini-implants. The patient of that case also displayed agenesis of a maxillary lateral incisor and palatal impaction of a maxillary canine, both conditions that seem to share the same genetic origin.
Considering the possible difficulty in performing tooth movement when faced with a case of osteosclerosis, the orthodontist should register its presence on the patient’s records and follow the patient radiographically. If moving a tooth through the zone of osteosclerosis is required, caution must be taken during the procedure since the lesion may render tooth movement difficult.
To the best of our knowledge, no previous study has investigated the association between idiopathic osteosclerosis and palatally impacted permanent maxillary canines. A single study21 was found comparing the prevalence of this lesion in certain malocclusion types, although the criterion adopted by the authors for diagnosing malocclusion was based solely on the gypsum model records. The authors did not distinguished the skeletal from the dental aspects of the sagittal malocclusions, a distinction seemingly relevant when studying possible correlations between this malocclusion type and a bone lesion.
A possible association between a greater prevalence of idiopathic osteosclerosis among patients with palatally impacted maxillary canines could suggest that idiopathic osteosclerosis is a genetic condition and possibly also the manifestation of the complex condition of palatally impacted maxillary canines.
The prevalence of palatally impacted maxillary canines found in the present study (3.27%) and the prevalence ofidiopathic osteosclerosis (7.41%) were similar to those reported elsewhere22. Finding an identical number of idiopathic osteosclerosis cases in both groups suggests that there is no association of this condition with palatally impacted maxillary canines. Also, the small number of idiopathic osteosclerosis cases observed in this study may have interfered with establishing a possible association. Further investigation is required with a greater sample of patients to effectively discard an association between the two pathologies or possibly demonstrate a common genetic origin. The results showed no correlation between palatally impacted maxillary canines and idiopathic osteosclerosis.
References
1. Anic-Milosevic S, Varga S, Mestrovic S Lapter-Varga M, Slaj M. Dental and occlusal features in patients with palatally displaced maxillary canines. Eur J Orthod. 2009; 31: 367-73. [ Links ]
2. Baccetti T. Risk indicators and interceptive treatment alternatives for palatally displaced canines. Semin Orthod. 2010; 16: 186-92. [ Links ]
3. Bennett J C, Mclaughlin R P. Controlled space closure with preadjusted appliance system. J Clin Orthod. 1990; 4: 251-60. [ Links ]
4. Baumgaertel S. Socket sclerosis- An obstacle for orthodontic space closure? Angle Orthod. 2009; 79: 800-3. [ Links ]
5. Bishara S E. Impacted maxillary canines: A review. Am J Orthod Dentofac Orthop. 1992; 101: 159-71. [ Links ]
6. Bondemark L, Jeppsson M, Lindh-Ingildsen L, Rangne K. Incidental findings of pathology and abnormality in pretreatment orthodontic panoramic radiographs. Angle Orthod. 2006; 76: 76-98. [ Links ]
7. Cankaya AB, Erdem MA, Isler SC, Cifter M, Olgac V, Kasapoglu C, ET al. Oral and maxillofacial considerations in Gardner’s Syndrome. Int J Med Sci. 2012; 9: 137-41.
8. Chaushu S, Sharabi S, Becker A. Dental morphologic characteristics of normal versus delayed developing dentitions with palatally displaced canines. Am J Orthod Dentofacial Orthop. 2012; 121: 339-46. [ Links ]
9. Ericson S, Kurol J. Longitudinal study and analysis of clinical supervision of maxillary canine eruption. Community Dent Oral Epidemiol. 1986; 8: 133-40. [ Links ]
10. Garib DG, Alencar BM, Lauris JR, Baccetti T. Agenesis of maxillary lateral incisors and associated dental anomalies. Am J Orthod Dentofacial Orthop. 2010; 137: 732-6. [ Links ]
11. Jacoby H. The etiology of maxillary canine impaction. Am J Orthod Dentofacial Orthop. 1983; 84: 125-32. [ Links ]
12. Langlais RP, Langland OE, Nortjé CJ. Generalized radiopacities. In: Cooke D, editor. Diagnostic Imaging of the jaws. Baltimore: Williams& Wilkins; 1995. p.565-615. [ Links ]
13. Leonardi R, Barbato E, Vichi M, Caltabiano M. Skeletal anomalies and normal variants in patients with palatally displaced canines. Angle Orthod. 2009; 79: 727-32. [ Links ]
14. Marques-Silva L, Guimarães ALS, Dilascio MLC, Castro WH, Gomez RS. A rare complication of idiopathic osteosclerosis. Med Oral Patol Oral Cir Bucal 2007, 12: E233-4. [ Links ]
15. Mah JK, Yi L, Huang RC, Choo HR. Advanced applications of cone beam computed tomography in orthodontics. Semin Orthod. 2011; 17: 57-71. [ Links ]
16. Mcdonald-Jankowski D S. Idiopathic osteosclerosis in the jaws of Britons and of the Hong Kong Chinese: radiology and systematic review. Dentomaxillofac Radiol. 1999; 28: 357-63. [ Links ]
17. Nakano K, Ogawa T, Sobue S, Ooshima T. Dense bone island: clinical features and possible complications. Int J Paediatr Dent. 2001; 12: 433-7. [ Links ]
18. Peck S. Dental Anomaly Patterns (DAP): A new way to look at malocclusion. Angle Orthod. 2009; 19: 1015-6. [ Links ]
19. White SC, Pharoah MJ. Benign tumours of the jaws. In: White SC, Pharoah MJ. Oral radiology: principles and interpretation. Saint Louis: Mosby; 2000. p.378-419. [ Links ]
20. Williams TP, Brooks SL. A longitudinal study of idiopathic osteosclerosis and condensing osteitis. Dentomaxillofac Radiol. 1998; 27: 275-8. [ Links ]
21. Lee S,Park I, Jang I, Choi D, Cha B. A study on the prevalence of the idiopathic osteosclerosis in Korean malocclusion patients. Korean J Oral Maxillofac Radiol. 2010; 40: 159-63. [ Links ]
22. Sisman Y, Ertas ET, Ertas H, Sekerci AE. The frequency and distribution of idiopathic osteosclerosis of the jaws. Eur J Dent. 2001; 5: 409-15. [ Links ]
 Correspondence:
Correspondence:
Cesar Augusto Rodenbusch Poletto
Rua Rubens de Almeida, 75,
CEP: 88523-180 - Lages, SC, Brasil
E-mail: cesarpoletto2@gmail.com













